Abstract
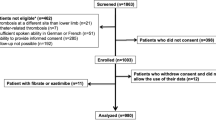
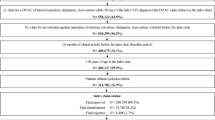
Statins were reported to have a potential effect of primary prevention of venous thromboembolism (VTE), although that of secondary prevention remains uncertain. To investigate the association between statins use and recurrent VTE in the current era. The COMMAND VTE Registry-2 is a multicenter registry enrolling 5,197 consecutive VTE patients among 31 centers in Japan between January 2015 and August 2020. We divided the entire cohort into 2 groups according to statins use at the time of discharge; the statins (N = 865) and no statins groups (N = 4332). The statins group was older (72.9 vs. 66.7 years, P < 0.001), and less often had active cancer (22.0% vs. 30.4%, P < 0.001). The cumulative incidence of discontinuation of anticoagulation was significantly lower in the statins group (60.3% vs. 52.6%, Log-rank P < 0.001). The cumulative 5-year incidence of recurrent VTE was significantly lower in the statins group (6.8% vs. 10.1%, Log-rank P = 0.01). Even after adjusting for the confounders, the lower risk of the statins group relative to the no statins group remained significant for recurrent VTE (HR 0.65, 95% CI 0.45–0.91, P = 0.01). The cumulative 5-year incidence of major bleeding was significantly lower in the statins group (12.2% vs. 14.1%, Log-rank P = 0.04), although, after adjusting for the confounders, the risk of the statins group relative to the no statins group turned to be insignificant (HR 0.77, 95% CI 0.59–1.00, P = 0.054). In this large real-world VTE registry, statins use was significantly associated with a lower risk for the recurrent VTE in the current era.
Graphical Abstract




Similar content being viewed by others
Data availability
The data, analytic methods, and study materials will not be made available to other researchers for purposes of reproducing the results or replicating the procedure. However, if the relevant review board or ethics committee approve data sharing and all investigators of the COMMAND VTE Registry-2 provide consent, the deidentified participant data will be shared on a request basis through the principal investigator. Study protocol will also be available. The data will be shared as Excel files via e-mail during the proposed investigation period.
Abbreviations
- CI:
-
Confidence interval
- DOAC:
-
Direct oral anticoagulant
- IOM:
-
Deep vein thrombosis
- HR:
-
Hazard ratio
- LDL:
-
Low-density lipoprotein
- PE:
-
Pulmonary embolism
- VTE:
-
Hazard ratio
References
Oleksiuk-Bójko M, Lisowska A (2023) Venous thromboembolism: why is it still a significant health problem? Adv Med Sci 68(1):10–20. https://doi.org/10.1016/j.advms.2022.10.002
Stevens SM, Woller SC, Kreuziger LB, Bounameaux H, Doerschug K, Geersing GJ et al (2021) Antithrombotic therapy for VTE Disease: second update of the CHEST Guideline and Expert Panel Report. Chest 160(6):e545–e608. https://doi.org/10.1016/j.chest.2021.07.055
Oesterle A, Laufs U, Liao JK (2017) Pleiotropic effects of statins on the Cardiovascular System. Circ Res 120:229–243. https://doi.org/10.1161/circresaha.116.308537
Undas A, Celińska-Löwenhoff M, Kaczor M, Musial J (2004) New nonlipid effects of statins and their clinical relevance in cardiovascular disease. Thromb Haemost 91:1065–1077. https://doi.org/10.1160/th04-02-0064
Undas A, Brummel-Ziedins KE, Mann KG (2005) Statins and blood coagulation. Arterioscler Thromb Vasc Biol. https://doi.org/10.1161/01.atv.0000151647.14923.ec. 25:287 – 94
Biedermann JS, Kruip M, van der Meer FJ, Rosendaal FR, Leebeek FWG, Cannegieter SC et al (2018) Rosuvastatin use improves measures of coagulation in patients with venous thrombosis. Eur Heart J 39:1740–1747. https://doi.org/10.1093/eurheartj/ehy014
Violi F, Calvieri C, Ferro D, Pignatelli P (2013) Statins as antithrombotic drugs. Circulation 127:251–257. https://doi.org/10.1161/circulationaha.112.145334
Glynn RJ, Danielson E, Fonseca FA, Genest J, Gotto AM Jr., Kastelein JJ et al (2009) A randomized trial of rosuvastatin in the prevention of venous thromboembolism. N Engl J Med 360:1851–1861. https://doi.org/10.1056/nejmoa0900241
Kunutsor SK, Seidu S, Khunti K (2017) Statins and primary prevention of venous thromboembolism a systematic review and meta-analysis. Lancet Haematol 4:e83–e93. https://doi.org/10.1016/s2352-3026(16)30184-3
Biere-Rafi S, Hutten BA, Squizzato A, Ageno W, Souverein PC, de Boer A et al (2013) Statin treatment and the risk of recurrent pulmonary embolism. Eur Heart J 34:1800–1806. https://doi.org/10.1093/eurheartj/eht046
