Abstract
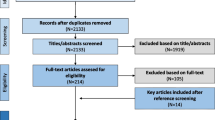
Cardiovascular risk is increased in patients with autoimmune rheumatic diseases. Endothelial, erythrocyte and platelet microvesicles (MVs) are elevated in patients with cardiovascular diseases and represent novel markers of endothelial dysfunction and thromboinflammation. We tested whether their levels are increased in patients with autoimmune rheumatic diseases (ARDs) in the absence of disease flare and cardiovascular comorbidities. Well-controlled patients with rheumatoid arthritis or systemic lupus erythematosus were studied, provided they were free from cardiovascular comorbidities and established cardiovascular disease. We additionally studied (a) a control group consisting of healthy volunteers and (b) a reference group including patients with stable coronary artery disease (CAD). MVs were measured using a standardized flow cytometry protocol. In a population of 74 participants, patients with ARDs (n = 17) presented increased levels of both endothelial (283.3 ± 195.0/μL vs 168.5 ± 54.8/μL, p = 0.029) and platelet MVs (374.0 ± 275.3/μL vs 225.7 ± 101.1/μL, p = 0.046) compared to controls (n = 34), whereas erythrocyte MVs did not significantly differ. In addition, patients with ARDs showed similar levels of endothelial MVs compared to CAD patients (n = 23) (283.3 ± 195.0/μL vs 297.0 ± 211.8/μL, p = 0.846). Platelet MVs were significantly associated with disease duration, and erythrocyte MVs with patients’ perceived disease activity. In conclusion, increased levels of endothelial and platelet MVs may be evident in patients with ARDs, even in the absence of disease flares and before the establishment of cardiovascular complications. Levels of endothelial MVs resemble those of patients with profound atherothrombotic profile. The prognostic potential of MVs in terms of cardiovascular disease prevention warrants further investigation in patients with ARDs.

Similar content being viewed by others
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
Anyfanti P, Gavriilaki E, Douma S, Gkaliagkousi E (2020) Endothelial dysfunction in patients with rheumatoid arthritis: the role of hypertension. Curr Hypertens Rep 22:56
Anyfanti P, Triantafyllou A, Gkaliagkousi E et al (2017) Subendocardial viability ratio in patients with rheumatoid arthritis: comparison with healthy controls and identification of prognostic factors. Clin Rheumatol 36:1229–1236. https://doi.org/10.1007/s10067-017-3659-9
Anyfanti P, Triantafyllou A, Gkaliagkousi E et al (2017) Retinal vessel morphology in rheumatoid arthritis: association with systemic inflammation, subclinical atherosclerosis and cardiovascular risk. Microcirculation. https://doi.org/10.1111/micc.12417
Anyfanti P, Gkaliagkousi E, Triantafyllou A et al (2018) Dermal capillary rarefaction as a marker of microvascular damage in patients with rheumatoid arthritis: association with inflammation and disorders of the macrocirculation. Microcirculation 25:e12451. https://doi.org/10.1111/micc.12451
Koletsos N, Gkaliagkousi E, Lazaridis A et al (2021) Skin microvascular dysfunction in patients with systemic lupus erythematosus with and without cardiovascular risk factors. Rheumatology 60:2834–2841. https://doi.org/10.1093/rheumatology/keaa722
Gkaliagkousi E, Gavriilaki E, Triantafyllou A, Douma S (2015) Clinical significance of endothelial dysfunction in essential hypertension. Curr Hypertens Rep. https://doi.org/10.1007/s11906-015-0596-3
Van Es N, Bleker S, Sturk A, Nieuwland R (2015) Clinical significance of tissue factor-exposing microparticles in arterial and venous thrombosis. Semin Thromb Hemost 41:718–727. https://doi.org/10.1055/s-0035-1556047
Lipets EN, Antonova OA, Shustova ON et al (2020) Use of Thrombodynamics for revealing the participation of platelet, erythrocyte, endothelial, and monocyte microparticles in coagulation activation and propagation. PLoS One 15:e0227932. https://doi.org/10.1371/journal.pone.0227932
Gkaliagkousi E, Gavriilaki E, Vasileiadis I et al (2019) Endothelial microvesicles circulating in peripheral and coronary circulation are associated with central blood pressure in coronary artery disease. Am J Hypertens 32:1199–1205. https://doi.org/10.1093/ajh/hpz116
Gkaliagkousi E, Nikolaidou B, Gavriilaki E et al (2019) Increased erythrocyte- and platelet-derived microvesicles in newly diagnosed type 2 diabetes mellitus. Diabetes Vasc Dis Res 16:458–465. https://doi.org/10.1177/1479164119844691
Gkaliagkousi E, Gavriilaki E, Yiannaki E et al (2021) Platelet microvesicles are associated with the severity of coronary artery disease: comparison between peripheral and coronary circulation. J Thromb Thrombolysis. https://doi.org/10.1007/s11239-020-02302-5
