Abstract
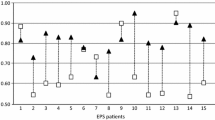
Encapsulating peritoneal sclerosis (EPS) is a serious and often fatal complication of long-term PD with severe malnutrition and poor prognosis. It causes progressive obstruction and encapsulation of the bowel. This retrospective study reviews our experience and that reviewed in the literature concerning EPS. It refers to a total of 1966 patients treated with chronic PD between 1974 and 2008. Twenty one of them (1.1%) developed EPS, with the incidence increasing with the duration of PD. Mean age of our patients with EPS was 43, ranging from 18 to 71 years, 8 were men and 13 women with a mean body mass index (BMI) of 21.6 kg/m2. Only one patient had Type II diabetes, 15 patients had glomerular disease, and six of these 15 had an autoimmune disease such as Wegener’s granulomatosis and SLE. Thirteen patients developed EPS while on PD, 7 within 2 years after transfer to HD, and only one after renal transplantation. However, 7 patients had a previous renal transplant before returning to PD and subsequently developing EPS. Interestingly, we did not observe more episodes of EPS after transplantation. In the patients who developed EPS, the peritonitis rate over the period of observation was 1/15.6 pt-months and was due to Staphylococcus aureus, coagulase-negative staphylococcus, Pseudomonas and fungi. A history of peritonitis was not a prerequisite for developing EPS, since one patient had no episodes of peritonitis and 4 had just one previous episode. Fifteen patients presented with peritonitis within 4 months before the diagnosis of EPS with particularly virulent micro-organisms such as S. aureus, Candida, Pseudomonas, Corynebacterium, and Peptostreptococcus. Eleven patients were treated with hypertonic dextrose solutions (4.25 g/dl of dextrose) and seven with icodextrin, indirectly suggesting problems with ultrafiltration. Nine of 21 patients were on beta-blockers. The diagnosis of EPS was made either surgically or radiologically with signs of small bowel obstruction in combination with severe malnutrition. Eleven of our patients (52%) had evidence of small bowel obstruction and 14 patients required total parenteral nutrition (TPN). Tamoxifen (10–20 mg daily) was started in 6 patients, 4 of whom are alive and 2 deceased 3 and 5 years after EPS was diagnosed. Of the 12 patients who were not given tamoxifen, 2 are alive and 10 died. No side effects of tamoxifen were reported. Only 7 of our patients (33%) died during the first year after the diagnosis of EPS. Currently, 4 patients are on HD and 3 have had a renal transplant. Six patients of the fourteen who underwent surgery (42.8%) died within the first 6 months after operation and five died after an average of 6.6 years, mostly due to cardiovascular causes, three are still alive. As EPS becomes more prevalent with longer duration of PD, large multicenter prospective studies are needed to establish its incidence and identify risk factors, therapeutic approach, and prognosis.
Similar content being viewed by others
References
Kawanishi H, Watanabe H, Moriishi M, Tsuchiya S (2005) Successful surgical management of encapsulating peritoneal sclerosis. Perit Dial Int 25(Suppl 4):39–47
Guest S (2009) Hypothesis: gender and encapsulating peritoneal sclerosis. Perit Dial Int 29(5):489–491
Slingeneyer A, Mion C, Mourad G, Ganaud B, Faller B, Beraud JJ (1983) Progressive sclerosing peritonitis: a late and severe complication of maintenance peritoneal dialysis. Trans AM Soc Artif Intern Organs 29:633–640
Balasubramaniam G, Brown EA, Davenport A, Cairns H, Cooper B, Fan SLS, Farrington K, Galagher H, Harnett P, Krausze S, Steddon S (2009) The Pan-thames EPS study: treatment and outcomes of encapsulating peritoneal sclerosis. Nephrol Dial Transplant 24(10):3209–3215
Afthentopoulos IE, Passadakis P, Oreopoulos DG, Bargman J (1998) Sclerosing peritonitis in continuous ambulatory peritoneal dialysis patients: one center’s experience and review of the literature. Adv Ren Replace Ther Oct 5(3):157–167
Brown MC, Simpson K, Kerssens JJ, Mactier RA (2009) Encapsulating peritoneal sclerosis in the new millennium: a national cohort study. Clin J Am Soc Nephrol 4(7):1222–1229
Maitra S, Burkart J, Prichard S, Bernardini J, Jindal KK, Oreopoulos DG (2000) Patients on chronic dialysis for 10 years or more in North America. Perit Dial Int 20(Suppl 2):S127–S133
