Abstract
Introduction
It is controversial whether microscopic invasion of the bladder neck (BN) has a high risk for biochemical progression following radical prostatectomy (RP). The tumor, node, and metastasis (TNM) classification for prostate cancer considers BN involvement to be pT4 disease, equivalent to rectal or external sphincter invasion, however, it does not specify whether the invasion is macroscopic or microscopic.
Materials and methods
Clinicopathological findings were studied from 290 patients submitted to RP. The time to biochemical (prostate-specific antigen, PSA) progression-free outcome for patients with BN invasion was compared to patients with extraprostatic extension (EPE) or seminal vesicle invasion (SVI). A univariate Cox proportional hazards model was created and a final multivariate Cox proportional hazards model was developed to assess the influence of several variables simultaneously.
Results
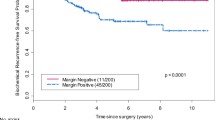
BN invasion was present in 55/290 (18.96%) surgical specimens and 18/290 (6.2%) also showed positive surgical margins. Patients with microscopic BN invasion had significantly higher preoperative PSA, higher Gleason score, higher apical and circumferential positive surgical margins, more advanced pathological stage, and more extensive tumors. At 5 years 42%, 40%, and 27% of the patients with BN invasion, extraprostatic extension (EPE), and seminal vesicle invasion (SVI), respectively, were free of biochemical recurrence following RP. In multivariate analysis, BN invasion did not contribute for a higher relative hazard of PSA recurrence when added to EPE or SVI.
Conclusion
BN invasion is associated with adverse clinicopathological findings. However, the biochemical-free outcome following RP is similar to patients with EPE but significantly better than patients with SVI. The findings of this study do not favor considering microscopic bladder neck invasion as stage pT4 but, probably, stage pT3a.



Similar content being viewed by others
References
Yossepowitch O, Engelstein D, Konichezky M et al (2000) Bladder neck involvement at radical prostatectomy: positive margins or advanced T4 disease? Urology 56:448–452
Dash A, Sanda MG, Yu M et al (2002) Prostate cancer involving the bladder neck: recurrence-free survival and implications for AJCC staging modifications. Urology 60:276–280
Yossepowitch O, Sircar K, Scardino PT et al (2002) Bladder neck involvement in pathological stage pT4 radical prostatectomy specimens is not an independent prognostic factor. J Urol 68:2011–2015
Walsh PC (1986) Radical retropubic prostatectomy. In: Walsh PC, Gittes RF, Perlmutter AD, Stamey TA (eds) Campbell’s urology, vol 3, 5th edn. WB Saunders, Philadelphia, pp 2754–2775
Billis A, Magna LA, Ferreira U (2003) Correlation between tumor extent in radical prostatectomies and preoperative PSA, histological grade, surgical margins, and extraprostatic extension: application of a new practical method for tumor extent evaluation. Int Braz J Urol 29:113–120
Epstein JI, Carmichael M, Walsh PC (1993) Adenocarcinoma of the prostate invading the seminal vesicle: definition and relation of tumor volume, grade and margins of resection to prognosis. J Urol 149:1040–1045
Bostwick DG, Montironi R (1997) Evaluating radical prostatectomy specimens: therapeutic and prognostic importance. Virchows Arch 430:1–16
Cookson MS, Aus G, Burnett AL et al (2007) Variation in the definition of biochemical recurrence in patients treated for localizaed prostate cancer: the American urological association prostate guidelines for localized prostate cancer update panel report and recommendations for a standard in the reporting of surgical outcomes. J Urol 177:540–545
International Union Against Cancer (2002) Prostate. In: Sobin LH, Ch Wittekind (eds) TNM classification of malignant tumours, 6th edn. Wiley-Liss, New York, pp 184–187
Epstein JI, Pizov G, Walsh PC (1993) Correlation of pathologic findings with progression after radical retropubic prostatectomy. Cancer 71:3582–3593
Epstein JI, Partin AW, Sauvageot J et al (1996) Prediction of progression following radical prostatectomy: a multivariate analysis of 721 men with long-term follow up. Am J Surg Pathol 20:286–292
Van den Ouden D, Bentvelsen FM, Boeve ER et al (1993) Positive margins after radical prostatectomy: correlation with local recurrence and distant progression. Br J Urol 72:489–494
D’Amico AV, Whittington R, Malkowicz B et al (1995) A multivariate analysis of clinical and pathological factors that predict for prostate specific antigen failure after radical prostatectomy for prostate cancer. J Urol 154:131–138
Blute ML, Bostwick DG, Bergstralh EJ et al (1997) Anatomic site-specific positive margins in organ confined prostate cancer and its impact on outcome after radical prostatectomy. Urology 50:733–739
Poulos CK, Koch MO, Eble JN et al (2004) Bladder neck invasion is an independent predictor of prostate-specific antigen recurrence. Cancer 101:1563–1568
Aydin H, Tsuzuki T, Hernandez D et al (2004) Positive proximal (bladder neck) margin at radical prostatectomy confers greater risk of biochemical progression. Urology 64:551–555
Buschemeyer WCIII, Hamilton RJ, Aronson WJ et al (2008) Is a positive bladder neck margin truly a T4 lesion in the prostate specific antigen era? Results from the SEARCH Database. J Urol 179:124–129
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ruano, T., Meirelles, L., Freitas, L.L. et al. The significance of microscopic bladder neck invasion in radical prostatectomies: pT4 disease?. Int Urol Nephrol 41, 71–76 (2009). https://doi.org/10.1007/s11255-008-9400-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-008-9400-5