Abstract
Purpose
Depression is a debilitating disease with residual symptoms that negatively impact patients’ quality of life (QoL). Stigma is associated with poor QoL; however, knowledge regarding stigma subtypes and each QoL domain concerning residual depression is limited. We aimed to investigate the association of residual depression symptoms with QoL and stigma among patients with major depressive disorder (MDD).
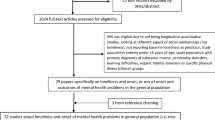
Methods
This cross-sectional study was conducted at an outpatient clinic among patients with MDD (March–July 2022). We administered the Thai version of the Patient Health Questionnaire-9, World Health Organization Quality of Life Brief, and Mental Health Consumers’ Experience of Stigma to assess patients’ levels of depression, QoL, and personal and perceived stigma, respectively. We performed correlational and logistic regression analyses to evaluate the association of demographics, QoL, stigma, and stress with residual depression.
Results
Of 384 patients with MDD (median age = 39.5, females = 73.2%), 54.4% had residual depression. Among those with residual depression, depression was negatively correlated with QoL (ρ = – 0.58, p < 0.001) and positively correlated with stigma (ρ = 0.24, p < 0.001). The risk of residual depression decreased as the QoL score increased (adjusted OR per 1-point increase 0.93 [0.91, 0.96], p < 0.001); residual depression was significantly associated with personal stigma.
Conclusion
Stigma and QoL exhibit an inverse relationship. Physical-, psychological-, and environmental-health domains of QoL and personal stigma are key contributing factors to residual MDD symptoms. Improvement of QoL and stigma requires further theoretical research and should be of concern in clinical practice. Longitudinal studies on relatively diverse populations and subsyndromal symptoms are needed.
Similar content being viewed by others
Data availability
The qualitative data used and analyzed during this study cannot be made publicly available for confidentiality reasons but can be made available, on request, from the corresponding author.
References
Ferrari, A. J., Somerville, A. J., Baxter, A. J., Norman, R., Patten, S. B., Vos, T., & Whiteford, H. A. (2013). Global variation in the prevalence and incidence of major depressive disorder: A systematic review of the epidemiological literature. Psychological Medicine, 43(3), 471–481.
Santomauro, D. F., Mantilla Herrera, A. M., Shadid, J., Zheng, P., Ashbaugh, C., Pigott, D. M., Abbafati, C., Adolph, C., Amlag, J. O., Aravkin, A. Y., Bang-Jensen, B. L., Bertolacci, G. J., Bloom, S. S., Castellano, R., Castro, E., Chakrabarti, S., Chattopadhyay, J., Cogen, R. M., Collins, J. K., & Ferrari, A. J. (2021). Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet, 398(10312), 1700–1712.
Lim, G. Y., Tam, W. W., Lu, Y., Ho, C. S., Zhang, M. W., & Ho, R. C. (2018). Prevalence of depression in the community from 30 countries between 1994 and 2014. Scientific Reports, 8(1), 2861.
Thongtang, O., Sukhatunga, K., Ngamthipwatthana, T., Chulakadabba, S., Vuthiganond, S., Pooviboonsuk, P., Kooptiwoot, S., & Phattharayuttawat, S. (2002). Prevalence and incidence of depression in the Thai elderly. Journal of the Medical Association of Thailand Chotmaihet Thangphaet, 85(5), 540–544.
Chomchoei, C., Apidechkul, T., Keawdounglek, V., Wongfu, C., Khunthason, S., Kullawong, N., Tamornpark, R., Upala, P., & Yeemard, F. (2020). Prevalence of and factors associated with depression among hill tribe individuals aged 30 years and over in Thailand. Heliyon, 6(6), e04273.
Gautam, S., Jain, A., Gautam, M., Vahia, V. N., & Grover, S. (2017). Clinical practice guidelines for the management of depression. Indian Journal of Psychiatry, 59(Suppl 1), S34–S50.
