Abstract
Few therapeutic specialty molecules from in vitro cultures beyond paclitaxel have come to market and although other more complex products like ginseng have also appeared, success has been limited. Often it is not the science that is limiting, but rather regulatory issues that limit considerations of potential products mainly because of costs in getting the product to market. Here we discuss broader thinking of such specialty molecules in the form of dietary supplements, nutraceuticals, herbal medicines, botanical drugs, and pure molecules along with potential complex products from a regulatory standpoint and especially within the realm of approved botanical drugs, e.g., Veregen and Fulyzaq, that have new drug applications (NDAs). The United States food and drug administration (US FDA) regulatory categories are used to provide examples of alternative product options that could prove useful for taking specialty molecules to market.
Key message
In vitro produced specialty molecules can be approved as not only pure compounds but also as botanical drugs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
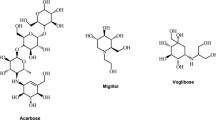
The herbal medicine market is poised to reach US$550 billion by 2030 (https://www.benzinga.com/pressreleases/21/09/ab22937181/herbal-medicine-market-2021-trends-demand-and-scope-with-outlook-business-strategies-and-forecast, accessed March 9, 2022), so there is keen interest in further developing such products from whole plants, as extracts, and from in vitro cultures. There is value added when products have approval from US food and drug administration (FDA) and other regulatory agencies or recognition from World Health Organization (WHO) as a botanical therapeutic or disease treatment agent. However, first a decision on the product composition and formulation must be made. Is the intended product a pure molecule (an active pharmaceutical ingredient, an API), a therapeutic botanical (botanical drug) for various routes of administration, or an herb, nutraceutical or dietary supplement? Such a decision determines the stringency of quality control, safety and efficacy requirements, and other regulatory details needed for gaining market permission or approval of the product. In vitro cultures, with the potential to provide all the necessary molecules in whole plants, may serve as the raw materials and yield any of these formulations (Fig. 1).
Nutraceuticals and herbal medicines are essentially the same as dietary supplements. Dietary supplements are regulated as food in the US by the FDA. Some products may be further studied and approved as Botanical Drugs with multiple or maybe not specifically characterized molecules as APIs, chemical drugs usually with one API, or fixed combinations with well-defined APIs. For purposes of this report, the regulatory requirements of the FDA will be the focus because the US FDA often serves as a reference source of information for drug approvals in other countries.
The US FDA defines a “botanical drug” as any product consisting of “vegetable materials, which may include plant materials, algae, macroscopic fungi, or combinations thereof” as a finished product (https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/what-botanical-drug, accessed on 9/24/2021). A botanical drug product may include a: powder, solution (e.g., tea infusion), topical, tablet, encapsulated material, elixir, tincture, or injection. A botanical drug has an intended use that affects the structure or function of the body including in diagnosis, mitigation, cure, treatment, or prevention of human disease. Highly purified, e.g., artemisinin, or chemically modified botanical substances, artesunate, are not considered botanical drug products.
Plant materials may include whole plants or plant parts, and their juices, gums, fatty oils, essential oils, etc.; algae or macroscopic fungi and similar products may also be considered. In the United States, botanicals and other natural products are categorized according to their intended use, such as foods (including dietary supplements), cosmetics, drugs, biologics, and medical devices. When a product is intended to be used to diagnose, treat, prevent, mitigate, or cure diseases in humans and animals, the product is a “drug” from a legal standpoint.