Ridger VC, Boulanger CM, Angelillo-Scherrer A et al (2017) Microvesicles in vascular homeostasis and diseases. Thromb Haemost 117:1296–1316. https://doi.org/10.1160/th16-12-0943
Bruce B, Fries JF (2005) The health assessment questionnaire (HAQ). Clin Exp Rheumatol 23(5 Suppl 39):S14-8
World Medical Association (2013) World medical association declaration of helsinki: ethical principles for medical research involving human subjects. JAMA 310:2191–2194. https://doi.org/10.1001/jama.2013.281053
Bordy R, Totoson P, Prati C et al (2018) Microvascular endothelial dysfunction in rheumatoid arthritis. Nat Rev Rheumatol 14:404–420. https://doi.org/10.1038/s41584-018-0022-8
Frangou E, Chrysanthopoulou A, Mitsios A et al (2019) REDD1_autophagy pathway promotes thromboinflammation and fibrosis in human systemic lupus erythematosus (SLE). Ann Rheum Dis 78:238–248
Kambas K, Chrysanthopoulou A, Vassilopoulos D et al (2013) Tissue factor expression in neutrophil extracellular traps and neutrophil derived microparticles in antineutrophil cytoplasmic antibody associated vasculitis may promote thromboinflammation and the thrombophilic state associated with the disease. Ann Rheum Dis 73:1854–1863
Rodríguez-Carrio J, Alperi-López M, López P et al (2015) Altered profile of circulating microparticles in rheumatoid arthritis patients. Clin Sci 128:437–448. https://doi.org/10.1042/CS20140675
Pamuk GE, Vural Ö, Turgut B et al (2008) Increased platelet activation markers in rheumatoid arthritis: are they related with subclinical atherosclerosis? Platelets 19:146–154. https://doi.org/10.1080/09537100701210057
Gitz E, Pollitt AY, Gitz-francois JJ et al (2016) CLEC-2 expression is maintained on activated platelets and on platelet microparticles. Blood 124:2262–2271. https://doi.org/10.1182/blood-2014-05-572818.The
Knijff-Dutmer EAJ, Koerts J, Nieuwland R et al (2002) Elevated levels of platelet microparticles are associated with disease activity in rheumatoid arthritis. Arthritis Rheum 46:1498–1503. https://doi.org/10.1002/art.10312
Pereira J, Alfaro G, Goycoolea M et al (2006) Circulating platelet-derived microparticles in systemic lupus erythematosus. Thromb Haemost 95:94–99. https://doi.org/10.1160/th05-05-0310
Sellam J, Proulle V, Jüngel A et al (2009) Increased levels of circulating microparticles in primary Sjögren’s syndrome, systemic lupus erythematosus and rheumatoid arthritis and relation with disease activity. Arthritis Res Ther 11:1–11. https://doi.org/10.1186/ar2833
Nielsen CT, Østergaard O, Johnsen C et al (2011) Distinct features of circulating microparticles and their relationship to clinical manifestations in systemic lupus erythematosus. Arthritis Rheum 63:3067–3077. https://doi.org/10.1002/art.30499
Erdbruegger U, Grossheim M, Hertel B et al (2008) Diagnostic role of endothelial microparticles in vasculitis. Rheumatology 47:1820–1825. https://doi.org/10.1093/rheumatology/ken373
Brogan PA, Shah V, Brachet C et al (2004) Endothelial and platelet microparticles in vasculitis of the young. Arthritis Rheum 50:927–936. https://doi.org/10.1002/art.20199
Bartoloni E, Alunno A, Bistoni O et al (2015) Characterization of circulating endothelial microparticles and endothelial progenitor cells in primary Sjögren’s syndrome: new markers of chronic endothelial damage? Rheumatol (United Kingdom) 54:536–544. https://doi.org/10.1093/rheumatology/keu320
López P, Rodríguez-Carrio J, Martínez-Zapico A et al (2017) Circulating microparticle subpopulations in systemic lupus erythematosus are affected by disease activity. Int J Cardiol 236:138–144. https://doi.org/10.1016/j.ijcard.2017.02.107
Funding
This research is co-financed by Greece and the European Union (European Social Fund- ESF) through the Operational Programme “Human Resources Development, Education and Lifelong Learning 2014–2020” in the context of the project “Evaluation of novel markers of endothelial dysfunction and thrombotic microenvironment in patients with rheumatoid arthritis: association with markers of subclinical inflammation and cardiovascular damage (MIS 5047870)”. Authors funded: PA, EGa, MD, EGk.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Anyfanti, P., Gavriilaki, E., Nikolaidou, B. et al. Patients with autoimmune chronic inflammatory diseases present increased biomarkers of thromboinflammation and endothelial dysfunction in the absence of flares and cardiovascular comorbidities. J Thromb Thrombolysis 53, 10–16 (2022). https://doi.org/10.1007/s11239-021-02517-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-021-02517-0