Abstract
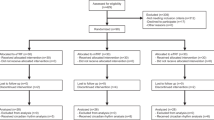
Restriction in meal timing has emerged as a promising dietary approach for the management of obesity and dysmetabolic diseases. The present systematic review and meta-analysis summarized the most recent evidence on the effect of time-restricted feeding (TRF) on weight-loss and cardiometabolic variables in comparison with unrestricted-time regimens. Studies involving TRF regimen were systematically searched up to January 2019. Effect size was expressed as weighted mean difference (WMD) and 95% confidence intervals (CI). A total of 11 studies, 5 randomized controlled trials and 6 observational, were included. All selected studies had a control group without time restriction; hours of fasting ranged from 12-h until 20-h and study duration from 4 to 8-weeks. Most studies involved the Ramadan fasting. TRF determined a greater weight-loss than control regimens (11 studies, n = 485 subjects) (WMD: −1.07 kg, 95%CI: −1.74 to −0.40; p = 0.002; I2 = 56.2%), unrelated to study design. The subgroup analysis showed an inverse association between TRF and fat free mass in observational studies (WMD: −1.33 kg, 95%CI: −2.55 to −0.11; p = 0.03; I2 = 0%). An overall significant reduction in fasting glucose concentrations was observed with TRF regimens (7 studies, n = 363 subjects) (WMD: −1.71 mg/dL, 95%CI: −3.20 to −0.21; p = 0.03; I2 = 0%), above all in trials (WMD:-2.45 mg/dL, 95%CI: −4.72 to −0.17; p = 0.03; I2 = 0%). No between-group differences in the other variables were found. TRF regimens achieved a superior effect in promoting weight-loss and reducing fasting glucose compared to approaches with unrestricted time in meal consumption. However, long-term and well-designed trials are needed to draw definitive conclusions.








Similar content being viewed by others
Change history
18 February 2020
The article “Effects of time-restricted feeding on body weight and metabolism. A systematic review and meta-analysis” written by Pellegrini Marianna, Cioffi Iolanda, Evangelista Andrea, Ponzo Valentina, Goitre Ilaria, Ciccone Giovannino, Ghigo Ezio, Bo Simona” was originally published with the surname and then first name of all authors.
References
WHO. Overweight and obesity [Internet]. WHO. [citato 24 giugno 2019]. Available at: http://www.who.int/gho/ncd/risk_factors/overweight/en/
Chooi YC, Ding C, Magkos F. The epidemiology of obesity. Metab Clin Exp. 2019;92:6–10.
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627–42.
Tobias DK, Hu FB. The association between BMI and mortality: implications for obesity prevention. The Lancet Diabetes & Endocrinology. 2018;6(12):916–7.
Jaacks LM, Vandevijvere S, Pan A, McGowan CJ, Wallace C, Imamura F, et al. The obesity transition: stages of the global epidemic. Lancet Diabetes Endocrinol. 2019;7(3):231–40.
Yannakoulia M, Poulimeneas D, Mamalaki E, Anastasiou CA. Dietary modifications for weight loss and weight loss maintenance. Metab Clin Exp. 2019;92:153–62.
Leech RM, Timperio A, Livingstone KM, Worsley A, McNaughton SA. Temporal eating patterns: associations with nutrient intakes, diet quality, and measures of adiposity. Am J Clin Nutr. 2017;106(4):1121–30.
Rothschild J, Hoddy KK, Jambazian P, Varady KA. Time-restricted feeding and risk of metabolic disease: a review of human and animal studies. Nutr Rev. 2014;72(5):308–18.
Chaix A, Zarrinpar A, Miu P, Panda S. Time-restricted feeding is a preventative and therapeutic intervention against diverse nutritional challenges. Cell Metab. 2014;20(6):991–1005.
Lessan N, Ali T. Energy Metabolism and Intermittent Fasting: The Ramadan Perspective. Nutrients. 2019;11(5):1192.
Abolaban H, Al-Moujahed A. Muslim patients in Ramadan: a review for primary care physicians. Avicenna J Med. 2017;7(3):81–7.
Trepanowski JF, Bloomer RJ. The impact of religious fasting on human health. Nutr J. 2010;9:57.
Fernando HA, Zibellini J, Harris RA, Seimon RV, Sainsbury A. Effect of Ramadan fasting on weight and body composition in healthy non-athlete adults: a systematic review and meta-analysis. Nutrients. 2019;11:478.
