Abstract
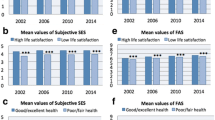
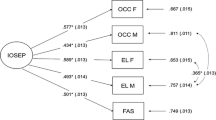
Socioeconomic differences in health are ubiquitous across age groups, cultures, and health domains. However, variation in the size and pattern of health inequalities appears to relate to the measure of socioeconomic position (SEP) applied. Little attention has been paid to these differences in adolescents and their implications for health surveillance and policy. We examined health inequalities in 1371 adolescents in seven European countries using four measures of SEP: youth-reported material assets and subjective social status and parent-reported material assets and household income. For each SEP variable, we estimated risk ratios, risk differences, concentration curves, and concentration indices of inequality for fair/poor self-rated health and low life satisfaction. Results showed that inequalities in health and life satisfaction were largest when subjective social status was used as the SEP variable. Moreover, health inequalities defined by subjective social status did not change after differences in assets and income were statistically controlled. Although material assets yielded similar health inequalities as household income, the results suggest that subjective and objective SEP relate differently to adolescent health and are not equivalent indicators of the same construct. In addition, possible bidirectional effects on health and wellbeing may inflate health inequalities defined by subjective social status. These results indicate that SEP differences in adolescent health are relate more closely to psychosocial processes than to material inequality.


Similar content being viewed by others
References
American Psychological Association Task Force on Socioeconomic Status. (2007). Report of the APA task force on socioeconomic status. Washington, DC: American Psychological Association.
Bradley, R. H., & Corwyn, R. F. (2002). Socioeconomic status and child development. Annual Review of Psychology, 53, 371–399.
Breidablik, H. J., Meland, E., & Lydersen, S. (2009). Self-rated health during adolescence: stability and predictors of change (Young-HUNT study, Norway). European Journal of Public Health, 19(1), 73–78.
Cantril, H. (1965). The pattern of human concern. New Brunswick, NJ: Rutgers University Press.
Currie, C., Inchley, J., Molcho, M., Lenzi, M., Veselska, Z., & Wild, F. (2014). Health Behaviour in School-aged Children (HBSC) study protocol: Background, methodology and mandatory items for the 2013/14 Survey. St. Andrews: Child and Adolescent Health Research Unit, St. Andrews University.
Currie, C., Molcho, M., Boyce, W., Holstein, B., Torsheim, T., & Richter, M. (2008). Researching health inequalities in adolescents: The development of the Health Behaviour in School-Aged Children (HBSC) family affluence scale. Social Science and Medicine, 66(6), 1429–1436.
Currie, C., Zanotti, C., Morgan, A., Currie, D., de Looze, M., Roberts, C., Samdal, O., Smith, O. R. F., & Barnekow, V. (2012). Social determinants of health and well-being among young people. In Health Behaviour in School-aged Children (HBSC) Study: International Report from the 2009/10 Survey (Health Policies for Children and Adolescents, No. 6. 2012). Copenhagen: World Health Organisation.
Elgar, F. J., De Clercq, B., Schnohr, C. W., Bird, P., Pickett, K. E., Torsheim, T., et al. (2013). Absolute and relative family affluence and psychosomatic symptoms in adolescents. Social Science and Medicine, 91, 25–31.
Elgar, F. J., Pförtner, T. K., Moor, I., De Clercq, B., Stevens, G. W., & Currie C. (in press). Socioeconomic inequalities in adolescent health 2002–2010: A time-series analysis of 34 countries participating in the Health Behaviour in School-aged Children study. The Lancet. doi: 10.1016/S0140-6736(14)61460-4.
Fosse, N. E., & Haas, S. A. (2009). Validity and stability of self-reported health among adolescents in a longitudinal, nationally representative survey. Pediatrics, 123(3), e496–e501.
Garbarski, D. (2010). Perceived social position and health: Is there a reciprocal relationship? Social Science and Medicine, 70(5), 692–699.
