Abstract
Purpose
Dent disease (DD) is a rare tubulopathy characterized by proximal tubular dysfunction leading to chronic kidney disease (CKD). The aim of the study was to characterize patients with DD in Poland.
Methods
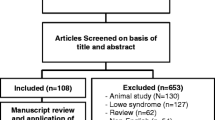
A retrospective analysis of a national cohort with genetically confirmed diagnosis.
Results
Of 24 males, all patients except one carried mutations in the CLCN5 gene; in one patient a mutation in the OCRL gene was disclosed. Molecular diagnosis was delayed 1 year on average (range 0–21 years). The most common features were tubular proteinuria (100%), hypercalciuria (87%), and nephrocalcinosis (56%). CKD (≤stage II) and growth deficiency were found in 45 and 22% of patients, respectively. Over time, a progression of CKD and persistence of growth impairment was noted. Subnephrotic and nephrotic proteinuria (20%) was found in most patients, but tubular proteinuria was assessed in only 67% of patients. In one family steroid-resistant nephrotic syndrome prompted a genetic testing, and reverse phenotyping. Five children (20%) underwent kidney biopsy, and two of them were treated with immunosuppressants. Hydrochlorothiazide and angiotensin-converting enzyme inhibitors were prescribed for a significant proportion of patients (42 and 37.5%, respectively), while supplemental therapy with phosphate, potassium, vitamin D (12.5% each), and alkali (4.2%) was insufficient, when compared to the percentages of patients requiring repletion.
Conclusions
We found CLCN5 mutations in the vast majority of Polish patients with DD. Proteinuria was the most constant finding; however, tubular proteins were not assessed commonly, likely leading to delayed molecular diagnosis and misdiagnosis in some patients. More consideration should be given to optimize the therapy.



Similar content being viewed by others
References
Blanchard A, Curis E, Guyon-Roger T et al (2016) Observations of a large Dent disease cohort. Kidney Int 90(2):430–439
Hoopes RR, Raja KM, Koich A et al (2004) Evidence for genetic heterogeneity in Dent’s disease. Kidney Int 65:1615–1620
Mansour-Hendili L, Blanchard A, Pottier NL et al (2015) Mutation update of the CLCN5 gene responsible for Dent disease 1. Hum Mutat 36:743–752
Hichri H, Rendu J, Monnier N et al (2011) From Lowe syndrome to Dent disease: correlations between mutations of the OCRL1 gene and clinical and biochemical phenotypes. Hum Mutat 32:379–388
Zaniew M, Bökenkamp A, Kołbuc M et al (2016) Long-term renal outcome in children with OCRL mutations: retrospective analysis of a large international cohort. Nephrol Dial Transplant. doi:10.1093/ndt/gfw350
Recker F, Zaniew M , Böckenhauer D et al (2015) Characterization of 28 novel patients expands the mutational and phenotypic spectrum of Lowe syndrome. Pediatr Nephrol 30(6):931–943
Bökenkamp A, Cheong HI, Hoppe B et al (2009) Dent-2 disease: a mild variant of Lowe syndrome. J Pediatr 155:94–99
Sekine T, Komoda F, Miura K et al (2014) Japanese Dent disease has a wider clinical spectrum than Dent disease in Europe/USA: genetic and clinical studies of 86 unrelated patients with low-molecular-weight proteinuria. Nephrol Dial Transplant 29(2):376–384
Akuta N, Lloyd SE, Igarashi T et al (1997) Mutations of CLCN5 in Japanese children with idiopathic low molecular weight proteinuria, hypercalciuria and nephrocalcinosis. Kidney Int 52:911–916
Copelovitch L, Nash MA, Kaplan BS (2007) Hypothesis: Dent disease is an underrecognized cause of focal glomerulosclerosis. Clin J Am Soc Nephrol 2:914–918
Frishberg Y, Dinour D, Belostotsky R et al (2009) Dent’s disease manifesting as focal glomerulosclerosis: is it the tip of the iceberg? Pediatr Nephrol 24:2369–2373
Wang X, Anglani F, Beara-Lasic L et al (2016) Glomerular pathology in Dent disease and its association with kidney function. Clin J Am Soc Nephrol 11(12):2168–2176
Van Berkel Y, Ludwig M, van Wijk JA, Bökenkamp A (2016) Proteinuria in Dent disease: a review of the literature. Pediatr Nephrol. doi:10.1007/s00467-016-3499-x
Szczepanska M, Zaniew M, Recker F et al (2015) Dent disease in children: diagnostic and therapeutic considerations. Clin Nephrol 84(4):222–230
Utsch B, Bökenkamp A, Benz MR et al (2006) Novel OCRL1 mutations in patients with the phenotype of Dent disease. Am J Kidney Dis 48:942–954
Schwartz GJ, Muñoz A, Schneider MF et al (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637
Levey AS, Coresh J, Greene T et al (2006) Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med 145:247–254
National Kidney Foundation (2002) K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 39:S1–S266
