Abstract
Introduction
Electrocautery, harmonic scalpel tissue dissection and other surgical techniques can generate surgical smoke with high proportion of ‘fine particles’ (PM2.5) <2.5 μm, which is known to have adverse effects on human health. The high-risk zone for PM2.5 during surgeries by time and by distance has not been well evaluated.
Methods
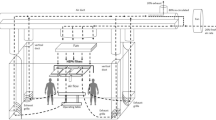
The study included open superficial, open abdominal, open pelvic, laparoscopic and transurethral urology surgeries, five of each. A particle counter was placed at three different distances from the incision site, and the real-time PM2.5 concentration was displayed after each cut. Air Quality Index (AQI) revised by the US Environmental Protection Agency and the calculated inhalation dose were used to evaluate the severity of PM2.5.
Results
In superficial, abdominal and pelvic surgeries, the peak PM2.5 concentration may reach 245.7, 149.4 and 165.1 μg/m3 3–6 s after a single cut 40 cm from the incision site. By the time, AQI usually turns to ‘unhealthy’ or ‘very unhealthy.’ In laparoscopic surgeries, 40 cm from the trocar, the air quality reached ‘hazardous’ in 3 s after opening of the trocar valve with a peak concentration of 517.5 μg/m3. In transurethral surgeries, the AQI 40 cm away from the resectoscope is generally at moderate level. In each surgery, the chief surgeon may inhale most of the PM2.5, while the assistant will inhale less than half the dose, and the scrub nurse may inhale nearly none. The use of wall suction may induce a 48–65 % decrease in fine particle inhalation.
Conclusions
During surgeries, the concentration of PM2.5 could reach a very unhealthy status, especially for the chief surgeon who is the nearest to the incision site. Surgical smoke evacuation in the first few seconds of a cut is essential; however, using smoke evacuators such as a wall suction alone may not be enough.



Similar content being viewed by others
References
Choi SH, Kwon TG, Chung SK, Kim TH (2014) Surgical smoke may be a biohazard to surgeons performing laparoscopic surgery. Surg Endosc 28(8):2374–2380. doi:10.1007/s00464-014-3472-3
Zhao C, Kim MK, Kim HJ, Lee SK, Chung YJ, Park JK (2013) Comparative safety analysis of surgical smoke from transurethral resection of the bladder tumors and transurethral resection of the prostate. Urology 82(3):744.e9–744.e14. doi:10.1016/j.urology.2013.05.028
Hensman C, Baty D, Willis RG, Cuschieri A (1998) Chemical composition of smoke produced by high-frequency electrosurgery in a closed gaseous environment. An in vitro study. Surg Endosc 12(8):1017–1019
Barrett WL, Garber SM (2003) Surgical smoke: a review of the literature. Is this just a lot of hot air? Surg Endosc 17(6):979–987. doi:10.1007/s00464-002-8584-5
Garden JM, O’Banion MK, Bakus AD, Olson C (2002) Viral disease transmitted by laser-generated plume (aerosol). Arch Dermatol 138(10):1303–1307
Brook RD, Franklin B, Cascio W, Hong Y, Howard G, Lipsett M, Luepker R, Mittleman M, Samet J, Smith SC Jr, Tager I (2004) Air pollution and cardiovascular disease: a statement for healthcare professionals from the Expert Panel on Population and Prevention Science of the American Heart Association. Circulation 109(21):2655–2671. doi:10.1161/01.CIR.0000128587.30041.C8
