Abstract
Purpose
To explore the types of proteinuria in the elderly population in China.
Methods
Seven hundred and fourteen elderly people (≥60 years old) from Tianjin, China, were selected for the study. The albumin-to-creatinine ratio and α1-microglobulin-to-creatinine ratio from morning urine samples were used as indicators of proteinuria. The prevalence of proteinuria was evaluated and the proportion of three different types of proteinuria (mixed, glomerular, and tubular) was assessed in the subjects by analyzing these indicators.
Results
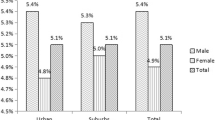
Of the 714 subjects, 29.13 % had elevated ACR and 46.36 % had elevated MCR. The proportion of subjects with either elevated ACR or MCR was 53.78 %. The correlation between MCR and ACR was moderate (r = 0.58, R 2 = 0.34, P < 0.001). Overall, tubular proteinuria was dominant (45.83 %), followed by mixed glomerular and tubular proteinuria (35.68 %), and significantly higher than glomerular proteinuria. A diet high in salt was the independent risk factor for tubular proteinuria; physical activity was the independent risk factor for glomerular proteinuria. The risk of glomerular proteinuria was lower in males than in females, but the risk of tubular proteinuria was higher in males.
Conclusions
The prevalence of tubular proteinuria was higher than that of glomerular proteinuria, and the risk factors are different, in the elderly in China; therefore, tubular damage markers should get more attention in the overall population.

Similar content being viewed by others
References
Methven S, MacGregor MS, Traynor JP et al (2010) Assessing proteinuria in chronic kidney disease: protein–creatinine ratio versus albumin-creatinine ratio. Nephrol Dial Transplant 9:2991–2996
Nauta FL, Scheven L, Meijer E et al (2013) Glomerular and tubular damage markers in individuals with progressive albuminuria. Clin J Am Soc Nephrol 7:1106–1114
El Nahas M (2010) Cardio-Kidney-Damage: a unifying concept. Kidney Int 1:14–18
Saydah SH, Pavkov ME, Zhang C et al (2013) Albuminuria prevalence in first morning void compared with previous random urine from adults in the National Health and Nutrition Examination Survey, 2009–2010. Clin Chem 4:675–683
O’Hare AM, Hailpern SM, Pavkov ME et al (2010) Prognostic implications of the urinary albumin to creatinine ratio in veterans of different ages with diabetes. Arch Intern Med 11:930–936
Bonventre J, Can V (2012) Can we target tubular damage to prevent renal function decline in diabetes? Semin Nephrol 5:452–462
Gibb DM, Tomlinson PA, Dalton NR et al (1989) Renal tubular proteinuria and microalbuminuria in diabetic patients. Arch Dis Child 1:129–134
Ekstrom B, Peterson PA, Berggard I (1975) A urinary and plasma α1-glycoprotein of low molecular weight: isolation and some properties. Biochem Biophys Res Commun 65:1427–1433
Yu H, Yanagisawa Y, Forbes MA et al (1983) Alpha-1-microglobulin: an indicator protein for renal tubular function. J Clin Pathol 3:253–259
Thomas Lothar (1998) Clinical Laboratory Diagnostics: Use and Assessment of Clinical Laboratory Results. TH-Books, Frankfurt am Main, pp 357–375
Fioretto P, Mauer M (2007) Histopathology of diabetic nephropathy. Semin Nephrol 27:195–207
Hong CY, Hughes K, Chia KS et al (2003) Urinary alpha1-microglobulin as a marker of nephropathy in type 2 diabetic Asian subjects in Singapore. Diabetes Care 2:338–342
Wang HB, Liu R (2014) Current Progress of the prevalence of albuminuria and its influencing factors. Chin J Lab Med 12:973–976
Group of Chinese Guidelines for the Management of Hypertension (2011) The 2010 Chinese guidelines for the management of hypertension. Chin J Cardiol 39(7):579–616
Chen B, Yang D, Chen Y et al (2010) The prevalence of microalbuminuria and its relationships with the components of metabolic syndrome in the general population of China. Clin Chim Acta 9–10:705–709
Acknowledgments
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. However, we appreciate Tianjin Jun Liangcheng Hospital for supporting this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No authors declared the potential conflict of interest.
Additional information
Hua-Bin Wang and Qing-Hong Yang have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Wang, HB., Yang, QH., Jiang, X. et al. Tubular proteinuria is the dominant type of proteinuria in an elderly community population in China. Int Urol Nephrol 47, 1541–1546 (2015). https://doi.org/10.1007/s11255-015-1064-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-015-1064-3