Tagalakis V, Eberg M, Kahn S, Azoulay L (2016) Use of statins and reduced risk of recurrence of VTE in an older population. A population-based cohort study. Thromb Haemost 115:1220–1228. https://doi.org/10.1160/th15-10-0775
Yoshikawa Y, Yamashita Y, Morimoto T, Mabuchi H, Amano H, Takase T et al (2020) Effect of statins on recurrent venous thromboembolism (from the COMMAND VTE Registry). Am J Cardiol 125:189–197. https://doi.org/10.1016/j.amjcard.2019.10.011
Delluc A, Tromeur C, Le Moigne E, Nowak E, Mottier D, Le Gal G et al (2012) Lipid lowering drugs and the risk of recurrent venous thromboembolism. Thromb Res 130:859–863. https://doi.org/10.1016/j.thromres.2012.08.296
Brækkan SK, Caram-Deelder C, Siegerink B, van Hylckama Vlieg A, le Cessie S, Rosendaal FR et al (2017) Statin use and risk of recurrent venous thrombosis: results from the MEGA follow-up study. Res Pract Thromb Haemost 1:112–119. https://doi.org/10.1002/rth2.12003
Kaneda K, Yamashita Y, Morimoto T, Chatani R, Nishimoto Y, Ikeda N et al (2023) Anticoagulation strategies and long-term recurrence in patients with venous thromboembolism in the era of direct oral anticoagulants. Eur J Intern Med 118:59–72. https://doi.org/10.1016/j.ejim.2023.08.007
Büller HR, Décousus H, Grosso MA, Mercuri M, Middeldorp S, Prins MH et al (2013) Edoxaban versus warfarin for the treatment of symptomatic venous thromboembolism. N Engl J Med 369:1406–1415. https://doi.org/10.1056/nejmoa1306638
Schulman S, Kearon C (2005) Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost 3:692–694. https://doi.org/10.1111/j.1538-7836.2005.01204.x
Yamashita Y, Morimoto T, Amano H, Takase T, Hiramori S, Kim K et al (2018) Anticoagulation therapy for venous thromboembolism in the Real World - from the COMMAND VTE Registry. Circ J: Official J Japanese Circulation Soc 82:1262–1270. https://doi.org/10.1253/circj.cj-17-1128
Konstantinides SV, Meyer G, Becattini C, Bueno H, Geersing GJ, Harjola VP et al (2020) 2019 ESC guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J 41:543–603. https://doi.org/10.1093/eurheartj/ehz405
Stevens SM, Woller SC, Kreuziger LB, Bounameaux H, Doerschug K, Geersing GJ et al (2021) Antithrombotic therapy for VTE Disease: second update of the CHEST Guideline and Expert Panel Report. Chest 160:e545–e608. https://doi.org/10.1016/j.chest.2021.07.055
Yamashita Y, Morimoto T, Amano H, Takase T, Hiramori S, Kim K et al (2018) Influence of baseline platelet count on outcomes in patients with venous thromboembolism (from the COMMAND VTE Registry). Am J Cardiol 122:2131–2141. https://doi.org/10.1016/j.amjcard.2018.08.053
Jaff MR, McMurtry MS, Archer SL, Cushman M, Goldenberg N, Goldhaber SZ et al (2011) Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension: a scientific statement from the American Heart Association. Circulation 123:1788–1830. https://doi.org/10.1161/cir.0b013e318214914f
Ando MFI, Ito M, Kobayashi T, Masuda M, Miyahara Y, Nakanishi N et al (2011) Guidelines for the diagnosis, treatment and prevention of pulmonary thromboembolism and deep vein thrombosis (JCS 2009). Circ J: Official J Japanese Circulation Soc 75:1258–1281. https://doi.org/10.1253/circj.cj-88-0010
Joseph P, Glynn R, Lonn E, Ramasundarahettige C, Eikelboom J, MacFadyen J et al (2022) Rosuvastatin for the prevention of venous thromboembolism: a pooled analysis of the HOPE-3 and JUPITER randomized controlled trials. Cardiovasc Res 118:897–903. https://doi.org/10.1093/cvr/cvab078
Ageno W, Becattini C, Brighton T, Selby R, Kamphuisen PW (2008) Cardiovascular risk factors and venous thromboembolism: a meta-analysis. Circulation 117:93–102. https://doi.org/10.1161/circulationaha.107.709204
Zaccardi F, Kunutsor SK, Seidu S, Davies MJ, Khunti K (2018) Is the lower risk of venous thromboembolism with statins related to low-density-lipoprotein reduction? A network meta-analysis and meta-regression of randomised controlled trials. Atherosclerosis 271:223–231. https://doi.org/10.1016/j.atherosclerosis.2018.02.035
Arshad N, Bjøri E, Hindberg K, Isaksen T, Hansen JB, Braekkan SK (2017) Recurrence and mortality after first venous thromboembolism in a large population-based cohort. J Thromb Haemost 15:295–303. https://doi.org/10.1111/jth.13587
Heit JA, Spencer FA, White RH (2016) The epidemiology of venous thromboembolism. J Thromb Thrombolysis 41:3–14. https://doi.org/10.1007/s11239-015-1311-6
