Abstract
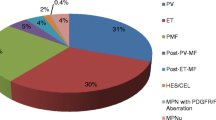
Arterial thrombosis is a common complication in patients with Ph− myeloproliferative neoplasms (MPN). We searched for the risk factors of stroke in MPN patients from anagrelide registry. We analyzed the potential risk factors triggering a stroke/TIA event in 249 MPN patients with previous stroke (n = 168) or Transient Ischemic Attack (TIA) (n = 140), and in 1,193 MPN control subjects (without clinical history of thrombosis). These patients were registered in a prospective manner, providing a follow-up period after Anagrelide treatment. The median age of the patients in the experimental group was of 56 years of age (ranging from 34–76) and of 53 years of age (ranging from 26–74) in the control group (p < 0.001). Using a multivariate model, we determined the following as risk factors: JAK2V617F mutation (OR 2.106, 1.458–3.043, p = 0.006), age (OR 1.017/year, 1.005–1,029, p = 0.006), male gender (OR 1.419, 1.057–1.903, p = 0.020), MPN diagnosis (OR for PMF 0.649, 0.446–0.944, p = 0.024), BMI (OR 0.687 for BMI > 25, 0.473–0.999, p = 0.05) and high TAG levels (OR 1.734, 1.162–2.586, p = 0.008), all of which were statistically significant for CMP development. Concerning the risk factors for thrombophilia, only the antiphospholipid syndrome (OR 1.994, 1.017–3.91, p = 0.048) was noteworthy in a stroke-relevant context. There was no significant difference between the blood count of the patients prior to a stroke event and the control group, both of which were under a cytoreductive treatment. We found that age, male gender, JAK2V617F mutation, previous venous thrombosis, and hypertriglyceridemia represent independent risk factors for the occurrence of a stroke in Ph− MPN patients.
Similar content being viewed by others
Data availability
CZEMP organisation.
References
Muxi PJ, Oliver AC (2014) Jak-2 positive myeloproliferative neoplasms. Curr Treat Options Oncol 15:147–156. https://doi.org/10.1007/s11864-014-0279-3
Barbui T, Finazzi G, Carobbio A, Thiele J, Passamonti F, Rumi E, Ruggeri M, Rodeghiero F, Randi ML, Bertozzi I, Gisslinger H, Buxhofer-Ausch V, De Stefano V, Betti S, Rambaldi A, Vannucchi AM, Tefferi A (2012) Development and validation of an International Prognostic Score of thrombosis in World Health Organization-essential thrombocythemia (IPSET-thrombosis). Blood 120:5128–5133. https://doi.org/10.1182/blood-2012-07-444067
Schwarz J, Ovesna P, Cerna O, Kissova J, Maaloufova Soukupova J, Brychtova Y, Doubek M, Cervinek L, Cmunt E, Dulicek P, Campr V, Kren L, Penka M (2016) Thrombosis in thrombocythemic Ph- myeloproliferations is associated with higher platelet count prior to the event: results of analyses of prothrombotic risk factors from a registry of patients treated with anagrelide. Eur J Haematol 96:98–106. https://doi.org/10.1111/ejh.12554
Artoni A, Bucciarelli P, Martinelli I (2014) Cerebral thrombosis and myeloproliferative neoplasms. Curr Neurol Neurosci Rep 14:496. https://doi.org/10.1007/s11910-014-0496-y
Harrison CN, Bareford D, Butt N, Campbell P, Conneally E, Drummond M, Erber W, Everington T, Green AR, Hall GW, Hunt BJ, Ludlam CA, Murrin R, Nelson-Piercy C, Radia DH, Reilly JT, Van der Walt J, Wilkins B, McMullin MF (2010) Guideline for investigation and management of adults and children presenting with a thrombocytosis. Br J Haematol 149:352–375. https://doi.org/10.1111/j.1365-2141.2010.08122.x
Barbui T, Barosi G, Birgegard G, Cervantes F, Finazzi G, Griesshammer M, Harrison C, Hasselbalch HC, Hehlmann R, Hoffman R, Kiladjian JJ, Kroger N, Mesa R, McMullin MF, Pardanani A, Passamonti F, Vannucchi AM, Reiter A, Silver RT, Verstovsek S, Tefferi A (2011) Philadelphia-negative classical myeloproliferative neoplasms: critical concepts and management recommendations from European LeukemiaNet. J Clin Oncol 29:761–770. https://doi.org/10.1200/JCO.2010.31.8436