Mazidi M, Rezaie P, Chaudhri O, Karimi E, Nematy M. The effect of Ramadan fasting on cardiometabolic risk factors and anthropometrics parameters: a systematic review. Pak J Med Sci. 2015;31(5):1250–5.
Al-Barha NS, Aljaloud KS. The effect of Ramadan fasting on body composition and metabolic syndrome in apparently healthy men. Am J Mens Health. 2019;13(1):1557988318816925.
Ongsara S, Boonpol S, Prompalad N, Jeenduang N. The effect of Ramadan fasting on biochemical parameters in healthy Thai subjects. J Clin Diagn Res. 2017;11(9):BC14–8.
Sadeghirad B, Motaghipisheh S, Kolahdooz F, Zahedi MJ, Haghdoost AA. Islamic fasting and weight loss: a systematic review and meta-analysis. Public Health Nutr. 2014;17(2):396–406.
Kul S, Savaş E, Öztürk ZA, Karadağ G. Does Ramadan fasting alter body weight and blood lipids and fasting blood glucose in a healthy population? A meta-analysis J Relig Health. 2014;53(3):929–42.
Koufakis T, Karras SΝ, Antonopoulou V, Angeloudi E, Zebekakis P, Kotsa K. Effects of orthodox religious fasting on human health: a systematic review. Eur J Nutr. 2017;56(8):2439–55.
Persynaki A, Karras S, Pichard C. Unraveling the metabolic health benefits of fasting related to religious beliefs: a narrative review. Nutrition. 2017;35:14–20.
LeCheminant JD, Christenson E, Bailey BW, Tucker LA. Restricting night-time eating reduces daily energy intake in healthy young men: a short-term cross-over study. Br J Nutr. 2013;110(11):2108–13.
Carlson O, Martin B, Stote KS, Golden E, Maudsley S, Najjar SS, et al. Impact of reduced meal frequency without caloric restriction on glucose regulation in healthy, normal-weight middle-aged men and women. Metab Clin Exp. 2007;56(12):1729–34.
Fond G, Macgregor A, Leboyer M, Michalsen A. Fasting in mood disorders: neurobiology and effectiveness. A review of the literature. Psychiatry Res. 2013;209(3):253–8.
Beccuti G, Monagheddu C, Evangelista A, Ciccone G, Broglio F, Soldati L, et al. Timing of food intake: Sounding the alarm about metabolic impairments? A systematic review. Pharmacol Res. 2017;125(Pt B):132–41.
Jiang P, Turek FW. Timing of meals: when is as critical as what and how much. Am J Physiol Endocrinol Metab. 2017;312(5):E369–80.
Saini C, Suter DM, Liani A, Gos P, Schibler U. The mammalian circadian timing system: synchronization of peripheral clocks. Cold Spring Harb Symp Quant Biol. 2011;76:39–47.
Longo VD, Panda S. Fasting, circadian rhythms, and time restricted feeding in healthy lifespan. Cell Metab. 2016;23(6):1048–59.
Ekmekcioglu C, Touitou Y. Chronobiological aspects of food intake and metabolism and their relevance on energy balance and weight regulation. Obes Rev. 2011;12(1):14–25.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
Cochrane Handbook for Systematic Reviews of Interventions [Internet]. [citato 11 luglio 2019]. Available at: http://handbook-5-1.cochrane.org.bibliopass.unito.it/
Harder-Lauridsen NM, Rosenberg A, Benatti FB, Damm JA, Thomsen C, Mortensen EL, et al. Ramadan model of intermittent fasting for 28 d had no major effect on body composition, glucose metabolism, or cognitive functions in healthy lean men. Nutrition. 2017;37:92–103.
Betts JA, Richardson JD, Chowdhury EA, Holman GD, Tsintzas K, Thompson D. The causal role of breakfast in energy balance and health: a randomized controlled trial in lean adults. Am J Clin Nutr. 2014;100(2):539–47.
Moro T, Tinsley G, Bianco A, Marcolin G, Pacelli QF, Battaglia G, et al. Effects of eight weeks of time-restricted feeding (16/8) on basal metabolism, maximal strength, body composition, inflammation, and cardiovascular risk factors in resistance-trained males. J Transl Med. 2016;14(1):290.
Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Afrasiabi A, Hassanzadeh S, Sattarivand R, Nouri M, Mahbood S. Effects of low fat and low calorie diet on plasma lipid levels in the fasting month of Ramadan. Saudi Med J. 2003;24(2):184–8.
Alsubheen SA, Ismail M, Baker A, Blair J, Adebayo A, Kelly L, et al. The effects of diurnal Ramadan fasting on energy expenditure and substrate oxidation in healthy men. Br J Nutr. 2017;118(12):1023–30.
