Abstract
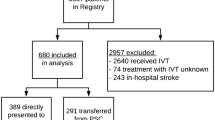
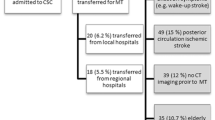
It is not known whether the current territorial organization for acute revascularization treatments in ischemic stroke patients guarantees similar time to treatment and functional outcomes among different levels of institutional stroke care. We aimed to assess the impact of time to treatment on functional outcomes in ischemic stroke patients who received intravenous thrombolysis (IVT) alone, bridging (IVT plus thrombectomy), or primary thrombectomy in level 1 and level 2 Stroke Units (SUs) in Triveneto, a geographical macroarea in Northeast of Italy. We conducted an analysis of data prospectively collected from 512 consecutive ischemic stroke patients who received IVT and/or mechanical thrombectomy in 25 SUs from September 17th to December 9th 2018. The favorable outcome measures were mRS score 0–1 and 0–2 at 3 months. The unfavorable outcome measures were mRS score 3–5 and death at 3 months. We estimated separately the possible association of each variable for time to treatment (onset-to-door, door-to-needle, onset-to-needle, door-to-groin puncture, needle-to-groin puncture, and onset-to-groin puncture) with 3-month outcome measures by calculating the odds ratios (ORs) with two-sided 95% confidence intervals (CI) after adjustment for pre-defined variables and variables with a probability value ≤ 0.10 in the univariate analysis for each outcome measure. Distribution of acute revascularization treatments was different between level 1 and level 2 SUs (p < 0.001). Among 182 patients admitted to level 1 SUs (n = 16), treatments were IVT alone in 164 (90.1%), bridging in 12 (6.6%), and primary thrombectomy in 6 (3.3%) patients. Among 330 patients admitted to level 2 SUs (n = 9), treatments were IVT alone in 219 (66.4%), bridging in 74 (22.4%), and primary thrombectomy in 37 (11.2%) patients. Rates of excellent outcome (51.4% vs 45.9%), favorable outcome (60.1% vs 58.7%), unfavorable outcome (33.3% vs 33.8%), and death (9.8% vs 11.3%) at 3 months were similar between level 1 and 2 SUs. No significant association was found between time to IVT alone (onset-to-door, door-to-needle, and onset-to-needle) and functional outcomes. After adjustment, door-to-needle time ≤ 60 min (OR 4.005, 95% CI 1.232–13.016), shorter door-to-groin time (OR 0.991, 95% CI 0.983–0.999), shorter needle-to-groin time (OR 0.986, 95% CI 0.975–0.997), and shorter onset-to-groin time (OR 0.994, 95% CI 0.988–1.000) were associated with mRS 0–1. Shorter door-to-groin time (OR 0.991, 95% CI 0.984–0.998), door-to-groin time ≤ 90 min (OR 12.146, 95% CI 2.193–67.280), shorter needle-to-groin time (OR 0.983, 95% CI 0.972–0.995), and shorter onset-to-groin time (OR 0.993, 95% CI 0.987–0.999) were associated with mRS 0–2. Longer door-to-groin time (OR 1.007, 95% CI 1.001–1.014) and longer needle-to-groin time (OR 1.019, 95% CI 1.005–1.034) were associated with mRS 3–5, while door-to-groin time ≤ 90 min (OR 0.229, 95% CI 0.065–0.808) was inversely associated with mRS 3–5. Longer onset-to-needle time (OR 1.025, 95% CI 1.002–1.048) was associated with death. Times to treatment influenced the 3-month outcomes in patients treated with thrombectomy (bridging or primary). A revision of the current territorial organization for acute stroke treatments in Triveneto is needed to reduce transfer time and to increase the proportion of patients transferred from a level 1 SU to a level 2 SU to perform thrombectomy.

Similar content being viewed by others
References
Stroke Unit Trialists’ Collaboration (2002) Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev 1:CD000197
Emberson J, Lees KR, Lyden P et al (2014) Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 384:1929–1935
Berkhemer OA, Fransen PS, Beumer D et al (2015) A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 372:11–20
Goyal M, Demchuk AM, Menon BK et al (2015) Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 372:1019–1030
Saver JL, Goyal M, Bonafe A et al (2015) Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 372:2285–2295
Campbell BC, Mitchell PJ, Kleinig TJ et al (2015) Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 372:1009–1018
Jovin TG, Chamorro A, Cobo E et al (2015) Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 372:2296–2306
Forlivesi S, Cappellari M, Baracchini C et al (2019) Intravenous thrombolysis for ischemic stroke in the Veneto region: the gap between eligibility and reality. J Thromb Thrombolysis 47:113–120
Bush CK, Kurimella D, Cross LJ et al (2016) Endovascular treatment with stent-retriever devices for acute ischemic stroke: a meta-analysis of randomized controlled trials. PLoS ONE 11:e0147287
Cappellari M, Mangiafico S, Saia V et al (2018) IER-START nomogram for prediction of three-month unfavorable outcome after thrombectomy for stroke. Int J Stroke 13:174749301876549
Lorenzano S, Ahmed N, Rosselli A et al (2010) Safe implementation of thrombolysis in stroke-monitoring study in Italy. Eur J Neurol 17(1):163–167
Waje-Andreassen U, Nabavi DG, Engelter ST et al (2018) European Stroke Organisation certification of stroke units and stroke centres. Eur Stroke J 3:220–226
Cappellari M, Turcato G, Forlivesi S et al (2018) The START nomogram for individualized prediction of the probability of unfavorable outcome after intravenous thrombolysis for stroke. Int J Stroke 13:700–706
Tsivgoulis G, Katsanos AH, Kadlecová P et al (2017) Intravenous thrombolysis for ischemic stroke in the golden hour: propensity-matched analysis from the SITS-EAST registry. J Neurol 264:912–920
Kim JT, Fonarow GC, Smith EE et al (2017) Treatment with tissue plasminogen activator in the golden hour and the shape of the 4.5-hour time-benefit curve in the National United States get with the guidelines-stroke population. Circulation 135:128–139
Saver JL, Goyal M, van der Lugt A et al (2016) Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA 316:1279–1288
Powers WJ, Rabinstein AA, Ackerson T et al (2018) 2018 Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 49:e46–e110
Acknowledgements
We thank all Collaborators for data collection in the SUs of Triveneto.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception/design and data collection. Analysis was performed by Manuel Cappellari. The first draft of the manuscript was written by Manuel Cappellari and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cappellari, M., Bonetti, B., Forlivesi, S. et al. Acute revascularization treatments for ischemic stroke in the Stroke Units of Triveneto, northeast Italy: time to treatment and functional outcomes. J Thromb Thrombolysis 51, 159–167 (2021). https://doi.org/10.1007/s11239-020-02142-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-020-02142-3