Pure drugs are derived from single molecules, and in this case small molecules are the focus as opposed to large molecules, such as proteins or complex carbohydrates. Botanical drugs are typically extracted from plant material and semi-purified to give an active pharmaceutical ingredient (API) with more than one active (or inactive) molecule that is then formulated along with inactive ingredients, as needed. A botanical product may or may not be used as a therapeutic. If used therapeutically, then the product must adhere to stringent FDA regulatory review as for any other non-botanical therapeutic agent on the market. A therapeutic botanical (botanical drug) may be comprised of multiple APIs within a complex botanical mixture, but with established and FDA approved therapeutic claims. Dietary supplements, which are often termed nutraceuticals by the general public and consumers, are also regulated by the US FDA, but the marketers/manufacturers may not make specific claims of health benefits that would potentially be interpreted as a drug (or pharmaceutical) claim. One of the primary indicators between dietary supplements and drugs relates to health (structure, function) claims or disease claims. A dietary supplement is meant to provide nutrients, a drug is designed to treat illness or disease. Dietary supplements may not state that they are intended to treat, diagnose, prevent, or cure diseases. If a disease treatment is claimed, then there must be an approval of the product as a drug.
For example, the anticancer drug, paclitaxel is FDA approved for treating certain cancers (Farrar and Jacobs 2020). The drug was isolated initially from yew trees (e.g., Taxus brevifolia Nutt.), later produced in vitro by cultivated Taxus sp. cells (Fett-Neto et al. 1992), and then extracted and purified according to stringent pharmaceutical guidelines. The regulations and guidelines are the same as would be used in the production of, for example, penicillin and include current Good Manufacturing Practices (cGMPs) and proper labeling. All the therapeutic indications selected for marketing are claimed only after extensive prior clinical trials have shown adequate efficacy and safety.
Ginseng (Panex ginseng C.A.Mey.), on the other hand, is mass cultivated as adventitious root cultures in large bioreactors in vitro and commercially sold as dried root mass (Choi et al. 2000; Paek et al. 2009) that is safe for per os consumption as a dietary supplement, or as an ingredient in food and drinks. Ginseng has been used in Traditional Chinese medicine (TCM) for thousands of years with multiple products approved and marketed as drugs in China and other parts of the world. Ginseng has also been touted for having health benefits in Korean and Japanese medicine systems and is now approved by the Korean food and drug administration (Gubser et al. 2021) for its disease treatment properties. On the other hand, there are no specific approved claims for treating any disease or pathology in the US, so it is classified as a dietary supplement.
Artemisia annua L. and artemisinin pose interesting examples. Currently, artemisinin, and artemisinic acid, mainly are extracted from plantation-grown plants (Wetzstein et al. 2018). The molecules are purified and further modified to produce the artemisinin derivative drugs including, artesunate, artemether, and dihydroartemisinin, which are then formulated into artemisinin combination therapies (ACTs). ACTs contain an artemisinin derivative along with a co-drug, most commonly lumefantrine, mefloquine, amodiaquine, sulfadoxine/primethamine, or piperaquine (https://www.malariaconsortium.org/pages/112.htm, accessed on December 2, 2021), to extend the therapeutic treatment effect and minimize evolution of artemisinin drug resistance. ACTs fall into the pure chemical drug regulatory classification. While there are no cost-effective plant cell cultures producing artemisinin, the production of artemisinic acid was engineered into E. coli (Martin et al. 2003) and yeast (Ro et al. 2006) and scaled to production. Unfortunately, those microbial production systems along with other market forces were barely able to compete with plantation production (Peplow 2016). Nevertheless, those microbe-engineered processes were aimed to produce products that fall within the pure chemical drug category.
An alternative approach for delivering artemisinin is through per os consumption of either the traditional tea infusion of the leaves and twigs or encapsulated dried leaves. Artemisinin is more bioavailable when consumed orally via the plant (Desrosiers et al. 2020; Desrosiers and Weathers 2016, 2018; Weathers et al. 2011). A. annua is a plant that is generally regarded as safe (GRAS) (Duke 2001) that, like ginseng, has a long ethnobotanical history of use and is reasonably safe to consume at moderate doses. Both of these delivery modes could be defined as botanical drugs, but only if a therapeutic claim was made directly relating tea or leaf consumption to treatment of a specific disease, e.g., malaria or Covid-19, and along with randomized clinical trials to validate therapeutic claims. Thus, at present the Artemisia herb falls into the dietary supplement (also often termed or interpreted, although incorrectly, as a nutraceutical) category, e.g., Artecinua produced by Atelier temenos (https://ateliertemenos.com, accessed on March 13, 2022).