Schwarz J, Pytlik R, Doubek M, Brychtova Y, Dulicek P, Campr V, Kren L, Penka M (2006) Analysis of risk factors: the rationale of the guidelines of the Czech Hematological Society for diagnosis and treatment of chronic myeloproliferative disorders with thrombocythemia. Semin Thromb Hemost 32:231–245. https://doi.org/10.1055/s-2006-939434
Cortelazzo S, Viero P, Finazzi G, D'Emilio A, Rodeghiero F, Barbui T (1990) Incidence and risk factors for thrombotic complications in a historical cohort of 100 patients with essential thrombocythemia. J Clin Oncol 8:556–562. https://doi.org/10.1200/JCO.1990.8.3.556
Carobbio A, Thiele J, Passamonti F, Rumi E, Ruggeri M, Rodeghiero F, Randi ML, Bertozzi I, Vannucchi AM, Antonioli E, Gisslinger H, Buxhofer-Ausch V, Finazzi G, Gangat N, Tefferi A, Barbui T (2011) Risk factors for arterial and venous thrombosis in WHO-defined essential thrombocythemia: an international study of 891 patients. Blood 117:5857–5859. https://doi.org/10.1182/blood-2011-02-339002
Palandri F, Polverelli N, Catani L, Ottaviani E, Baccarani M, Vianelli N (2011) Impact of leukocytosis on thrombotic risk and survival in 532 patients with essential thrombocythemia: a retrospective study. Ann Hematol 90:933–938. https://doi.org/10.1007/s00277-010-1154-3
Radaelli F, Colombi M, Calori R, Zilioli VR, Bramanti S, Iurlo A, Zanella A (2007) Analysis of risk factors predicting thrombotic and/or haemorrhagic complications in 306 patients with essential thrombocythemia. Hematol Oncol 25:115–120. https://doi.org/10.1002/hon.816
Tefferi A, Thiele J, Orazi A, Kvasnicka HM, Barbui T, Hanson CA, Barosi G, Verstovsek S, Birgegard G, Mesa R, Reilly JT, Gisslinger H, Vannucchi AM, Cervantes F, Finazzi G, Hoffman R, Gilliland DG, Bloomfield CD, Vardiman JW (2007) Proposals and rationale for revision of the World Health Organization diagnostic criteria for polycythemia vera, essential thrombocythemia, and primary myelofibrosis: recommendations from an ad hoc international expert panel. Blood 110:1092–1097. https://doi.org/10.1182/blood-2007-04-083501
Schwarz J, Penka M, Campr V, Pospisilova D, Kren L, Novakova L, Bodzasova C, Brychtova Y, Cerna O, Dulicek P, Joniasova A, Kissova J, Koristek Z, Schutzova M, Vonke I, Walterova L (2011) Diagnosis and treatment of BCR/ABL-negative myeloproliferative diseases–principles and rationale of CZEMP recommendations. Vnitr Lek 57:189–213
Murphy S, Peterson P, Iland H, Laszlo J (1997) Experience of the Polycythemia Vera Study Group with essential thrombocythemia: a final report on diagnostic criteria, survival, and leukemic transition by treatment. Semin Hematol 34:29–39
Lee HS, Park LC, Lee EM, Lee SJ, Shin SH, Im H, Do KM, Kim EJ, Ye BJ, Song MK, Kim SH, Lee SM, Lee WS, Kim YS (2012) Incidence rates and risk factors for vascular events in patients with essential thrombocythemia: a multicenter study from Korea. Clin Lymphoma Myeloma Leukemia 12:70–75. https://doi.org/10.1016/j.clml.2011.10.002
Schneider AT, Pancioli AM, Khoury JC, Rademacher E, Tuchfarber A, Miller R, Woo D, Kissela B, Broderick JP (2003) Trends in community knowledge of the warning signs and risk factors for stroke. JAMA J Am Med Assoc 289:343–346
Nobel L, Mayo NE, Hanley J, Nadeau L, Daskalopoulou SS (2014) MyRisk_Stroke calculator: a personalized stroke risk assessment tool for the general population. J Clin Neurol 10:1–9. https://doi.org/10.3988/jcn.2014.10.1.1
Wolf PA, D'Agostino RB, Belanger AJ, Kannel WB (1991) Probability of stroke: a risk profile from the Framingham Study. Stroke 22:312–318
Pastuszak Z, Kozniewska E, Stepien A, Piusinska-Macoch A, Czernicki Z, Koszewski W (2018) Importance rating of risk factors of ischemic stroke in patients over 85 years old in the polish population. Neurol Neurochir Pol 52:88–93. https://doi.org/10.1016/j.pjnns.2017.11.007
Kjeldsen SE (2017) Hypertension and cardiovascular risk: general aspects. Pharmacol Res. https://doi.org/10.1016/j.phrs.2017.11.003
Sanchez-Inigo L, Navarro-Gonzalez D, Fernandez-Montero A, Pastrana-Delgado J, Martinez JA (2017) Risk of incident ischemic stroke according to the metabolic health and obesity states in the Vascular-Metabolic CUN cohort. Int J Stroke 12:187–191. https://doi.org/10.1177/1747493016672083