Aliasghari F, Izadi A, Gargari BP, Ebrahimi S. The effects of Ramadan fasting on body composition, blood pressure, glucose metabolism, and markers of inflammation in NAFLD patients: an observational trial. J Am Coll Nutr. 2017;36(8):640–5.
Nugraha B, Ghashang SK, Hamdan I, Gutenbrunner C. Effect of Ramadan fasting on fatigue, mood, sleepiness, and health-related quality of life of healthy young men in summer time in Germany: A prospective controlled study. Appetite. 2017;111:38–45.
Karatoprak C, Yolbas S, Cakirca M, Cinar A, Zorlu M, Kiskac M, et al. The effects of long term fasting in Ramadan on glucose regulation in type 2 diabetes mellitus. Eur Rev Med Pharmacol Sci. 2013;17(18):2512–6.
Stote KS, Baer DJ, Spears K, Paul DR, Harris GK, Rumpler WV, et al. A controlled trial of reduced meal frequency without caloric restriction in healthy, normal-weight, middle-aged adults. Am J Clin Nutr. 2007;85(4):981–8.
Sutton EF, Beyl R, Early KS, Cefalu WT, Ravussin E, Peterson CM. Early Time-Restricted Feeding Improves Insulin Sensitivity, Blood Pressure, and Oxidative Stress Even without Weight Loss in Men with Prediabetes. Cell Metab. 2018;27(6):1212–1221.e3.
Tinsley GM, Forsse JS, Butler NK, Paoli A, Bane AA, La Bounty PM, et al. Time-restricted feeding in young men performing resistance training: a randomized controlled trial. Eur J Sport Sci. 2017;17(2):200–7.
Hatori M, Vollmers C, Zarrinpar A, DiTacchio L, Bushong EA, Gill S, et al. Time-restricted feeding without reducing caloric intake prevents metabolic diseases in mice fed a high-fat diet. Cell Metab. 2012;15(6):848–60.
Olsen MK, Choi MH, Kulseng B, Zhao C-M, Chen D. Time-restricted feeding on weekdays restricts weight gain: A study using rat models of high-fat diet-induced obesity. Physiol Behav. 2017;173:298–304.
Chaix A, Lin T, Le HD, Chang MW, Panda S. Time-Restricted Feeding Prevents Obesity and Metabolic Syndrome in Mice Lacking a Circadian Clock. Cell Metab. 2019;29(2):303–319.e4.
Melkonian EA, Schury MP. Physiology, Gluconeogenesis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 [citato 29 giugno 2019]. Available at: http://www.ncbi.nlm.nih.gov/books/NBK541119/
Anton SD, Moehl K, Donahoo WT, Marosi K, Lee SA, Mainous AG, et al. Flipping the metabolic switch: understanding and applying the health benefits of fasting. Obesity (Silver Spring). 2018;26(2):254–68.
Zarrinpar A, Chaix A, Yooseph S, Panda S. Diet and feeding pattern affect the diurnal dynamics of the gut microbiome. Cell Metab. 2014;20(6):1006–17.
Ren J, Hu D, Mao Y, Yang H, Liao W, Xu W, et al. Alteration in gut microbiota caused by time-restricted feeding alleviate hepatic ischaemia reperfusion injury in mice. J Cell Mol Med. 2019;23(3):1714–22.
van der Merwe M, Sharma S, Caldwell J, Smith N, Bloomer R, Buddington R, et al. Diet Modification and Not Timed Feeding Strategies Result in Intestinal Microbiome Alterations (P21–030-19). Curr Dev Nutr. 2019;3(Suppl 1).
Leone V, Gibbons SM, Martinez K, Hutchison AL, Huang EY, Cham CM, et al. Effects of diurnal variation of gut microbes and high-fat feeding on host circadian clock function and metabolism. Cell Host Microbe. 2015;17(5):681–9.
Depner CM, Stothard ER, Wright KP. Metabolic consequences of sleep and circadian disorders. Curr Diab Rep. 2014;14(7):507.
Parkar SG, Kalsbeek A, Cheeseman JF. Potential Role for the Gut Microbiota in Modulating Host Circadian Rhythms and Metabolic Health. Microorganisms. 2019;7(2):41.
Salim I, Al Suwaidi J, Ghadban W, Alkilani H, Salam AM. Impact of religious Ramadan fasting on cardiovascular disease: a systematic review of the literature. Curr Med Res Opin. 2013;29(4):343–54.