The goal of this report is to provide an overview to investigators in understanding the key questions that must be answered to meet the requirements for their choice of product formulation as a new drug. There are unfortunately challenges in defining these different regulatory categories (Daliu et al. 2019). Along with several prior publications (Hoffman 2015; McChesney et al. 2019), this report aims to guide product definition to dispel regulatory confusion to improve translation of botanicals and other in vitro plant-based products into clinical trials as investigational new drugs (INDs), ultimately for regulatory approval for use in treating patients (Sorkin et al. 2020).
Single molecule, pure chemical drug regulatory considerations
For market approval of new drugs in the United States, the Federal Food, Drug and Cosmetic Act (FDCA) and regulations demand adequate and well-controlled clinical trials to demonstrate the benefits of the products outweighing their potential risks. FDA is also actively engaged in developing numerous guidance documents to articulate the agency’s current thinking on how to implement the regulations and direct the industry for more successful trials leading to timely approval of new drugs. It also is worth mentioning that many of the guidance documents were developed and became effective under the International Council for Harmonization of Technical Requirements for Pharmaceuticals for Human Use (ICH; https://www.ich.org, accessed on March 9, 2022) and members of the Organization for Economic Co-operation and Development (OECD; https://www.oecd.org/, accessed on March 9, 2022). FDA coordinates with international drug research and evaluation related activities with each regulatory agency maintaining autonomy in new drug approval responsibilities. A few key clinical evaluation related guidance documents include those under ICH-Efficacy, such as E4—Dose–Response Information to Support Drug Registration; E6—Good Clinical Practice (GCPs); E9—Statistical Principles for Clinical Trials; and E10—Choice of Control Group.
There are also other general quality (e.g., ICH-Quality), safety (e.g., ICH-Safety), multidisciplinary (e.g., ICH-Multidisciplinary), and therapeutic area-specific drug development related policies and guidance documents available on the FDA web pages (https://www.fda.gov/regulatory-information/search-fda-guidance-documents, accessed on December 15, 2021).
Other regulations and guidelines include current good manufacturing practice (cGMP), chemistry, manufacturing, and control (CMC) related to ensure product quality standards. There is also good laboratory practice (GLP) (https://www.ecfr.gov/current/title-21/chapter-I/subchapter-A/part-58, accessed on March 11, 2022) to instruct and guide the animal toxicology studies supporting INDs and new drug applications (NDAs) being conducted and documented with accuracy, consistency, integrity and overall acceptable quality.
Under the FDA, the pharmaceutical industry experienced significant growth in the past few decades. With the advances in synthetic and analytical chemistry and biotechnology, many of the new chemical drugs approved are natural products or derivatives of natural products. For example, over 90% of cancer cytotoxic chemotherapy agents are derived from higher plants, such as podophyllotoxin derivatives etoposide and teniposide, vinca alkaloids, paclitaxel and its semi-synthetic analog, docetaxel) and other natural sources (e.g., As2O3) (Newman and Cragg 2020). Three vinca alkaloids (i.e., vinblastine, vinorelbine, and vincristine) isolated from Catharanthus roseus G.Don have been approved for several decades and are still being used as cancer treatments (Moudi et al. 2013).