Kennedy, S. H., Lam, R. W., McIntyre, R. S., Tourjman, S. V., Bhat, V., Blier, P., Hasnain, M., Jollant, F., Levitt, A. J., MacQueen, G. M., McInerney, S. J., McIntosh, D., Milev, R. V., Müller, D. J., Parikh, S. V., Pearson, N. L., Ravindran, A. V., & Uher, R. (2016). Canadian network for mood and anxiety treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: Section 3. Pharmacological treatments. Canadian Journal of Psychiatry, 61(9), 540–560.
Al-Harbi, K. S. (2012). Treatment-resistant depression: Therapeutic trends, challenges, and future directions. Patient Preference and Adherence, 6, 369–388.
Balestri, M., Calati, R., Souery, D., Kautzky, A., Kasper, S., Montgomery, S., Zohar, J., Mendlewicz, J., & Serretti, A. (2016). Socio-demographic and clinical predictors of treatment resistant depression: A prospective European multicenter study. Journal of Affective Disorders, 189, 224–232.
Pitanupong, J., Sathaporn, K., & Tepsuan, L. (2022). Residual symptoms and their associated factors among Thai patients with depression: A multihospital-based survey. Annals of General Psychiatry, 21(1), 50.
Romera, I., Pérez, V., Ciudad, A., Caballero, L., Roca, M., Polavieja, P., & Gilaberte, I. (2013). Residual symptoms and functioning in depression, does the type of residual symptom matter? A post-hoc analysis. BMC Psychiatry, 13, 51.
Wang, Y., Wang, G., Zhang, N., Huang, J., Wu, W., Jia, F., Liu, T., Gao, C., Hu, J., Hong, W., & Fang, Y. (2020). Association between residual symptoms and social functioning in patients with depression. Comprehensive Psychiatry, 98, 152164.
Whooley, M. A., Kiefe, C. I., Chesney, M. A., Markovitz, J. H., Matthews, K., & Hulley, S. B. (2002). Depressive symptoms, unemployment, and loss of income: The CARDIA Study. Archives of Internal Medicine, 162(22), 2614–2620.
Hengartner, M. P., & Plöderl, M. (2018). Statistically significant antidepressant-placebo differences on subjective symptom-rating scales do not prove that the drugs work: Effect size and method bias matter! Frontiers in Psychiatry, 9, 517.
Link, B. G., & Phelan, J. C. (2001). Conceptualizing stigma. Annual Review of Sociology, 27, 363–385.
Steger, M. F., & Kashdan, T. B. (2009). Depression and everyday social activity, belonging, and well-being. Journal of Counseling Psychology, 56(2), 289–300.
Kupferberg, A., Bicks, L., & Hasler, G. (2016). Social functioning in major depressive disorder. Neuroscience & Biobehavioral Reviews, 69, 313–332.
Barney, L. J., Griffiths, K. M., Jorm, A. F., & Christensen, H. (2006). Stigma about depression and its impact on help-seeking intentions. Australian and New Zealand Journal of Psychiatry, 40(1), 51–54.
Griffiths, K. M., Christensen, H., & Jorm, A. F. (2008). Predictors of depression stigma. BMC Psychiatry, 8, 25.
Holubova, M., Prasko, J., Ociskova, M., Marackova, M., Grambal, A., & Slepecky, M. (2016). Self-stigma and quality of life in patients with depressive disorder: A cross-sectional study. Neuropsychiatric Disease and Treatment, 12, 2677–2687.
Sun, Y., Chen, G., Wang, L., Li, N., Srisurapanont, M., Hong, J. P., Hatim, A., Chen, C. H., Udomratn, P., Bae, J. N., Fang, Y. R., Chua, H. C., Liu, S. I., George, T., Bautista, D., Chan, E., Rush, A. J., Yang, H., Su, Y. A., & Si, T. M. (2019). Perception of stigma and its associated factors among patients with major depressive disorder: A multicenter survey from an Asian population. Frontiers in Psychiatry, 10, 321.
Lotrakul, M., Sumrithe, S., & Saipanish, R. (2008). Reliability and validity of the Thai version of the PHQ-9. BMC Psychiatry, 8, 46.
Wahl, O. F. (1999). Mental health consumers’ experience of stigma. Schizophrenia Bulletin, 25(3), 467–478.
Wannachat, O. (2016). Life skills as perceived by caregivers, social support and perceived stigma among persons with schizophrenia. Chiangmai University.