de Lau LM, Leebeek FW, de Maat MP, Koudstaal PJ, Dippel DW (2010) Screening for coagulation disorders in patients with ischemic stroke. Expert Rev Neurotherapeutics 10:1321–1329. https://doi.org/10.1586/ern.10.104
Kenet G, Lutkhoff LK, Albisetti M, Bernard T, Bonduel M, Brandao L, Chabrier S, Chan A, deVeber G, Fiedler B, Fullerton HJ, Goldenberg NA, Grabowski E, Gunther G, Heller C, Holzhauer S, Iorio A, Journeycake J, Junker R, Kirkham FJ, Kurnik K, Lynch JK, Male C, Manco-Johnson M, Mesters R, Monagle P, van Ommen CH, Raffini L, Rostasy K, Simioni P, Strater RD, Young G, Nowak-Gottl U (2010) Impact of thrombophilia on risk of arterial ischemic stroke or cerebral sinovenous thrombosis in neonates and children: a systematic review and meta-analysis of observational studies. Circulation 121:1838–1847. https://doi.org/10.1161/CIRCULATIONAHA.109.913673
Montanaro VV, Freitas DD, Ruiz MC, Cavalcanti EB, Marinho PB, Freitas MC, Oliveira EM (2017) Ischemic stroke in young adults: profile of SARAH Hospital Brasilia from 2008 to 2012. Neurologist 22:61–63. https://doi.org/10.1097/NRL.0000000000000110
Dulicek P, Ivanova E, Kostal M, Sadilek P, Beranek M, Zak P, Hirmerova J (2017) Analysis of risk factors of stroke and venous thromboembolism in females with oral contraceptives use. Clin Appl Thromb. https://doi.org/10.1177/1076029617727857
Cervera R (2017) Antiphospholipid syndrome. Thromb Res 151(1):S43–S47. https://doi.org/10.1016/S0049-3848(17)30066-X
Okuma H, Kitagawa Y (2013) Diagnosis and potential treatment of antiphospholipid syndrome-related mainly on ischemic stroke. Brain Nerve 65:1319–1332
Rahemtullah A, Van Cott EM (2007) Hypercoagulation testing in ischemic stroke. Arch Pathol Lab Med 131:890–901. https://doi.org/10.1043/1543-2165(2007)131[890:HTIIS]2.0.CO;2
Buxhofer-Ausch V, Steurer M, Sormann S, Schloegl E, Schimetta W, Gisslinger B, Ruckser R, Gastl G, Gisslinger H (2016) Influence of platelet and white blood cell counts on major thrombosis-analysis from a patient registry in essential thrombocythemia. Eur J Haematol 97:511–516. https://doi.org/10.1111/ejh.12759
Carobbio A, Finazzi G, Antonioli E, Guglielmelli P, Vannucchi AM, Delaini F, Guerini V, Ruggeri M, Rodeghiero F, Rambaldi A, Barbui T (2008) Thrombocytosis and leukocytosis interaction in vascular complications of essential thrombocythemia. Blood 112:3135–3137. https://doi.org/10.1182/blood-2008-04-153783
van Genderen PJ, Leenknegt H, Michiels JJ, Budde U (1996) Acquired von Willebrand disease in myeloproliferative disorders. Leuk Lymphoma 22(1):79–82. https://doi.org/10.3109/10428199609074364
Acknowledgements
This work was supported by grants MH CZ—DRO (UHHK, 00179906) and PROGRES Q40/08.
Funding
Supported by MH CZ- DRO (UHHK, 00179906) and PROGRES Q40/08.
Author information
Authors and Affiliations
Consortia
Contributions
All authors, except MK and PO, contributed to this Registry with the highest numbers of patients. JS, MP, PD, and PO designed the study. PO performed the statistical analyses. MK and PO wrote the manuscript, and PD made the final corrections.
Corresponding author
Ethics declarations
Conflict of interest
MK receives a speaker ‘s honoraria from Novartis, AOP Orphan Pharmaceuticals. JS has received speaker ‘s and consultancy honoraria from AOP Orphan Pharmaceuticals. MP receives speaker ‘s and consultancy honoraria from AOP Orphan Pharmaceuticals AG and Novartis. PD receives speaker’s and consultancy honoraria from AOP Orphan Pharmaceuticals. P.O. has no conflict of interests.
Informed consent
All authors read the manuscript and agree with its publication in the Journal of Thrombosis and Thrombolysis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Košťál, M., Schwarz, J., Ovesná, P. et al. Ph− myeloproliferative neoplasms and the related risk factors for stroke occurrence: Results from a registry of patients treated with Anagrelide. J Thromb Thrombolysis 51, 112–119 (2021). https://doi.org/10.1007/s11239-020-02175-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-020-02175-8