There are more than ten antibody–drug conjugate (ADC) drugs approved by the US FDA and regulatory agencies around the world, with the drug portion of the ADC being potent cytotoxic agents derived from plants and other natural sources. (Antibody–Drug Conjugates Up To 2021 https://www.biochempeg.com/article/74.html, accessed December 13, 2021) For example, two cytotoxic drug molecules of ADCs, deruxtecan and govitecan, are derivatives of camptothecin, an alkaloid initially isolated from the Happy Tree (Camptotheca acuminate Decne.) native to China (Wall and Wani 1996). The Happy Tree is considered an endangered species, so it is important that alternative sources of camptothecin from plants (e.g., Nothapodytes nimmoniana (J.Graham) Mabb.) and endophytes have shown some success (Mohinudeen et al. 2021).
Therapeutic botanical regulatory considerations
The mainstream prescription drug products in the US, are roughly categorized as purified small molecule drugs or chemical drugs and biologic products (e.g., monoclonal antibodies, bispecific antibodies) which usually have a well-defined composition of their active ingredients.
The general regulatory requirements for clinical data to demonstrate overall safety and efficacy and support marketing approvals of new drugs from complex naturally-derived mixtures, including botanicals, are the same as those for highly purified synthetic drugs and biologics.
To encourage and facilitate botanical drug development in the United States, the FDA has published review polices (https://www.fda.gov/media/72454/download, accessed March 10, 2022) and guidelines (http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM458484.pdf, accessed December 16, 2021) and established a new review process that includes a dedicated botanical review team (BRT) in the Center for Drug Evaluation and Research (CDER). Although botanicals and other naturally-derived substances (e.g., fish oil) can be marketed in the United States within different categories of FDA regulated products, including food, dietary supplements, cosmetics, and drugs, here we focus on new drug development from natural in vitro plant sources.
As the result of the advancements in science and technology, we are more equipped to study a wide spectrum of drug candidates, from small and purified molecules to biologics, as well as complex mixtures (such as botanicals) potentially composed of multiple classes of active and inactive molecules. Since 2000, the year that the Guidance for Industry-Botanical Drug Products (Draft) was published, there have been two botanical NDA approvals: Veregen from green tea (the leaves of Camellia sinensis (L.) Kuntze) for the treatment of genital warts, and Fulyzaq from dragon’s blood (the latex of Croton lechleri Müll. Arg.) for relief from diarrhea in HIV/AIDS patients on anti-retroviral therapy. Their NDA and IND review experience was reported in several articles (Chen et al. 2008; Dou et al. 2019; Lee et al. 2015).
The FDA guidance document describes CDER’s “current thinking on appropriate development plans for botanical drugs to be submitted in NDAs and specific recommendations on submitting INDs in support of future NDA submissions for botanical drugs” (https://www.fda.gov/regulatory-information/search-fda-guidance-documents/botanical-drug-development-guidance-industry, accessed December 15, 2021). The botanical guidance document defined a botanical drug as a botanical derived mixture (in contrast with the purified chemical drugs) that is being development as an indication for disease treatment, diagnosis, or prevention. Oral, topical, injectable (e.g., intramuscular, intravenous), and all suitable routes of administration and formulation could be used for developing botanical drugs. Previously documented human experience also can be used to speed early phase clinical trials, e.g., Phase 1 dose-ranging in healthy volunteers and Phase 2 proof-of-concept studies in patients. These can be based on prior use as traditional formulas, refined concentrated extracts, combinations with a market history in the US as a dietary supplement, or use as an herbal medicine in foreign countries. For phase 3 trials, controls of raw materials are required as part of the CMC, quantitative and qualitative chemical analyses, and bioassay to ensure batch-to-batch consistency and GLP toxicology studies are often necessary. With both safety and efficacy results from the phase 3 trial(s), a NDA can be submitted and potentially approved.
