Abstract
Purpose
Adequate and functional long-term vascular access (VA) is pivotal for the efficient hemodialysis (HD). It has been shown that the most reliable VA is autogenous arteriovenous fistulas (AVFs) as compared with arteriovenous grafts (AVGs) and vascular catheters (VCs). The vascular access register (VAR) has been established since 2010, and the 4-year trend of VA in Serbia is presented in this paper.
Methods
All HD centers in Serbia provided their data by fulfilling the questionnaire that included prevalent and incident HD patients on December 31, 2010–1013.
Results
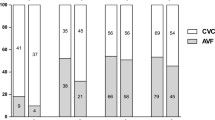
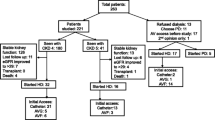
AVF is the most frequent prevalent VA (89.5–93.1 %) and also the most frequent newly created VA (87–89 %) during the observational period. The number of preemptive AVF is increasing, but it is still low (7.8 % in 2010 and 14.6 % in 2013). The percentage of incident AVG is constant (~3.4 %) as well as the number of permanent VC (8.2 % in 2010 and 7.8 % in 2013). The number of incident patients who started HD with AVF is decreasing (from 37 to 27 %), and the number of urgent start with VC is on the increase (from 63 to 73 %). In almost all relevant dialysis centers, vascular access is created by surgeons. Temporal VCs are placed by anesthesiologists (all centers), nephrologists (up to 25 % of centers) and vascular surgeons (up to 20 %). VCs are located mainly in jugular vein, but the number of femoral catheters remains high (up to 69 %).
Conclusion
Although we have favorable data, the VAR is of a great importance and ensures continuous quality improvement.




Similar content being viewed by others
References
Ng Y-Y, We S-C, Hung Y-N, Ko P-J (2009) Effect of demographic characteristics and timing of vascular access maturation on patency in Chinese incident haemodialysis patients. Nephrol Dial Transplant 24(11):3447–3453
Vascular Access 2006 Work Group (2006) Clinical practice guidelines for vascular access. Am J Kidney Dis 48(Suppl 1):S176–S247
Zangan SM, Falk A (2009) Optimizing arteriovenous fistula maturation. Semin Interv Radiol 26(2):144–150
The AV fistula first breakthrough initiative coalition: arteriovenous fistula first website. http://www.fistulafirst.org. About fistula first, fistula first catheter last (FF/CL) data, July 2003–April 2012 graphs, graphs of prevalent AV fistula use rates, by network. Accessed 9 Sept 2013
Jindal K, Chan CT, Deziel C, Hirsch D, Soroka SD, Tonelli M, Culleton BF, Canadian Society of Nephrology Committee for Clinical Practice Guidelines (2006) Hemodialysis clinical practice guidelines for the Canadian Society of Nephrology. J Am Soc Nephrol 17(3 Suppl 1):S1–S27
National Kidney Foundation (2006) Clinical practice guidelines for vascular access. Am J Kidney Dis 48(Suppl 1):S176–S247
Pisoni RL, Zepel L, Port FK, Robinson BM (2015) Trends in US vascular access use, patient preferences, and related practices: an update from the US DOPPS practice monitor with international comparisons. Am J Kidney Dis 65(6):905–915
Yearly report on renal replacement therapy in Serbia, 2013: Annual report on vascular access for hemodialysis in Serbia, 2013. http://www.udruzenjenefrologa.com/en/registry-andrecommendations/. Accessed 13 Feb 2016
Malovrh M (2015) Vascular access creation and care should be provided by nephrologists. J Vasc Access 16(Suppl 9):S20–S23
Ravani P, Marcelli D, Malberti F (2002) Vascular access surgery managed by renal physicians: the choice of native arteriovenous fistulas for hemodialysis. Am J Kidney Dis 40(6):1264–1276
Konner K, Hulbert-Shearon TE, Roys EC, Port FK (2002) Tailoring the initial vascular access for dialysis patients. Kidney Int 62(1):329–338
Mishler R (2009) Autologous arteriovenous fistula creation by nephrologists. Adv Chronic Kidney Dis 16(5):321–328