World Health Organization. Division of Mental, H. (1996). WHOQOL-BREF: Introduction, administration, scoring and generic version of the assessment: Field trial version, December 1996. World Health Organization.
Ministry of Public Health. (1997). WHOQOL-BREF-THAI. Retrieved 3 December, 2022, from http://www.dmh.go.th/test/whoqol/
Lovibond, P. F., & Lovibond, S. H. (1995). The structure of negative emotional states: Comparison of the depression anxiety stress scales (DASS) with the beck depression and anxiety inventories. Behaviour Research and Therapy, 33(3), 335–343.
Oei, T. P., Sawang, S., Goh, Y. W., & Mukhtar, F. (2013). Using the depression anxiety stress scale 21 (DASS-21) across cultures. International Journal of Psychology, 48(6), 1018–1029.
Yang, L., Zhao, Y., Wang, Y., Liu, L., Zhang, X., Li, B., & Cui, R. (2015). The effects of psychological stress on depression. Current Neuropharmacology, 13(4), 494–504.
Ravindran, A. V., Matheson, K., Griffiths, J., Merali, Z., & Anisman, H. (2002). Stress, coping, uplifts, and quality of life in subtypes of depression: A conceptual frame and emerging data. Journal of Affective Disorders, 71(1–3), 121–130.
Bostwick, J. M., & Pankratz, V. S. (2000). Affective disorders and suicide risk: A reexamination. American Journal of Psychiatry, 157(12), 1925–1932.
Hiranyatheb, T., Nakawiro, D., Wongpakaran, T., Wongpakaran, N., Bookkamana, P., Pinyopornpanish, M., Saisavoey, N., Wannarit, K., Satthapisit, S., & Tanchakvaranont, S. (2016). The impact of residual symptoms on relapse and quality of life among Thai depressive patients. Neuropsychiatric Disease and Treatment, 12, 3175–3181.
Mackenzie, C. S., Heath, P. J., Vogel, D. L., & Chekay, R. (2019). Age differences in public stigma, self-stigma, and attitudes toward seeking help: A moderated mediation model. Journal of Clinical Psychology, 75(12), 2259–2272.
Hansson, L. (2002). Quality of life in depression and anxiety. International Review of Psychiatry, 14(3), 185–189.
El-Badri, S., & Mellsop, G. (2007). Stigma and quality of life as experienced by people with mental illness. Australasian Psychiatry, 15(3), 195–200.
Oliveira, S. E., Carvalho, H., & Esteves, F. (2016). Internalized stigma and quality of life domains among people with mental illness: The mediating role of self-esteem. Journal of Mental Health, 25(1), 55–61.
Acknowledgements
The authors acknowledge the participants for their willingness to offer information; the psychiatric clinic’s nursing staff for providing space at the clinic as well as facilitating several operational aspects of the study; and the team’s research assistants, Nisan Werachattawan and Kreuwan Jongborwanwiwat, for their support. This article was proofread and edited by the International Affairs Department of the Faculty of Medicine, Prince of Songkla University.
Funding
This work was supported by the Faculty of Medicine, Prince of Songkla University, Thailand. However, the funders played no role in the study’s design, data collection, analysis, decision to publish, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
JP: Conceptualization, Methodology, Investigation, Writing—Original Draft, Project administration, and Funding acquisition. WA: Methodology, Formal analysis, Investigation, Data Curation, Writing—Review & Editing, Visualization, and Project administration. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
We confirm that all methods were carried out under the relevant guidelines and regulations. The authors declare no conflict of interests.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the Faculty of Medicine, Prince of Songkla University (REC: 64-569-3-1), who waived the requirement for informed consent as the patients could not be identified throughout the research process. All stages of the research were conducted in full compliance with the Declaration of Helsinki and Ethical Statements of the Ethics Committee of the Faculty of Medicine, Prince of Songkla University.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pitanupong, J., Aunjitsakul, W. Personal and perceived stigma in relation to diverse domains of quality of life among patients with major depressive disorder having residual symptoms: a hospital-based cross-sectional study in Thailand. Qual Life Res 33, 399–409 (2024). https://doi.org/10.1007/s11136-023-03527-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-023-03527-6