Abstract
Background
Under physiological conditions, kidneys work continuously, 168 h/week. In contrast, patients with end-stage renal disease are usually dialysed only 12 h/week. Even if considered adequate by current Kt/V-based dose estimates, this unphysiological dose is associated with an unacceptable annual mortality rate of 10–20%. Increasing dialysis dose might ameliorate this mortality rate.
Design
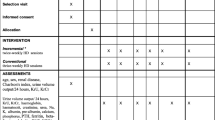
Eleven patients were switched from their conventional haemodialysis (cHD, 3 × 4 h/week) to an intensified short daily home haemodialysis regimen (sdhHD, 6 × 3 h/week) and followed up for 12 months. Different parameters were evaluated before treatment conversion and quarterly during follow-up [i.e. dialysis efficacy, mean arterial pressure (MAP), antihypertensive drug score, haemoglobin, transferrin saturation, ferritin, dose of erythropoiesis-stimulating agents (ESA), iron requirement, parameters of nutrition (body weight, albumin, protein), C-reactive protein, calcium–phosphate product, alkaline phosphatase (AP), intact parathyroid hormone (iPTH) and amount of phosphate-binding pharmacotherapy].
Results
HD efficacy as assessed by cumulative blood volume increased after dialysis intensification (P < 0.01). The pre- and post-dialytic MAP declined during the study period (P < 0.0001), while antihypertensive drugs could be reduced (P = 0.02). Haemoglobin levels improved (P < 0.0001). Additionally, the need for ESAs fell under intensified sdhHD (P = 0.008). Nutritional status improved [albumin, P = 0.03; total serum protein, P = 0.02; ‘dry’ body weight (BW) and body mass index (BMI) (both P < 0.001)]. The calcium–phosphate product declined (P < 0.01), without changes in the dose of phosphate binders.
Conclusion
Conversion from conventional in-centre to short daily home HD leads to an improvement in numerous dialysis-associated metabolic variables and thus represents an attractive treatment modality for selected patients.


Similar content being viewed by others
References
US Renal Data System (2006): USRDS 2006 Annual Data Report: Atlas of End-Stage Renal Disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD
DePalma JR, Pecker EA, Maxwell MH (1969) A new automatic coil dialyser system for ‘daily’ dialysis. Proc EDTA 6:26
Baillod R, Comty C, Shaldon S (1965) Over-night haemodialysis in the home. Proc Eur Dial Transplant Assoc 2:99–104
Rao M, Muirhead N, Klarenbach S et al (2003) Management of anemia with quotidian haemodialysis. Am J Kidney Dis 42:18–23
Fagugli RM, Reboldi G, Quintaliani G et al (2001) Short-daily haemodialysis: blood pressure control and left ventricular mass reduction in hypertensive haemodialysis patients. Am J Kidney Dis 38:371–376
Lindsay RM, Alhejaili F, Nesrallah G et al (2003) Calcium and phosphate balance with quotidian haemodialysis. Am J Kidney Dis 42:24–29
Spanner E, Suri R, Heidenheim AP et al (2003) The impact of quotidian haemodialysis on nutrition. Am J Kidney Dis 42:30–35
Heidenheim AP, Muirhead N, Moist L et al (2003) Patient quality of life on quotidian haemodialysis. Am J Kidney Dis 42:36–41
Oreopoulos DG, Thodis E, Passadakis P et al (2009) Home dialysis as a first option: a new paradigm. Int Urol Nephrol 41(3):595–605
Flanigan MJ, Khairullah QT, Lim VS (1997) Dialysate sodium delivery can alter chronic blood pressure management. Am J Kidney Dis 29:383–391
Jacobs C, Frei D, Perkins AC (2005). Results of the European Survey on Anaemia Management 2003 (ESAM 2003): current status of anaemia management in dialysis patients, factors affecting epoetin dosage and changes in anaemia management over the last 5 years. Nephrol Dial Transplant; 20:iii3–iii24
Ledebo I, Lameire N, Charra B et al. (2000) Improving the outcome of dialysis–opinion vs scientific evidence. Report on the Dialysis Opinion Symposium at the ERA-EDTA Congress, 6 September 1999, Madrid. Nephrol Dial Transplant; 15: 1310–1316
Nesrallah G, Suri R, Moist L et al (2003) Volume control and blood pressure management in patients undergoing quotidian haemodialysis. Am J Kidney Dis 42:13–17
Trial Group FHN, Chertow GM, Levin NW, Beck G et al (2010) In-center hemodialysis six times per week versus three times per week. N Engl J Med 363(24):2287–2300
Pecoits-Filho R, Lindholm B, Stenvinkel P (2002) The malnutrition, inflammation, and atherosclerosis (MIA) syndrome—the heart of the matter. Nephrol Dial Transplant 17:28–31
Yuen D, Richardson RM, Chan CT (2005) Improvements in phosphate control with short daily in-center haemodialysis. Clin Nephrol 64(5):364–370
Charra B, Calemard E, Ruffet M et al (1992) Survival as an index of adequacy of dialysis. Kidney Int 41:1286–1291
Wilson J, Shah T, Nissenson AR (2004) Role of sodium and volume in the pathogenesis of hypertension in haemodialysis. Semin Dial 17(4):260–264
Kjellstrand CM, Buoncristiani U, Ting G et al (2008) Short daily haemodialysis: survival in 415 patients treated for 1006 patient-years. Nephrol Dial Transplant 23(10):3283–3289
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lorenzen, J.M., Thum, T., Eisenbach, G.M. et al. Conversion from conventional in-centre thrice-weekly haemodialysis to short daily home haemodialysis ameliorates uremia-associated clinical parameters. Int Urol Nephrol 44, 883–890 (2012). https://doi.org/10.1007/s11255-011-9918-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-011-9918-9