Abstract
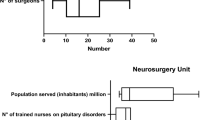
Surgical experience is of paramount importance to reach therapeutic success and minimize operative complications. In the field of pituitary surgery, this led to the concept of Pituitary Center of Excellence (PTCOE) defined as a center where an interdisciplinary team works in collaboration and where surgeons can be trained appropriately to reach and keep excellence in daily practice. To review the literature to define the optimal referral population size to establish a PTCOE to optimize both training and specific field research. A review of the literature was performed about epidemiology. The time needed to observe 200 cases of PAs in a single PTCOE and to reach the minimal surgical experience threshold (MSET) was calculated for different referral population groups. The time needed to reach MSET decreased as population size increased. We defined a population as the optimal one to be served by a single PTCOE with a single dedicated neurosurgeon. PTCOEs should be established after an analysis of the referral population, number of cases suitable for surgical treatment and number of dedicated neurosurgeons.







Similar content being viewed by others
References
Gittleman H, Ostrom QT, Farah PD, Ondracek A, Chen Y, Wolinsky Y, et al. Descriptive epidemiology of pituitary tumors in the United States, 2004-2009. J Neurosurg. 2014;121(3):527–35.
Melmed S. Pituitary-tumor endocrinopathies. N Engl J Med. 2020;382(10):937–50.
Karavitaki N. Prevalence and incidence of pituitary adenomas. Ann Endocrinol (Paris). 2012;73(2):79–80.
Raappana A, Koivukangas J, Ebeling T, Pirilä T. Incidence of pituitary adenomas in northern Finland in 1992-2007. J Clin Endocrinol Metab. 2010;95(9):4268–75.
Agustsson TT, Baldvinsdottir T, Jonasson JG, Olafsdottir E, Steinthorsdottir V, Sigurdsson G, et al. The epidemiology of pituitary adenomas in Iceland, 1955-2012: a nationwide population-based study. Eur J Endocrinol. 2015;173(5):655–64.
Day PF, Loto MG, Glerean M, Picasso MFR, Lovazzano S, Giunta DH. Incidence and prevalence of clinically relevant pituitary adenomas: retrospective cohort study in a health management organization in Buenos Aires, Argentina. Arch Endocrinol Metab. 2016;60(6):554–61.
Gruppetta M, Mercieca C, Vassallo J. Prevalence and incidence of pituitary adenomas: a population based study in Malta. Pituitary. 2013;16(4):545–53.
Tjornstrand A, et al. The incidence rate of pituitary adenomas in western Sweden for the period 2001-2011. Eur J Endocrinol. 2014;171(4):519–26.
Colao A, Grasso LFS, Giustina A, Melmed S, Chanson P, Pereira AM, et al. Acromegaly. Nat Rev Dis Primers. 2019;5(1):20.
Al-Dahmani K, et al. Sellar masses: an epidemiological study. Can J Neurol Sci. 2016;43(2):291–7.
Arnaldi G, Angeli A, Atkinson AB, Bertagna X, Cavagnini F, Chrousos GP, et al. Diagnosis and complications of Cushing's syndrome: a consensus statement. J Clin Endocrinol Metab. 2003;88(12):5593–602.
Melmed S, Colao A, Barkan A, Molitch M, Grossman AB, Kleinberg D, et al. Guidelines for acromegaly management: an update. J Clin Endocrinol Metab. 2009;94(5):1509–17.
Casanueva FF, Molitch ME, Schlechte JA, Abs R, Bonert V, Bronstein MD, et al. Guidelines of the pituitary society for the diagnosis and management of prolactinomas. Clin Endocrinol. 2006;65(2):265–73.
Petersenn S, Giustina A. Diagnosis and management of prolactinomas: current challenges. Pituitary. 2020;23(1):1–2.
Buchfelder M, Zhao Y, Schlaffer SM. Surgery for prolactinomas to date. Neuroendocrinology. 2019;109(1):77–81.
Kreutzer J, Buslei R, Wallaschofski H, Hofmann B, Nimsky C, Fahlbusch R, et al. Operative treatment of prolactinomas: indications and results in a current consecutive series of 212 patients. Eur J Endocrinol. 2008;158(1):11–8.
Babey M, Sahli R, Vajtai I, Andres RH, Seiler RW. Pituitary surgery for small prolactinomas as an alternative to treatment with dopamine agonists. Pituitary. 2011;14(3):222–30.
Buchfelder M, Schlaffer SM, Zhao Y. The optimal surgical techniques for pituitary tumors. Best Pract Res Clin Endocrinol Metab. 2019;33(2):101299.
Agam MS, et al. Complications associated with microscopic and endoscopic transsphenoidal pituitary surgery: experience of 1153 consecutive cases treated at a single tertiary care pituitary center. J Neurosurg. 2018:1–8.
