Abstract
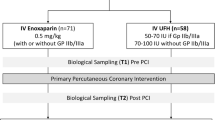
Our objective was to determine the association of activated partial thromboplastin time (aPTT) with recurrent ischemic events and non-coronary artery bypass surgery-related thrombolysis in myocardial infarction major bleeding. We studied 4,985 patients with high-risk non-ST-segment elevation acute coronary syndromes (NSTE ACS) participating in SYNERGY, a prospective, randomized, international trial designed to emulate contemporary practice wherein unfractionated heparin (UFH) is given intravenously and titrated according to a weight-adjusted dosing nomogram to a target aPTT of 1.5–2 times the upper limit of normal (approximately 50–70 s). Aspirin was administered to 95% of patients, clopidogrel to 63%, and glycoprotein IIb/IIIa receptor inhibitors to 58%. More than 90% of patients underwent early coronary angiography, and 69% were revascularized. Used as a time-dependent covariate, aPTT was evaluated as a predictor of time to ischemic or major hemorrhagic events in proportional hazards regression models. Using discrete variable analysis, aPTT was categorized as persistently below a lower threshold of anticoagulation (<50 vs. ≥50 s) for recurrent ischemic events and above an upper threshold (>70 vs. ≤70 s) for major hemorrhagic events. UFH treatment lasted a median of 42 (30, 78) h. At >6–12 (n = 3,021), >12–24 (n = 3,406), and >24–48 (n = 2,497) h, 34, 41, and 46% of patients achieved the target aPTT range, respectively. Both before and after adjusting for baseline predictors of anticoagulant response and risk score (age, hypertension, diabetes, smoking, ST depression, and renal function), no significant relationship between aPTT values and recurrent ischemic events or major bleeding was found. No relationship was observed between clinical outcomes and aPTT values persistently above or below the designated thresholds. Measurements of aPTT were not associated with clinical outcomes among patients with NSTE ACS treated with UFH. The required intensity of anticoagulation for benefit may be relatively modest when UFH is administered concomitantly with dual or triple platelet-directed therapy, particularly in patients undergoing early coronary revascularization.


Similar content being viewed by others
References
Anderson JL, Adams CD, Antman EM et al (2007) ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to revise the 2002 Guidelines for the Management of Patients with Unstable Angina/Non-ST-Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons; endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. J Am Coll Cardiol 50:e1–e157
Anand SS, Yusuf S, Pogue J et al (2003) Relationship of activated partial thromboplastin time to coronary events and bleeding in patients with acute coronary syndromes who receive heparin. Circulation 107:2884–2888
Gilchrist IC, Berkowitz SD, Thompson TD et al (2002) Heparin dosing and outcome in acute coronary syndromes: the GUSTO-IIb experience. Am Heart J 144:73–80
Granger CB, Hirsh J, Califf RM et al (1996) Activated partial thromboplastin time and outcome after thrombolytic therapy for acute myocardial infarction. Results from the GUSTO-I trial. Circulation 93:870–878
SYNERGY Executive Committee (2002) The SYNERGY trial: study design and rational. Am Heart J 143:952–960
Ferguson JJ, Califf RM, Antman EM et al (2004) Enoxaparin vs. unfractionated heparin in high-risk patients with non-ST-segment elevation in acute coronary syndromes managed with an intended early invasive strategy. JAMA 292:45–54
Braunwald E, Antman EM, Beasley JW et al (2002) ACC/AHA guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction—2002: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (committee on the Management of Patients With Unstable Angina). Circulation 106:1893–1900
Yusuf S, Zhao F, Mehta SR et al (2001) Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med 345:494–502
Alexander KP, Chen AY, Roe MT et al (2005) Excess dosing of antiplatelet and antithrombin agents in the treatment of non-ST-segment elevation acute coronary syndromes. JAMA 294:3108–3116
Cheng S, Morrow DA, Sloan S et al (2009) Predictors of initial nontherapeutic anticoagulation with unfractionated heparin in ST-segment elevation myocardial infarction. Circulation 119:1195–1202
Mahaffey KW, Goodman SG (2006) Low-molecular-weight heparin vs unfractionated heparin in acute coronary syndromes—reply. JAMA 295:2353–2354
Funding
The SYNERGY trial was sponsored by Sanofi-Aventis.
Conflict of interest
M. Thomas, K. Chiswell, and R. Becker have no disclosures to report in the development or writing of this manuscript. K. Mahaffey received research grants and consulting fees or honoraria from Sanofi-Aventis. M. Cohen received research grants from and was on the speaker’s bureau for Sanofi-Aventis. M. Kontos was on the speaker’s bureau of and received consultation fees or honoraria from Sanofi-Aventis. E. Antman received research grants from Sanofi-Aventis. J. Ferguson received research grants and consultation fees or honoraria from and was on the speaker’s bureau of Sanofi-Aventis. R. Califf received consultation fees or honoraria and research funding from Sanofi-Aventis. S. Goodman received research grants and consulting fees or honoraria from Sanofi-Aventis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thomas, M.P., Mahaffey, K.W., Chiswell, K. et al. Activated partial thromboplastin time measurement is not associated with clinical outcomes in patients with high-risk non-ST-segment elevation acute coronary syndromes treated with unfractionated heparin. J Thromb Thrombolysis 34, 114–119 (2012). https://doi.org/10.1007/s11239-012-0693-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-012-0693-y