Weld KJ, Dryer S, Ames CD, Cho K, Hogan C, Lee M, Biswas P, Landman J (2007) Analysis of surgical smoke produced by various energy-based instruments and effect on laparoscopic visibility. J Endourol 21(3):347–351. doi:10.1089/end.2006.9994
Walczak DA, Grobelski B, Pasieka Z (2011) “There is no smoke without a fire”—surgical smoke and the risk connected with it. Pol Przegl Chir 83(11):634–639. doi:10.2478/v10035-011-0101-x
Atkinson RW, Kang S, Anderson HR, Mills IC, Walton HA (2014) Epidemiological time series studies of PM2.5 and daily mortality and hospital admissions: a systematic review and meta-analysis. Thorax 69(7):660–665. doi:10.1136/thoraxjnl-2013-204492
Semple S, Ibrahim AE, Apsley A, Steiner M, Turner S (2013) Using a new, low-cost air quality sensor to quantify second-hand smoke (SHS) levels in homes. Tob Control. doi:10.1136/tobaccocontrol-2013-051188
Edwards BE, Reiman RE (2012) Comparison of current and past surgical smoke control practices. AORN J 95(3):337–350. doi:10.1016/j.aorn.2011.07.019
Yu Q, Lu Y, Xiao S, Shen J, Li X, Ma W, Chen L (2012) Commuters’ exposure to PM1 by common travel modes in Shanghai. Atmos Environ 59:39–46
U.S. Environmental Protection Agency (EPA) (2011) Exposure factors handbook: 2011 Edition. National Center for Environmental Assessment W, DC; EPA/600/R-09/052F. Available from the National Technical Information Service, Springfield, VA, and online at http://www.epa.gov/ncea/efh
Revised Air Quality Standards For Particle Pollution and Updates to the Air Quality Index (AQI). The National Ambient Air Quality Standards for Particle Pollution web site: http://www.epa.gov/airquality/particlepollution/2012/decfsstandards.pdf
Brook RD, Rajagopalan S, Pope CA 3rd, Brook JR, Bhatnagar A, Diez-Roux AV, Holguin F, Hong Y, Luepker RV, Mittleman MA, Peters A, Siscovick D, Smith SC Jr, Whitsel L, Kaufman JD (2010) Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation 121(21):2331–2378. doi:10.1161/CIR.0b013e3181dbece1
Beelen R, Raaschou-Nielsen O, Stafoggia M, Andersen ZJ, Weinmayr G, Hoffmann B, Wolf K, Samoli E, Fischer P, Nieuwenhuijsen M, Vineis P, Xun WW, Katsouyanni K, Dimakopoulou K, Oudin A, Forsberg B, Modig L, Havulinna AS, Lanki T, Turunen A, Oftedal B, Nystad W, Nafstad P, De Faire U, Pedersen NL, Ostenson CG, Fratiglioni L, Penell J, Korek M, Pershagen G, Eriksen KT, Overvad K, Ellermann T, Eeftens M, Peeters PH, Meliefste K, Wang M, Bueno-de-Mesquita B, Sugiri D, Kramer U, Heinrich J, de Hoogh K, Key T, Peters A, Hampel R, Concin H, Nagel G, Ineichen A, Schaffner E, Probst-Hensch N, Kunzli N, Schindler C, Schikowski T, Adam M, Phuleria H, Vilier A, Clavel-Chapelon F, Declercq C, Grioni S, Krogh V, Tsai MY, Ricceri F, Sacerdote C, Galassi C, Migliore E, Ranzi A, Cesaroni G, Badaloni C, Forastiere F, Tamayo I, Amiano P, Dorronsoro M, Katsoulis M, Trichopoulou A, Brunekreef B, Hoek G (2014) Effects of long-term exposure to air pollution on natural-cause mortality: an analysis of 22 European cohorts within the multicentre ESCAPE project. Lancet 383(9919):785–795. doi:10.1016/S0140-6736(13)62158-3