Mortini P. Cons: endoscopic endonasal transsphenoidal pituitary surgery is not superior to microscopic transsphenoidal surgery for pituitary adenomas. Endocrine. 2014;47(2):415–20.
Asemota AO, Ishii M, Brem H, Gallia GL. Comparison of complications, trends, and costs in endoscopic vs microscopic pituitary surgery: analysis from a US health claims database. Neurosurgery. 2017;81(3):458–72.
Rolston JD, Han SJ, Aghi MK. Nationwide shift from microscopic to endoscopic transsphenoidal pituitary surgery. Pituitary. 2016;19(3):248–50.
Greenblatt SH. Harvey Cushing’s paradigmatic contribution to neurosurgery and the evolution of his thoughts about specialization. Bull Hist Med. 2003;77(4):789–822.
Barker FG II, Klibanski A, Swearingen B. Transsphenoidal surgery for pituitary tumors in the United States, 1996-2000: mortality, morbidity, and the effects of hospital and surgeon volume. J Clin Endocrinol Metab. 2003;88(10):4709–19.
Gittoes NS, Sheppard MC, Johnson AP, Stewart PM. Outcome of surgery for acromegaly--the experience of a dedicated pituitary surgeon. QJM. 1999;92:741–5.
Wang YY, Higham C, Kearney T, Davis JRE, Trainer P, Gnanalingham KK. Acromegaly surgery in Manchester revisited--the impact of reducing surgeon numbers and the 2010 consensus guidelines for disease remission. Clin Endocrinol. 2012;76(3):399–406.
Ahmed S, Elsheikh M, Stratton IM, Page RC, Adams CB, Wass JA. Outcome of transphenoidal surgery for acromegaly and its relationship to surgical experience. Clin Endocrinol. 1999;50(5):561–7.
Honegger J, Grimm F. The experience with transsphenoidal surgery and its importance to outcomes. Pituitary. 2018;21(5):545–55.
Jane JA Jr, Sulton LD, Laws ER Jr. Surgery for primary brain tumors at United States academic training centers: results from the residency review committee for neurological surgery. J Neurosurg. 2005;103(5):789–93.
Ramsay CR, Grant AM, Wallace SA, Garthwaite PH, Monk AF, Russell IT. Statistical assessment of the learning curves of health technologies. Health Technol Assess. 2001;5(12):1–79.
Papachristofi O, Jenkins D, Sharples LD. Assessment of learning curves in complex surgical interventions: a consecutive case-series study. Trials. 2016;17(1):266.
Cook JA, Ramsay CR, Fayers P. Statistical evaluation of learning curve effects in surgical trials. Clin Trials. 2004;1(5):421–7.
Ciric IR, Ragin A, Baumgartner C, Pierce D. Complications of transsphenoidal surgery: results of a national survey, review of the literature, and personal experience. Neurosurgery. 1997;40:225–37.
Mortini P, Barzaghi LR, Albano L, Panni P, Losa M. Microsurgical therapy of pituitary adenomas. Endocrine. 2018;59(1):72–81.
Clayton RN, Stewart PM, Shalet SM, Wass JAH. Pituitary surgery for acromegaly. Should be done by specialists. BMJ. 1999;319(7210):588–9.
Giustina A, et al. A consensus on the diagnosis and treatment of acromegaly comorbidities: an update. J Clin Endocrinol Metab. 2020:105(4).
Giustina A, Bronstein MD, Casanueva FF, Chanson P, Ghigo E, Ho KKY, et al. Current management practices for acromegaly: an international survey. Pituitary. 2011;14(2):125–33.
Giustina A, Bronstein MD, Chanson P, Petersenn S, Casanueva FF, Sert C, et al. Staging and managing patients with acromegaly in clinical practice: baseline data from the SAGIT(R) validation study. Pituitary. 2019;22(5):476–87.
Fusco A, Zatelli MC, Bianchi A, Cimino V, Tilaro L, Veltri F, et al. Prognostic significance of the Ki-67 labeling index in growth hormone-secreting pituitary adenomas. J Clin Endocrinol Metab. 2008;93(7):2746–50.
Mancini T, Doga M, Mazziotti G, Giustina A. Cushing’s syndrome and bone. Pituitary. 2004;7(4):249–52.
Mancini T, Porcelli T, Giustina A. Treatment of Cushing disease: overview and recent findings. Ther Clin Risk Manag. 2010;6:505–16.
Ho KKY, Fleseriu M, Wass J, van der Lely A, Barkan A, Giustina A, et al. A tale of pituitary adenomas: to NET or not to NET : pituitary society position statement. Pituitary. 2019;22(6):569–73.
Casanueva FF, et al. Criteria for the definition of pituitary tumor centers of excellence (PTCOE): a pituitary society statement. Pituitary. 2017;20(5):489–98.
Cushing H. Intracranial tumors: notes upon a series of two thousand verified cases with surgical-mortality percentages pertaining thereto. JAMA. 1932.
