Abstract
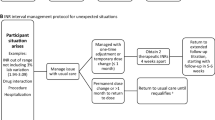
Guidelines suggest restarting warfarin at known maintenance doses, although this may result in a delay to achieving therapeutic anticoagulation. As such, we compared the time to achieve an INR ≥ 2.0 between those restarting warfarin maintenance vs loading doses after transient interruption, and the impact on protein C, S and factor II levels. Patients requiring interruption of warfarin for elective procedures without hospitalization were randomized 1:1 to receive warfarin maintenance or loading doses (1.5 times the maintenance dose for 3 days followed by pre-procedural warfarin maintenance dosing). Protein C, S and Factor II were drawn at baseline (prior to warfarin interruption), 7 and 14 days after restarting warfarin. Among 19 patients randomized to maintenance and 20 to loading doses, nearly half in each group had mechanical heart valves with gastrointestinal endoscopic procedures most commonly performed (41%). The median number of days to reach an INR ≥ 2.0 was 7.8 days in the loading and 9.0 in the maintenance group (difference between medians 1.2 days, 95% CI −3.1 to 4.9; P = 0.19). Although levels of protein C, S and factor II were lower in the loading vs maintenance dose group, all remained above that of baseline. Warfarin resumption with loading doses shortened the time to achieve a therapeutic INR by a median of 1.2 days. Prompt warfarin dose escalation should be done in response to the INR. Protein C and S remained above pre-warfarin interruption levels, implying a lack of depletion with restarting warfarin.



Similar content being viewed by others
References
Ansell J, Hirsh J, Hylek E, Jacobson A, Crowther M, Palareti G (2008) Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians evidence-based clinical practice guidelines (8th edn). Chest 133(Suppl 6):160S–198S. doi:10.1378/chest.08-0670
Siegal D, Yudin J, Kaatz S, Douketis JD, Lim W, Spyropoulos AC (2012) Periprocedural heparin bridging in patients receiving vitamin K antagonists: systematic review and meta-analysis of bleeding and thromboembolic rates. Circulation 126:1630–1639. doi:10.1161/CIRCULATIONAHA.112.105221
Keeling DM, Baglin T, Tait C, Watson H, Perry D, Baglin C, Kitchen S, Makris M (2011) Guidelines on oral anticoagulation with warfarin - fourth edition. Br J Haematol 154:311–324. doi:10.1111/j.1365-2141.2011.08753.x
Schultz KT, Bungard TJ (2011) Dosing options for decreasing the time to achieve therapeutic anticoagulation when reinitiating warfarin: a case series. Pharmacotherapy 31:793–805. doi:10.1592/phco.31.8.793
Weiss P, Soff GA, Halkin H, Seligsohn U (1987) Decline of proteins C and S and factors II, VII, IX and X during the initiation of warfarin therapy. Thromb Res 45:783–790. doi:10.1016/0049-3848(87)90088-0
Viganò S, Mannucci PM, Solinas S, Bottasso B, Mariani G (1984) Decrease in protein C antigen and formation of an abnormal protein soon after starting oral anticoagulant therapy. Br J Haematol 57:213–220. doi:10.1111/j.1365-2141.1984.tb02889.x
Holm J, Berntorp E, Carlsson R, Erhardt L (1993) Low-dose warfarin decreases coagulability without affecting prothrombin complex activity. J Intern Med 234:303–308
Bungard TJ, Archer SL, Hamilton P, Ritchie B, Tymchak W, Tsuyuki RT (2006) Bringing the benefits of anticoagulation management services to the community: Alberta program may serve as a model of care. Can Pharm J/Rev Des Pharm Du Canada 139:58–64. doi:10.1177/171516350613900207
Rosendaal FR, Cannegieter SC, van der Meer FJ, Briët E (1993) A method to determine the optimal intensity of oral anticoagulant therapy. Thromb Haemost 69:236–239
DiCiccio tj (1996) Efron e. Bootstrap confidence intervals. Stat Sci 11:189–228. doi:10.1214/ss/1032280214
Schulman S, Hwang HG, Eikelboom JW, Kearon C, Pai M, Delaney J (2014) Loading dose vs. maintenance dose of warfarin for reinitiation after invasive procedures: a randomized trial. J Thromb Haemost 12:1254–1259. doi:10.1111/jth.12613
Raskob ge, George JN (1997) Thrombotic complications of antithrombotic therapy: a paradox with implications for clinical practice. Ann Intern Med 127:839–841
Stirling Y (1995) Warfarin-induced changes in procoagulant and anticoagulant proteins. Blood Coagul Fibrinolysis 6:361–373. http://www.ncbi.nlm.nih.gov/pubmed/8589201
Nakashima MO, Rogers HJ (2014) Hypercoagulable states: an algorithmic approach to laboratory testing and update on monitoring of direct oral anticoagulants. Blood Res 49:85–94. doi:10.5045/br.2014.49.2.85
Amin A, Deitelzweig S, Jing Y, Makenbaeva D, Wiederkehr D, Lin J, Graham J (2014) Estimation of the impact of warfarin’s time-in-therapeutic range on stroke and major bleeding rates and its influence on the medical cost avoidance associated with novel oral anticoagulant use-learnings from ARISTOTLE, ROCKET-AF, and RE-LY trials. J Thromb Thrombolysis 38:150–159. doi:10.1007/s11239-013-1048-z
Funding
Peer reviewed funding was received through the University Hospital Foundation Medical Research Competition, Office of Research, Faculty of Medicine and Dentistry, University of Alberta. Pfizer, Canada supplied dalteparin (Fragmin™) prefilled syringes for use in this research study. The sponsors had no role in the conduct of this research, the collection, analysis and interpretation of data; in writing the report nor the decision to submit the article for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
TJB has received honoraria for an advisory board for BMS-Pfizer and Boehringer Ingelheim, as well as honoraria for speaking from Bayer. TJB has received unrestricted grants from BMS Pfizer and Bayer. JM has nothing to disclose. BR has served on advisory boards, given sponsored lectures using his own slides and received travel expense remuneration for Bayer, Baxter, Beohringer-Ingelheim, CSL-Behring, Pfizer, Sanofi, Servier and Shire. In lieu of honoraria for these activities, the companies have given financial contributions to the University of Alberta. BR reports grants from Novo Nordisk, CSL-Behring and Baxter, all outside of this submitted work.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Bungard, T.J., Mutch, J. & Ritchie, B. A randomized trial of restarting warfarin at maintenance versus loading doses following an elective procedure. J Thromb Thrombolysis 44, 507–515 (2017). https://doi.org/10.1007/s11239-017-1553-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-017-1553-6