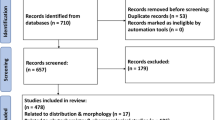
At the end of 2018, the accumulated number of INDs and pre-IND meeting consultations received in CDER at FDA reached 800. About 1/3 of the INDs were categorized as commercial INDs and sponsors were aiming to advance their drug development programs to NDA submissions. Due to some of the challenging issues surrounding botanicals, the botanical commercial INDs had a relatively low success rate of advancing into Phase 3 trials, roughly 5% compared to the 14% of all commercial INDs submitted to FDA (Wu et al. 2020). Although there have been no new NDA approvals after Mytesi/Fulyzaq’s approval in 2012, at least two additional market applications were submitted to FDA in the past few years, including an NDA for a birch bark extract product, Filsuvez Gel, indicated for epidermolysis bullosa (EB) (https://epidermolysisbullosanews.com/2021/12/03/fda-extends-decision-on-filsuvez-gel-for-skin-wounds-to-february/, accessed December 16, 2021) and a Biologics License Application (BLA) for NexoBrid that is enriched in bromalin from pineapple for burn application (https://www.globenewswire.com/news-release/2021/06/29/2254769/30505/en/MediWound-Receives-Complete-Response-Letter-from-U-S-FDA-for-NexoBrid-Biologics-License-Application.html, accessed December 16, 2021).
Botanical dietary supplement related regulatory considerations
The US congress passed the “Dietary Supplement Health and Education Act” (DSHEA; 1994) that included herbs or traditional medicines that are commonly used in China, India, Europe, and other Asian countries, Africa, South America. Prior to the passage of DSHEA those traditional medicines could be marketed in the US as dietary supplements without further evaluation or research. Dietary supplements, many with their prior human use history as medicines outside of the US, are not permitted to bear any drug claims, but with a disclaimer as follows: “These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.” (https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRsearch.cfm?fr=101.93, accessed December 15, 2021).
Despite the FDA definition of dietary supplements, herbal and traditional medicines native to the US or imported from foreign countries can be consumed by the US population as dietary supplements and may include, for example, sleep aids, immune enhancement, regulation of bowl movement, or lessening certain minor symptoms such as knee discomfort (or minor pain). Sometimes, the differentiation of disease indications and dietary supplement claims may be not straightforward, such as fatigue related to minor diseases such as the common cold or serious conditions, such as cancer or depression, etc.
For dietary supplements, only oral formulations as tablets, capsules, and liquids, are permissible; patches, creams, injections, etc., are not viable product development pathways. Herbal dietary supplements, especially those used in traditional Chinese or Ayurveda medicine, remain popular in the US, and are often used together with minerals and vitamins.
Because dietary supplements are assumed to be safe, long term and high levels of consumption could potentially lead to harmful effects. There is no regulatory framework that obviates those possible adverse effects. There is a misinformed assumption within the general population that if it is natural, it is safe. This is not true as many natural products are very toxic if not used appropriately.
The need for an IND to conduct clinical trials of botanical drug products in humans
A botanical product can be regulated as a drug, or a dietary supplement based on its intended use and how the product is labeled. In general, whether an IND application is required for a human clinical trial involving a botanical marketed as a food/dietary supplement depends on whether the intended use is for a structure/function claim (no IND needed) or a disease claim (IND needed), and not on the physical or chemical properties of the product.
Clinical trials of a new drug product in human subjects often require submitting an IND application to ensure that the study drug will not cause unreasonable harm to the human subjects enrolled in the clinical studies. Preliminary safety and proof-of-concept studies are often conducted (e.g., Phase 1 and Phase 2) before initiation of well-controlled Phase 3 trials with apparent regulatory, scientific and other related considerations provided.
Regarding studies evaluating certain cellular mechanisms or pharmacodynamic responses, such as antioxidant activity, immune modulation, and COX-2 inhibition, the decision to require an IND may be based on whether the clinical data will be used to support the product’s future labeling and proposed marketed use, and on whether there is a safety concern. For example, a clinical investigation designed to study the relationship between a dietary supplement’s effect on normal structure or function in humans (e.g., guarana, the seeds of Paullinia cupana Kunth., and maximal oxygen uptake) or to characterize the mechanism by which a dietary supplement acts to maintain a structure or function (e.g., fiber and bowel regularity) would not need to be conducted under an IND. Psyllium creates an interesting example, as it could be labeled and used to treat constipation as an over the counter (OTC) drug, but still could be used as a dietary supplement for “bowel regularity”.