Goodman, E., Adler, N. E., Kawachi, I., Frazier, A. L., Huang, B., & Colditz, G. A. (2001). Adolescents’ perceptions of social status: Development and evaluation of a new indicator. Pediatrics, 108(2), e31.
Goodman, E., Huang, B., Schafer-Kalkhoff, T., & Adler, N. E. (2007). Perceived socioeconomic status: A new type of identity that influences adolescents’ self-rated health. Journal of Adolescent Health, 41(5), 479–487.
Hollingshead, A. A. (1975). Four-factor index of social status. Unpublished manuscript, New Haven, CT: Yale University.
Kleinman, L. C., & Norton, E. C. (2009). What’s the risk? A simple approach for estimating adjusted risk measures from nonlinear models including logistic regression. Health Services Research, 44(1), 288–302.
Lindelow, M. (2006). Sometimes more equal than others: How health inequalities depend on the choice of welfare indicator. Health Economics, 15(3), 263–279.
Quon, E. C., & McGrath, J. J. (2014). Subjective socioeconomic status and adolescent health: A meta-analysis. Health Psychology, 33(5), 433–447.
Singh, G. K., & Ghandour, R. M. (2012). Impact of neighborhood social conditions and household socioeconomic status on behavioral problems among US children. Maternal and Child Health Journal, 16(1), S158–S169.
Singh-Manoux, A., Adler, N. E., & Marmot, M. G. (2003). Subjective social status: its determinants and its association with measures of ill-health in the Whitehall II study. Social Science and Medicine, 56(6), 1321–1333.
Starfield, B., Riley, A. W., Witt, W. P., & Robertson, J. (2002). Social class gradients in health during adolescence. Journal of Epidemiology and Community Health, 56(5), 354–361.
Torsheim, T., Currie, C., Boyce, W., Kalnins, I., Overpeck, M., & Haugland, S. (2004). Material deprivation and self-rated health: A multilevel study of adolescents from 22 European and North American countries. Social Science and Medicine, 59(1), 1–12.
Viner, R. M., Ozer, E. M., Denny, S., Marmot, M., Resnick, M., Fatusi, A., & Currie, C. (2012). Adolescence and the social determinants of health. Lancet, 379(9826), 1641–1652.
Wagstaff, A., Van Doorslaer, E., & Paci, P. (1991). On the measurement of horizontal inequity in the delivery of health care. Journal of Health Economics, 10(2), 169–205.
West, P., & Sweeting, H. (2004). Evidence on equalisation in health in youth from the West of Scotland. Social Science and Medicine, 59(1), 13–27.
Williams, D. R., & Collins, C. (1995). US socioeconomic and racial differences in health: Patterns and explanations. Annual Review of Sociology, 21, 349–386.
Acknowledgments
The study was supported by grants from the Canadian Institutes for Health Research, the Social Sciences and Humanities Research Council of Canada, and the Canada Research Chairs programme. The Health Behaviour in School-aged Children study (HBSC) is a World Health Organisation (WHO) collaborative cross-national study carried out in collaboration with WHO Regional Office for Europe. The International Coordinator of the 2014 survey was Candace Currie, University of St. Andrews and the Data Bank Manager was Oddrun Samdal, University of Bergen. The data used for this research were collected by principal investigators in Greenland (Birgit Niclasen), Italy (Franco Cavallo), Norway (Oddrun Samdal), Poland (Joanna Mazur), Romania (Adriana Baban), Scotland (Candace Currie), and Slovakia (Andrea Madarasova Geckova). For details, see http://www.hbsc.org.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Elgar, F.J., McKinnon, B., Torsheim, T. et al. Patterns of Socioeconomic Inequality in Adolescent Health Differ According to the Measure of Socioeconomic Position. Soc Indic Res 127, 1169–1180 (2016). https://doi.org/10.1007/s11205-015-0994-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11205-015-0994-6