Rees DA, Hanna FWF, Davies JS, Mills RG, Vafidis J, Scanlon MF. Long-term follow-up results of transsphenoidal surgery for Cushing’s disease in a single centre using strict criteria for remission. Clin Endocrinol. 2002;56(4):541–51.
Trinh VT, Davies JM, Berger MS. Surgery for primary supratentorial brain tumors in the United States, 2000-2009: effect of provider and hospital caseload on complication rates. J Neurosurg. 2015;122(2):280–96.
Birkmeyer JD, Siewers AE, Finlayson EVA, Stukel TA, Lucas FL, Batista I, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346(15):1128–37.
Hillner BE, Smith TJ, Desch CE. Hospital and physician volume or specialization and outcomes in cancer treatment: importance in quality of cancer care. J Clin Oncol. 2000;18(11):2327–40.
Weisman CS, Squires GL. Women's health centers: are the National Centers of excellence in women’s health a new model? Womens Health Issues. 2000;10(5):248–55.
Champion JK, Pories WJ. Centers of excellence for bariatric surgery. Surg Obes Relat Dis. 2005;1(2):148–51.
Pratt GM, McLees B, Pories WJ. The ASBS bariatric surgery centers of excellence program: a blueprint for quality improvement. Surg Obes Relat Dis. 2006;2(5):497–503 discussion 503.
Begg CB, Cramer LD, Hoskins WJ, Brennan MF. Impact of hospital volume on operative mortality for major cancer surgery. JAMA. 1998;280(20):1747–51.
Cushing H. The special field of neurological surgery: five years later. Bull Johns Hopkins Hosp. 1910;65:327.
Giustina A, Chanson P, Bronstein MD, Klibanski A, Lamberts S, Casanueva FF, et al. A consensus on criteria for cure of acromegaly. J Clin Endocrinol Metab. 2010;95(7):3141–8.
Erturk E, Tuncel E, Kiyici S, Ersoy C, Duran C, Imamoglu S. Outcome of surgery for acromegaly performed by different surgeons: importance of surgical experience. Pituitary. 2005;8(2):93–7.
Bates PR, Carson MN, Trainer PJ, Wass JAH, the UK National Acromegaly Register Study Group (UKAR-2). Wide variation in surgical outcomes for acromegaly in the UK. Clin Endocrinol. 2008;68(1):136–42.
Lissett CA, Peacey SR, Laing I, Tetlow L, Davis JR, Shalet SM. The outcome of surgery for acromegaly: the need for a specialist pituitary surgeon for all types of growth hormone (GH) secreting adenoma. Clin Endocrinol. 1998;49(5):653–7.
Katznelson L, Bogan JS, Trob JR, Schoenfeld DA, Hedley-Whyte ET, Hsu DW, et al. Biochemical assessment of Cushing’s disease in patients with corticotroph macroadenomas. J Clin Endocrinol Metab. 1998;83(5):1619–23.
Perry A, Graffeo CS, Meyer J, Carlstrom LP, Oushy S, Driscoll CLW, et al. Beyond the learning curve: comparison of microscopic and endoscopic incidences of internal carotid injury in a series of highly experienced operators. World Neurosurg. 2019;131:e128–35.
Clayton RN. How many surgeons to operate on acromegalic patients?*. Clin Endocrinol. 1999;50:557–9.
Wass JA, Turner HE, Adams CB. The importance of locating a good pituitary surgeon. Pituitary. 1999;2(1):51–4.
McLaughlin N, Laws ER, Oyesiku NM, Katznelson L, Kelly DF. Pituitary centers of excellence. Neurosurgery. 2012;71(5):916–24 discussion 924-6.
Giustina A. Acromegaly and vertebral fractures: facts and questions. Trends Endocrinol Metab. 2020;31(4):274–5.
Mazziotti G, Frara S, Giustina A. Pituitary diseases and bone. Endocr Rev. 2018;39(4):440–88.
Shahlaie K, McLaughlin N, Kassam AB, Kelly DF. The role of outcomes data for assessing the expertise of a pituitary surgeon. Curr Opin Endocrinol Diabetes Obes. 2010;17(4):369–76.
Giustina A, Mazziotti G, Torri V, Spinello M, Floriani I, Melmed S. Meta-analysis on the effects of octreotide on tumor mass in acromegaly. PLoS One. 2012;7(5):e36411.
Mancini T, Casanueva FF, Giustina A. Hyperprolactinemia and prolactinomas. Endocrinol Metab Clin N Am. 2008;37(1):67–99 viii.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mortini, P., Nocera, G., Roncelli, F. et al. The optimal numerosity of the referral population of pituitary tumors centers of excellence (PTCOE): A surgical perspective. Rev Endocr Metab Disord 21, 527–536 (2020). https://doi.org/10.1007/s11154-020-09564-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11154-020-09564-7