Conclusions
Therapeutic in vitro products must adhere to the regulatory requirements needed at the level of scrutiny needed for the product’s intended final use. Specialty molecules from plants, and also animals, can be developed from in vitro cultures for life saving medications, with adequate quality control, animal toxicology data, and most importantly, human clinical trials to demonstrate both safety and efficacy. Although herbal products typically used as food or dietary supplements, and botanical combinations used in traditional herbal medicines, can be resources for the development of purified small molecules, it is likely more important to develop them as botanical drugs for unmet global public health needs.
Data availability
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
Abbreviations
- ACT:
-
Artemisinin combination therapy
- ADC:
-
Antibody–drug conjugate
- API:
-
Active pharmaceutical ingredient
- BLA:
-
Biologics license agreement
- BRT:
-
Botanical review team
- CDER:
-
Center for drug evaluation and research
- CMC:
-
Chemistry manufacturing and control
- EB:
-
Epidermolysis bullosa
- FDA:
-
US food and drug administration
- GLP:
-
Good laboratory practice
- cGMP:
-
Current good manufacturing practice
- GRAS:
-
Generally recognized as safe
- ICH:
-
International Council for Harmonization of Technical Requirements for Pharmaceuticals for Human Use
- IND:
-
Investigational new drug
- NDA:
-
New drug application
- OECD:
-
Organization for economic co-operation and development
- OTC:
-
Over the counter
- TCM:
-
Traditional Chinese medicine
- WHO:
-
World Health Organization
References
Chen ST, Dou J, Temple R, Agarwal R, Wu K-M, Walker S (2008) New therapies from old medicines. Nat Biotechnol 26(10):1077–1083
Choi SM, Son SH, Yun SR, Kwon OW, Seon JH, Paek KY (2000) Pilot-scale culture of adventitious roots of ginseng in a bioreactor system. Plant Cell Tiss Org Cult 62(3):187–193
Daliu P, Santini A, Novellino E (2019) From pharmaceuticals to nutraceuticals: bridging disease prevention and management. Expert Rev Clin Pharmacol 12(1):1–7
Desrosiers MR, Weathers PJ (2016) Effect of leaf digestion and artemisinin solubility for use in oral consumption of dried Artemisia annua leaves to treat malaria. J Ethnopharmacol 190:313–318. https://doi.org/10.1016/j.jep.2016.06.041
Desrosiers MR, Weathers PJ (2018) Artemisinin permeability via Caco-2 cells increases after simulated digestion of Artemisia annua leaves. J Ethnopharmacol 210:254–259. https://doi.org/10.1016/j.jep.2017.08.038
Desrosiers MR, Mittelman A, Weathers PJ (2020) Dried leaf Artemisia annua improves bioavailability of artemisinin via cytochrome P450 inhibition and enhances artemisinin efficacy downstream. Biomolecules 10(2):254
Dou J, Beitz J, Temple R (2019) Development of plant-derived mixtures as botanical drugs: clinical considerations. In: Sasisekharan R, Lee S (eds) The science and regulations of naturally derived complex drugs. Springer, Cham, pp 245–264
Duke JA (2001) Handbook of phytochemical constituents of gras herbs and other economic plants. CRC Press, Boca Raton
Farrar MC, Jacobs TF (2020) Paclitaxel. StatPearls Publishing, Treasure Island, FL
Fett-Neto AG, DiCosmo F, Reynolds W, Sakata K (1992) Cell culture of Taxus as a source of the antineoplastic drug taxol and related taxanes. Bio/technology 10(12):1572–1575
Gubser G, Vollenweider S, Eibl D, Eibl R (2021) Food ingredients and food made with plant cell and tissue cultures: state-of-the art and future trends. Eng Life Sci 21(3–4):87–98