Kronenberg RM, Beglinger S, Stalder O, Méan M, Limacher A, Beer JH et al (2019) Statin therapy and recurrent venous thromboembolism in the elderly: a prospective cohort study. Sci Rep 9:14804. https://doi.org/10.1038/s41598-019-51374-8
Kunutsor SK, Seidu S, Khunti K (2017) Statins and secondary prevention of venous thromboembolism: pooled analysis of published observational cohort studies. Eur Heart J 38:1608–1612
Zhu H, Zheng H, Xu T, Liu X, Liu X, Sun L et al (2022) Effects of statins in primary and secondary prevention for venous thromboembolism events: a meta analysis. Vascul Pharmacol 142:106931. https://doi.org/10.1093/eurheartj/ehx107
Li R, Yuan M, Yu S, Fu W, Yu W, Ling S et al (2021) Effect of statins on the risk of recurrent venous thromboembolism: a systematic review and meta-analysis. Pharmacol Res 165:105413. https://doi.org/10.1016/j.phrs.2020.105413
Hemkens LG, Benchimol EI, Langan SM, Briel M, Kasenda B, Januel JM et al (2016) The reporting of studies using routinely collected health data was often insufficient. J Clin Epidemiol 79:104–111. https://doi.org/10.1016/j.jclinepi.2016.06.005
Chaffey P, Thompson M, Pai AD, Tafreshi AR, Tafreshi J, Pai RG (2018) Usefulness of statins for Prevention of venous thromboembolism. Am J Cardiol 121:1436–1440. https://doi.org/10.1016/j.amjcard.2018.02.024
Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM Jr., Kastelein JJ et al (2008) Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 359:2195–2207. https://doi.org/10.1056/nejmoa0807646
Fulcher J, O’Connell R, Voysey M, Emberson J, Blackwell L, Mihaylova B et al (2015) Efficacy and safety of LDL-lowering therapy among men and women: meta-analysis of individual data from 174,000 participants in 27 randomised trials. Lancet (London England) 385:1397–1405. https://doi.org/10.1016/s0140-6736(14)61368-4
Ridker PM, Miletich JP, Hennekens CH, Buring JE (1997) Ethnic distribution of factor V Leiden in 4047 men and women. Implications for venous thromboembolism screening. JAMA 277(16):1305–1307. https://jamanetwork.com/journals/jama/article-abstract/415610
Acknowledgements
The authors appreciate the support and collaboration of the coinvestigators participating in the COMMAND VTE Registry-2.
Funding
The COMMAND VTE Registry-2 is partially supported by JSPS KAKENHI (grant number: JP21K16022). The research funding body had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Research involving human participants and/or animals
The current study was conducted in accordance with the principles of the Declaration of Helsinki. We further confirm that any aspect of the work covered in this manuscript that has involved either experimental animals or human patients has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript.
Informed consent
Written informed consent from each patient was waived, because we used clinical information obtained in routine clinical practice. This method is concordant with the guidelines for epidemiological studies issued by the Ministry of Health, Labor, and Welfare in Japan.
Conflicts of interest
Dr. Yamashita received lecture fees from Bayer Healthcare, Bristol-Myers Squibb, Pfizer, and Daiichi-Sankyo and grant support from Bayer Healthcare and Daiichi-Sankyo. Dr. Morimoto reports lecture fees from Bristol-Myers Squibb, Daiichi Sankyo, Japan Lifeline, Kowa, Kyocera, Novartis, and Toray and manuscript fees from Bristol-Myers Squibb and Kowa; he was on the advisory board for Sanofi. Dr. Kaneda received lecture fees from Bristol-Myers Squibb, Pfizer, and Daiichi-Sankyo. Dr. Nishimoto received lecture fees from Bayer Healthcare, Bristol-Myers Squibb, Pfizer, and Daiichi-Sankyo. Dr. Ikeda N. received lecture fees from Bayer Healthcare, Bristol-Myers Squibb, and Daiichi-Sankyo. Dr. Ikeda S. received lecture fees from Bayer Healthcare, Bristol-Myers Squibb and Daiichi-Sankyo. Dr. Ogihara received research funding from Bayer Healthcare. Dr. Koitabashi received lecture fees from Bayer Healthcare and grant support from Pfizer. All other authors reported that they have no relationships relevant to the contents of this paper to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mabuchi, H., Nishikawa, R., Yamashita, Y. et al. Statins use and recurrent venous thromboembolism in the direct oral anticoagulant era: insight from the COMMAND VTE Registry-2. J Thromb Thrombolysis (2024). https://doi.org/10.1007/s11239-024-03002-0
Accepted:
Published:
DOI: https://doi.org/10.1007/s11239-024-03002-0