Santos HO, Macedo RCO. Impact of intermittent fasting on the lipid profile: assessment associated with diet and weight loss. Clin Nutr ESPEN. 2018;24:14–21.
Turin TC, Ahmed S, Shommu NS, Afzal AR, Al Mamun M, Qasqas M, et al. Ramadan fasting is not usually associated with the risk of cardiovascular events: a systematic review and meta-analysis. J Family Community Med. 2016;23(2):73–81.
Patterson RE, Sears DD. Metabolic Effects of Intermittent Fasting. Annu Rev Nutr. 2017;37:371–93.
Hutchison AT, Heilbronn LK. Metabolic impacts of altering meal frequency and timing - does when we eat matter? Biochimie. 2016;124:187–97.
Patterson RE, Laughlin GA, LaCroix AZ, Hartman SJ, Natarajan L, Senger CM, et al. Intermittent fasting and human metabolic health. J Acad Nutr Diet. 2015;115(8):1203–12.
Jamshed H, Beyl RA, Della Manna DL, Yang ES, Ravussin E, Peterson CM. Early Time-Restricted Feeding Improves 24-Hour Glucose Levels and Affects Markers of the Circadian Clock, Aging, and Autophagy in Humans. Nutrients. 2019;11(6)1234.
Scheer FAJL, Hilton MF, Mantzoros CS, Shea SA. Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci U S A. 2009;106(11):4453–8.
Wefers J, van Moorsel D, Hansen J, Connell NJ, Havekes B, Hoeks J, et al. Circadian misalignment induces fatty acid metabolism gene profiles and compromises insulin sensitivity in human skeletal muscle. Proc Natl Acad Sci USA. 2018;115(30):7789–94.
Bo S, Musso G, Beccuti G, Fadda M, Fedele D, Gambino R, et al. Consuming more of daily caloric intake at dinner predisposes to obesity. A 6-year population-based prospective cohort study. PLoS ONE. 2014;9(9):e108467.
Bo S, Fadda M, Castiglione A, Ciccone G, De Francesco A, Fedele D, et al. Is the timing of caloric intake associated with variation in diet-induced thermogenesis and in the metabolic pattern? A randomized cross-over study. Int J Obes. 2015;39(12):1689–95.
Bo S, Broglio F, Settanni F, Parasiliti Caprino M, Ianniello A, Mengozzi G, et al. Effects of meal timing on changes in circulating epinephrine, norepinephrine, and acylated ghrelin concentrations: a pilot study. Nutr Diabetes. 2017;7(12):303.
Archer SN, Laing EE, Möller-Levet CS, van der Veen DR, Bucca G, Lazar AS, et al. Mistimed sleep disrupts circadian regulation of the human transcriptome. Proc Natl Acad Sci U S A. 2014;111(6):E682–91.
Buijs RM, Scheer FA, Kreier F, Yi C, Bos N, Goncharuk VD, et al. Organization of circadian functions: interaction with the body. Prog Brain Res. 2006;153:341–60.
Kohsaka A, Bass J. A sense of time: how molecular clocks organize metabolism. Trends Endocrinol Metab. 2007;18(1):4–11.
Thaiss CA, Zeevi D, Levy M, Zilberman-Schapira G, Suez J, Tengeler AC, et al. Transkingdom control of microbiota diurnal oscillations promotes metabolic homeostasis. Cell. 2014;159(3):514–29.
Acknowledgments
This research was funded by a grant from the Ministry of Education, University and Research of Italy (ex-60% 2017).
Author information
Authors and Affiliations
Contributions
MP participated in the conception of the paper, collection and analysis of the studies, manuscript writing and revision. IC, VP, IG, EG participated in the collection of the references and interpretation, manuscript writing and revision. AE, GC participated in the statistical analyses and interpretation of the results. SB participated in conception of the paper, collection and analysis of the studies, manuscript writing and revision. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: The article “Effects of time-restricted feeding on body weight and metabolism. A systematic review and meta-analysis” written by Pellegrini Marianna, Cioffi Iolanda, Evangelista Andrea, Ponzo Valentina, Goitre Ilaria, Ciccone Giovannino, Ghigo Ezio, Bo Simona” was originally published with the surname and then first name of all authors.
Electronic supplementary material
ESM 1
(DOCX 19 kb)
Rights and permissions
About this article
Cite this article
Pellegrini, M., Cioffi, I., Evangelista, A. et al. Effects of time-restricted feeding on body weight and metabolism. A systematic review and meta-analysis. Rev Endocr Metab Disord 21, 17–33 (2020). https://doi.org/10.1007/s11154-019-09524-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11154-019-09524-w