Hoffman FA (2015) Botanicals as “new” drugs: US development. Epilepsy Behav 52:338–343
Lee SL, Dou J, Agarwal R, Temple R, Beitz J, Wu C, Mulberg A, Yu LX, Woodcock J (2015) Evolution of traditional medicines to botanical drugs. Science 347(6219):S32–S34
Martin VJ, Pitera DJ, Withers ST, Newman JD, Keasling JD (2003) Engineering a mevalonate pathway in Escherichia coli for production of terpenoids. Nat Biotechnol 21(7):796–802
McChesney J, Dou J, Harrington P (2019) The development of botanical drugs–a review. Pharmaceut Reg Aff 8(2):2
Mohinudeen IK, Kanumuri R, Soujanya K, Shaanker RU, Rayala SK, Srivastava S (2021) Sustainable production of camptothecin from an Alternaria sp. isolated from Nothapodytes nimmoniana. Sci Rep 11(1):1–11
Moudi M, Go R, Yien CYS, Nazre M (2013) Vinca alkaloids. Int J Prev Med 4(11):1231
Newman DJ, Cragg GM (2020) Natural products as sources of new drugs over the nearly four decades from 01/1981 to 09/2019. J Nat Prod 83(3):770–803
Paek K-Y, Murthy HN, Hahn E-J, Zhong J-J (2009) Large scale culture of ginseng adventitious roots for production of ginsenosides. In: Zhong JJ, Bai FW (eds) Biotechnology in China I. Springer, Berlin, pp 151–176
Peplow M (2016) Synthetic biology’s first malaria drug meets market resistance. Nat News 530(7591):389
Ro D-K, Paradise EM, Ouellet M, Fisher KJ, Newman KL, Ndungu JM, Ho KA, Eachus RA, Ham TS, Kirby J (2006) Production of the antimalarial drug precursor artemisinic acid in engineered yeast. Nature 440(7086):940–943
Sorkin BC, Kuszak AJ, Bloss G, Fukagawa NK, Hoffman FA, Jafari M, Barrett B, Brown PN, Bushman FD, Casper SJ (2020) Improving natural product research translation: from source to clinical trial. FASEB J 34(1):41–65
Wall ME, Wani MC (1996) Camptothecin and taxol: from discovery to clinic. J Ethnopharmacol 51(1–3):239–254
Weathers PJ, Arsenault PR, Covello PS, McMickle A, Teoh KH, Reed DW (2011) Artemisinin production in Artemisia annua: studies in planta and results of a novel delivery method for treating malaria and other neglected diseases. Phytochem Rev 10(2):173–183
Wetzstein HY, Porter JA, Janick J, Ferreira JF, Mutui TM (2018) Selection and clonal propagation of high artemisinin genotypes of Artemisia annua. Front Plant Sci 9:358
Wu C, Lee S-L, Taylor C, Li J, Chan Y-M, Agarwal R, Temple R, Throckmorton D, Tyner K (2020) Scientific and regulatory approach to botanical drug development: a US FDA Perspective. J Nat Prod 83(2):552–562
Acknowledgements
Authors gratefully acknowledge our respective organizations for supporting our time and effort involved in this academic endeavor.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
JD—wrote article; edited article; corresponding author on regulatory questions. PW—wrote article; edited article; corresponding author overall and on in vitro production questions.
Corresponding authors
Ethics declarations
Conflict of interest
The authors’ opinions are their own, and should not be interpreted as views and/or policies of their respective employers. Authors have no relevant financial or non-financial interests to disclose.
Additional information
Communicated by Christophe Hano.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dou, J., Weathers, P. Specialty molecules from plants and in vitro cultures as new drugs: regulatory considerations from flask to patient. Plant Cell Tiss Organ Cult 149, 105–111 (2022). https://doi.org/10.1007/s11240-022-02287-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11240-022-02287-4