Noordzij M, Jager K, van der Veer S, Kramar K, Collart F, Heaf JG, Stojceva-Taneva O, Leivestad T, Buturovic-Ponikvar J, Benitez Sanchez M, Moreso F, Prutc KG, Severn A, Wanner C, Vanholder R, Ravani P (2014) Use of vasculat access for hemodialysis in Europe: a report from the ERA EDTA registry. Nephrol Dial Transplant 29:1956–1964
Stojceva-Taneva O, Selim G (2014) Vascular access in hemodialysis patients—registry data. Hippokratia 18(3):209–211
Ravani P, Gillespie BW, Quinn RR, MacRae J, Manns B, Mendelssohn D, Tonelli M, Hemmelgarn B, James M, Pannu N, Robinson BM, Zhang X, Pisoni R et al (2013) Temporal risk profile for infectious and noninfectious complications of hemodialysis access. J Am Soc Nephrol 24:1668–1677
The AV Fistula first breakthrough initiative coalition: arteriovenous fistula first website, 2015. http://www.fistulafirst.org.FFCL-Dashboard-Jun2014.xlsx. Accessed 23 Dec 2015
van der Veer SN, Ravani P, Coentrão L, Fluck R, Kleophas W, Labriola L, Hoischen SH, Noordzij M, Jager KJ, van Biesen W (2015) Barriers to adopting a fistula-first policy in Europe: an international survey among national experts. J Vasc Access 16(2):113–119
Roca-Tey R, Arcos E, Comas J, Cao H, Tort J, Registre de Malalts Renals de Catalunya (RMRC), Organització Catalana de Trasplantaments (OCATT), Health Department of Catalonia, Catalonia—Spain (2015) Vascular access for incident hemodialysis patients in Catalonia: analysis of data from the Catalan renal registry (2000–2011). J Vasc Access 16(6):472–479
Vascular Access Society, home page, guidelines, 10. Central venous access, Guidelines 10.3. http://wwwvascularaccesssociety.com/intro/guidelines. Accessed 20 Aug 2015
Tordoir J, Canaud B, Haage P, Konner K, Basci A, Fouque D, Kooman J, Martin-Malo A, Pedrini L, co Pizzarelli F, Tattersall J, Vennegoor M, Wanner C, ter Wee P, Vanholder R (2007) EBPG on vascular access. Guideline 10.3 Central venous access. Nephrol Dial Transplant 22(Suppl 2):112–113
Goodkin DA, Pisoni RL, Locatelli F, Port FK, Saran R (2010) Hemodialysis vascular access training and practices are key to improved access outcomes. Am J Kidney Dis 56(6):1032–1042
Acknowledgments
We kindly acknowledge colleagues from the Serbian HD Centers contributing to the study (in alphabetical order): Andric Branislav, Antic Miodrag, Aracki Snezana, Arsenovic Aleksandra, Berto Sabo Anika, Bogdanovic Jasmina, Cekovic Biljana, Cuckovic Cedomir, Cukic Zoran, Cveticanin Anica, Djordjevic Verica, Dudic Svetlana, Gajic Snezana, Gojakovic Biljana, Golubovic Predrag, Gucic Ljubinka, Hadzibulic Edvin, Hadzifejzovic Mersada, Hamzagic Nedim, Haviza-Lilic Branimir, Ilic Mira, Ilic Nasta, Jelacic Rosa, Kostic Mirjana, Kovacevic Miodrag, Lazarevic Tatjana, Markovic Rodoljub, Micunovic Vesna, Milenkovic Olgica, Milenkovic Radomir, Milenkovic Srboljub, Milicevic Biserka, Milicevic Olivera, Nikolic Zora, Obrenovic Slavica, Orescanin Mira, Pavlovic Stevan, Pesic Snezana, Petkovic Dobrila, Pilipovic Dragana, Prokopovic Miomir, Radovanovic Zoran, Rakic Nenad, Rangelov Vanja, Sefer Kornelija, Sibalic Simin Marija, Stefanovic Nikola, Stojanovic Dragoslav, Stojanovic Stanojevic Marina, Tirmenstajn Jankovic Biserka, Vasic Jovanovic Vesna, Vasilic Kokotovic Olivera, Vojinovic Goran, Vuckovic Dragana, Vukelic Vesna, Vukic Jasmina, Zagorac Nikola, Zec Nenad. Work on the vascular access register was promoted by the Serbian Society of Nephrology, and it could never have been carried out without their support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was not required for the purposes of this study as it was based upon anonymous patient data and did not involve patient intervention or the use of human tissue samples.
Additional information
An erratum to this article is available at http://dx.doi.org/10.1007/s11255-017-1511-4.
Rights and permissions
About this article
Cite this article
Jemcov, T., Dimkovic, N. Vascular access registry of Serbia: a 4-year experience. Int Urol Nephrol 49, 319–324 (2017). https://doi.org/10.1007/s11255-016-1378-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-016-1378-9