Oules R, Challah S, Brunner FP (1988) Case-control study to determine the cause of sclerosing peritoneal disease. Nephrol Dial Transplant 3(1):66–69
Rigby R, Hawley M (1998) Sclerosing peritonitis: the experience in Australia. Nephrol Dial Transplant 13(1):154–159
Korte MR et al (2007) Increasing incidence of severe encapsulating peritoneal sclerosis after kidney transplantation. Nephrol Dial Transplant 22(8):2412–2414
Krishnan M, Thodis E, Ikonomopoulos D, Vidgen E, Chu M, Bargman JM, Vas SI, Oreopoulos DG (2002) Predictors of outcome following bacterial peritonitis in peritoneal dialysis. Perit Dial Int 22(5):573–581
Summers AM, Clancy MJ, Syed F, Harwood N, Brenchley PEC, Augustine T, Riad H, Hutchison AJ, Taylor P, Pearson R (2005) Single center experience of encapsulating peritoneal sclerosis in patients on peritoneal dialysis for end-stage renal failure. Kidney Int 68(5):2381–2388
Sawai T, Tomono K et al (1997) Role of coagulase in a murine model of hematogenous pulmonary infection induced by intravenous injection of Staphylococcus aureus enmeshed in agar beads. Infect Immun 65(2):466–471
Nakamoto H, Imai H, Ishida Y, Yamanouchi Y, Inoue T, Okade H, Suzuki H (2001) New animal models for encapsulating peritoneal sclerosis—role of acidic solution. Perit Dial Int 21(Suppl 3):S349–S353
Lafrance JP, Letourneau I, Ouimet D, Bonnardeux A, Leblanc M, Mathieu N, Pichette V (2008) Successful treatment of encapsulating peritoneal sclerosis with immunosuppressive therapy. Am J Kidney Dis 51(2):e7–e10
Kawanishi H, Moriishi M (2005) Epidemiology of encapsulating peritoneal sclerosis in Japan. Perit Dial Int 25(S4):S14–S18
Hall DR, Morrison JB, Edwards FR (1978) Pleural fibrosis after practolol therapy. Thorax 33(6):822–824
Noh H, Ha H, Yu MR, Kim YO, Kim JH, Lee HB (2005) Angiotensin II mediates high glucose-induced TGF-beta1 and fibronectin upregulation in HPMC through reactive oxygen species. Perit Dial Int 25(1):38–47
Sawada T, Ishii Y, Tojimbara T, Nakajima I, Fuchinoue S, Teraoka S (2002) The ACE inhibitor, quinapril, ameliorates peritoneal fibrosis in an encapsulating peritoneal sclerosis model in mice. Pharmacol Res 46(6):505–510
Kyuden I, Ito T, Yorioka N, Kohno N (2005) TGF-beta1 induced by high glucose is controlled by angiotensin-converting enzyme inhibitor and angiotensin II receptor blocker on cultured human peritoneal mesothelial cells. Perit Dial Int 25(5):483–491
Nakamoto H, Imai H, Fukushima R, Ishida Y, Yamanouchi Y, Suzuki H (2008) Role of the renin-angiotensin system in the pathogenesis of peritoneal fibrosis. Perit Dial Int 28(Suppl 3):S83–S87
Sampimon DE, Korte MR, Lopes Barreto D, Vlijm A, de Waart DR, Struijk DG, Krediet RT (2010) Early diagnostic markers for EPS—a case-control study. Perit Dial Int 30(2):163–169
Krediet RT, Sampimon DE, Vlijm A, Coester AM, Struijk DG, Smit W (2009) Biological markers in the peritoneal dialysate: are they useful? Contrib Nephrol 163:54–59
Parikova A, Zweers MM, Struijk DG, Krediet RT (2003) Peritoneal effluent markers of inflammation in patients treated with icodextrin-based and glucose-based dialysis solutions. Adv Perit Dial 19:186–190
Dedeoglu F, Rose CD, Athreya BH et al (2001) Successful treatment of retroperitoneal fibrosis with tamoxifen in a child. J Rheumatol 28(7):1693–1695
Frankart L, Lorge F, Donckier J (1997) Tamoxifen for retroperitoneal fibrosis. Postgrad Med J 73(864):653–654
Tallarigo C, D’ Amico A, Pocaro AB et al (2000) Our experience in the treatment of retroperitoneal fibrosis. Arch Ital Urol Androl 72(2):51–58
Ruffy M, Kunnavatana S, Koch R (2006) Effects of tamoxifen on normal human dermal fibroblasts. Arch Facial Plast Surg 8:329–332
Payne WG, Ko F, Anspaugh S, Wheeler CK, Wright TE, Robson MC (2006) Down- regulating causes of fibrosis with tamoxifen: a possible cellular/molecular approach to treat rhinophyma. Ann Plast Surg 56:301–305
Eltoum MA, Wright S, Atchley J, Mason JC (2006) Four consecutive cases of peritoneal dialysis-related encapsulating peritoneal sclerosis treated successfully with Tamoxifen. Perit Dial Int 26(2):203–206
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Trigka, K., Dousdampanis, P., Chu, M. et al. Encapsulating peritoneal sclerosis: a single-center experience and review of the literature. Int Urol Nephrol 43, 519–526 (2011). https://doi.org/10.1007/s11255-010-9848-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-010-9848-y