Raaschou-Nielsen O, Andersen ZJ, Beelen R, Samoli E, Stafoggia M, Weinmayr G, Hoffmann B, Fischer P, Nieuwenhuijsen MJ, Brunekreef B, Xun WW, Katsouyanni K, Dimakopoulou K, Sommar J, Forsberg B, Modig L, Oudin A, Oftedal B, Schwarze PE, Nafstad P, De Faire U, Pedersen NL, Ostenson CG, Fratiglioni L, Penell J, Korek M, Pershagen G, Eriksen KT, Sorensen M, Tjonneland A, Ellermann T, Eeftens M, Peeters PH, Meliefste K, Wang M, Bueno-de-Mesquita B, Key TJ, de Hoogh K, Concin H, Nagel G, Vilier A, Grioni S, Krogh V, Tsai MY, Ricceri F, Sacerdote C, Galassi C, Migliore E, Ranzi A, Cesaroni G, Badaloni C, Forastiere F, Tamayo I, Amiano P, Dorronsoro M, Trichopoulou A, Bamia C, Vineis P, Hoek G (2013) Air pollution and lung cancer incidence in 17 European cohorts: prospective analyses from the European Study of Cohorts for Air Pollution Effects (ESCAPE). Lancet Oncol 14(9):813–822. doi:10.1016/S1470-2045(13)70279-1
Cesaroni G, Forastiere F, Stafoggia M, Andersen ZJ, Badaloni C, Beelen R, Caracciolo B, de Faire U, Erbel R, Eriksen KT, Fratiglioni L, Galassi C, Hampel R, Heier M, Hennig F, Hilding A, Hoffmann B, Houthuijs D, Jockel KH, Korek M, Lanki T, Leander K, Magnusson PK, Migliore E, Ostenson CG, Overvad K, Pedersen NL, Juha Pekkanen J, Penell J, Pershagen G, Pyko A, Raaschou-Nielsen O, Ranzi A, Ricceri F, Sacerdote C, Salomaa V, Swart W, Turunen AW, Vineis P, Weinmayr G, Wolf K, de Hoogh K, Hoek G, Brunekreef B, Peters A (2014) Long term exposure to ambient air pollution and incidence of acute coronary events: prospective cohort study and meta-analysis in 11 European cohorts from the ESCAPE Project. BMJ 348:f7412
Pedersen M, Giorgis-Allemand L, Bernard C, Aguilera I, Andersen AM, Ballester F, Beelen RM, Chatzi L, Cirach M, Danileviciute A, Dedele A, Eijsden M, Estarlich M, Fernandez-Somoano A, Fernandez MF, Forastiere F, Gehring U, Grazuleviciene R, Gruzieva O, Heude B, Hoek G, de Hoogh K, van den Hooven EH, Haberg SE, Jaddoe VW, Klumper C, Korek M, Kramer U, Lerchundi A, Lepeule J, Nafstad P, Nystad W, Patelarou E, Porta D, Postma D, Raaschou-Nielsen O, Rudnai P, Sunyer J, Stephanou E, Sorensen M, Thiering E, Tuffnell D, Varro MJ, Vrijkotte TG, Wijga A, Wilhelm M, Wright J, Nieuwenhuijsen MJ, Pershagen G, Brunekreef B, Kogevinas M, Slama R (2013) Ambient air pollution and low birthweight: a European cohort study (ESCAPE). Lancet Respir Med 1(9):695–704. doi:10.1016/S2213-2600(13)70192-9
Spearman J, Tsavellas G, Nichols P (2007) Current attitudes and practices towards diathermy smoke. Ann R Coll Surg Engl 89(2):162–165. doi:10.1308/003588407X155752
Acknowledgments
This work was supported by grants from the National Natural Science Foundation of China (No. 81202004).
Author contributions
Hong-Kai Wang, Fei Mo and Hai-Liang Zhang had full access to all of the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis. Hong-Kai Wang, Fei Mo, Chun-Guang Ma, Bo Dai, Guo-Hai Shi, and Yao Zhu involved in acquisition of data. Hai-Liang Zhang involved in study concept and design. Hong-Kai Wang wrote the manuscript. Supervision: Ding-Wei Ye and Hai-Liang Zhang conceived of the study and participated in its design and coordination.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
All authors declare no competing financial interests.
Additional information
Hong-Kai Wang and Fei Mo have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Wang, HK., Mo, F., Ma, CG. et al. Evaluation of fine particles in surgical smoke from an urologist’s operating room by time and by distance. Int Urol Nephrol 47, 1671–1678 (2015). https://doi.org/10.1007/s11255-015-1080-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-015-1080-3