Heilbron DC, Holliday MA, Al-Dahwi A, Kogan BA (1991) Expressing glomerular filtration rate in children. Pediatr Nephrol 5:5–11
Tanuma A, Sato H, Takeda T et al (2007) Functional characterization of a novel missense CLCN5 mutation causing alterations in proximal tubular endocytic machinery in Dent’s disease. Nephron Physiol 107:87–97
Grand T, Mordasini D, L’Hoste S et al (2009) Novel CLCN5 mutations in patients with Dent’s disease result in altered ion currents or impaired exchanger processing. Kidney Int 76:999–1005
D’Antonio C, Molinski S, Ahmadi S, Huan LJ, Wellhauser L, Bear CE (2013) Conformational defects underlie proteasomal degradation of Dent’s disease-causing mutants of ClC-5. Biochem J 452:391–400
Böckenhauer D, Bökenkamp A, Nuutinen M et al (2012) Novel OCRL mutations in patients withDent-2 disease. J Pediatr Genet 1:15–23
Cho HY, Lee BH, Choi HJ, Ha IS, Choi Y, Cheong HI (2008) Renal manifestations of Dent disease and Lowe syndrome. Pediatr Nephrol 23:243–249
Edvardsson VO, Goldfarb DS, Lieske JC et al (2013) Hereditary causes of kidney stones and chronic kidney disease. Pediatr Nephrol 28(10):1923–1942
Klootwijk ED, Reichold M, Unwin RJ, Kleta R, Warth R, Bockehauer D (2015) Renal Fanconi syndrome: taking a proximal look at the nephron. Nephol Dial Transplant 30(9):1456–1460
Ludwig M, Levtchenko E, Bökenkamp A (2014) Clinical utility gene card for: Dent disease (Dent-1 and Dent-2). Eur J Hum Genet 22(11):1338
Levtchenko E, Bökenkamp A, Monnens L, Ludwig M. Dent’s disease. In: Sahay M (ed) Diseases of renal parenchyme. InTech—Open Access Publisher, Croatia pp 17–32. ISBN: 978-953-51-0245-8
Ludwig M, Utsch B, Balluch B, Frund S, Kuwertz-Broking E, Bökenkamp A (2006) Hypercalciuria in patients with CLCN5 mutations. Pediatr Nephrol 21:1241–1250
Lipska BS, Iatropoulos P, Maranta R et al (2013) Genetic screening in adolescents with steroid-resistant nephrotic syndrome. Kidney Int 84(1):206–213
Raja KA, Schurman S, D’Mello RG et al (2002) Responsiveness of hypercalciuria to thiazide in Dent’s disease. J Am Soc Nephrol 13:2938–2944
Blanchard A, Vargas-Poussou R, Peyrard S et al (2008) Effect of hydrochlorothiazide on urinary calcium excretion in Dent disease: an uncontrolled trial. Am J Kidney Dis 52:1084–1095
Gambaro G, Croppi E, Coe F et al (2016) Metabolic diagnosis and medical prevention of calcium nephrolithiasis and its systemic manifestations: a consensus statement. J Nephrol 29(6):715–734
Alon US (2009) Medical treatment of pediatric urolithiasis. Pediatr Nephrol 24(11):2129–2135
Krieger NS, Asplin JR, Frick KK et al (2015) Effect of potassium citrate on calcium phosphate stones in a model of hypercalciuria. J Am Soc Nephrol 26(12):3001–3008
Cebotaru V, Kaul S, Devuyst O et al (2005) High citrate diet delays progression of renal insufficiency in the ClC-5 knockout mouse model of Dent’s disease. Kidney Int 68:642–652
Philips R, Hanchanale VS, Myatt A, Somani B, Nabi G, Biyani CS (2015) Citrate salts for preventing and treating calcium containing kidney stones in adults. Cochrane Database Syst Rev 10:CD010057
Acknowledgements
We are grateful to the patients and their parents for their invaluable contributions. We thank the Polish Registry of Inherited Tubulopathies (POLtube) and all physicians (listed below), who helped with patient recruitment and contributed with data of their patients. Danuta Zwolińska (Department of Pediatric Nephrology, Wrocław Medical University, Wrocław), Anna Moczulska (Department of Pediatric Nephrology, Kraków), Anna Niemirska, Dariusz Runowski (Department of Nephrology & Kidney Transplantation, The Children’s Memorial Health Institute, Warsaw), Hanna Szymanik-Grzelak (Department of Pediatrics and Nephrology, Medical University of Warsaw, Warsaw), Anna Wasilewska (Department of Pediatrics and Nephrology, Medical University, Białystok) all from Poland, and Franz Schaefer (Division of Paediatric Nephrology, Centre for Pediatric and Adolescent Medicine, Heidelberg, Germany). Part of the research leading to these results (F19 family testing) has received funding from the European Community’s Seventh Framework Programme (FP7/2007-2013) under grant agreement no. 2012-305608 (EURenOmics) and from Bundesministerium für Bildung und Forschung (BMBF) through the e-Rare initiative (PodoNet).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All other authors have declared no competing interests.
Rights and permissions
About this article
Cite this article
Zaniew, M., Mizerska-Wasiak, M., Załuska-Leśniewska, I. et al. Dent disease in Poland: what we have learned so far?. Int Urol Nephrol 49, 2005–2017 (2017). https://doi.org/10.1007/s11255-017-1676-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-017-1676-x