Abstract
Purpose
Because physical-mental comorbidity in children is relatively common, this study tested for response shift (RS) in children with chronic physical illness using a parent-reported measure of child psychopathology.
Methods
Data come from Multimorbidity in Children and Youth across Life-course (MY LIFE), a prospective study of n = 263 children aged 2–16 years with physical illness in Canada. Parents provided information on child psychopathology using the Ontario Child Health Study Emotional Behavioral Scales (OCHS-EBS) at baseline and 24 months. Oort’s structural equation modeling was used to test for different forms of RS in parent-reported assessments between baseline and 24 months. Model fit was evaluated using root mean square error of approximation (RMSEA), comparative fit index (CFI), and standardized root mean residual (SRMR).
Results
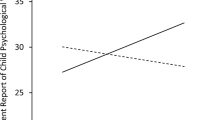
There were n = 215 (81.7%) children with complete data and were included in this analysis. Of these, n = 105 (48.8%) were female and the mean (SD) age was 9.4 (4.2) years. A two-factor measurement model provided good fit to the data [RMSEA (90% CI) = 0.05 (0.01, 0.10); CFI = 0.99; SRMR = 0.03]. Non-uniform recalibration RS was detected on the conduct disorder subscale of the OCHS-EBS. This RS effect had negligible impact on the longitudinal change in externalizing and internalizing disorders construct over time.
Conclusions
Response shift detected on the conduct disorder subscale of the OCHS-EBS, indicated that parents of children with physical illness may recalibrate their responses on child psychopathology over 24 months. Researchers and health professionals should be aware of RS when using the OCHS-EBS to assess child psychopathology over time.


Similar content being viewed by others
Availability of data and materials
Not available.
Code availability
Not available.
References
Van Cleave, J., Gortmaker, S. L., & Perrin, J. M. (2010). Dynamics of obesity and chronic health conditions among children and youth. JAMA, 303(7), 623–630.
Adams, J. S., Chien, A. T., & Wisk, L. E. (2019). Mental illness among youth with chronic physical conditions. Pediatrics, 144(1), 1.
Arrondo, G., Solmi, M., Dragioti, E., Eudave, L., Ruiz-Goikoetxea, M., Ciaurriz-Larraz, A. M., Magallon, S., Carvalho, A. F., Cipriani, A., Fusar-Poli, P., Larsson, H., Correll, C. U., & Cortese, S. (2022). Associations between mental and physical conditions in children and adolescents: An umbrella review. Neuroscience and Biobehavioral Reviews, 137, 104662.
Romano, I., Buchan, C., Baiocco-Romano, L., & Ferro, M. A. (2021). Physical-mental multimorbidity in children and youth: A scoping review. British Medical Journal Open, 11(5), e043124.
Tegethoff, M., Belardi, A., Stalujanis, E., & Meinlschmidt, G. (2015). Association between mental disorders and physical diseases in adolescents from a nationally representative cohort. Psychosomatic Medicine, 77(3), 319–332.
Merikangas, K. R., Calkins, M. E., Burstein, M., He, J. P., Chiavacci, R., Lateef, T., Ruparel, K., Gur, R. C., Lehner, T., Hakonarson, H., & Gur, R. E. (2015). Comorbidity of physical and mental disorders in the neurodevelopmental genomics cohort study. Pediatrics, 135(4), e927-938.
Ferro, M. A. (2016). Major depressive disorder, suicidal behaviour, bipolar disorder, and generalised anxiety disorder among emerging adults with and without chronic health conditions. Epidemiology and Psychiatric Sciences, 25(5), 462–474.
Ferro, M. A., Qureshi, S., Van Lieshout, R. J., Lipman, E. L., Georgiades, K., Gorter, J. W., Timmons, B. W., & Shanahan, L. (2022). Prevalence and correlates of physical-mental multimorbidity in outpatient children from a pediatric hospital in Canada. The Canadian Journal of Psychiatry, 2022, 7067437221074430.
Butler, A., Van Lieshout, R. J., Lipman, E. L., MacMillan, H. L., Gonzalez, A., Gorter, J. W., Georgiades, K., Speechley, K. N., Boyle, M. H., & Ferro, M. A. (2018). Mental disorder in children with physical conditions: A pilot study. British Medical Journal Open, 8(1), e019011.
Canning, E. H., Hanser, S. B., Shade, K. A., & Boyce, W. T. (1992). Mental disorders in chronically ill children: Parent–child discrepancy and physician identification. Pediatrics, 90(5), 692–696.
Boyle, M. H., Duncan, L., Georgiades, K., Bennett, K., Gonzalez, A., Van Lieshout, R. J., Szatmari, P., MacMillan, H. L., Kata, A., Ferro, M. A., Lipman, E. L., & Janus, M. (2017). Classifying child and adolescent psychiatric disorder by problem checklists and standardized interviews. International Journal of Methods in Psychiatric Research, 26(4), e1544.
De Los Reyes, A., & Kazdin, A. E. (2005). Informant discrepancies in the assessment of childhood psychopathology: A critical review, theoretical framework, and recommendations for further study. Psychological Bulletin, 131(4), 483–509.
Georgiades, K., Duncan, L., Wang, L., Comeau, J., Boyle, M. H., & Ontario Child Health Study, T. (2019). Six-month prevalence of mental disorders and service contacts among children and youth in Ontario: Evidence from the 2014 Ontario Child Health Study. The Canadian Journal of Psychiatry, 64(4), 246–255.
Duncan, L., Boyle, M., Ferro, M. A., Georgiades, K., Van Lieshout, R. J., Bennett, K., Janus, M., Lipman, E., MacMillan, H., & Szatmari, P. (2018). Psychometric evaluation of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID). Psychological Assessment, 30(7), 916–928.
Sprangers, M. A., & Schwartz, C. E. (1999). Integrating response shift into health-related quality of life research: A theoretical model. Social Science and Medicine, 48(11), 1507–1515.
Sajobi, T. T., Brahmbatt, R., Lix, L. M., Zumbo, B. D., & Sawatzky, R. (2018). Scoping review of response shift methods: Current reporting practices and recommendations. Quality of Life Research, 27(5), 1133–1146.
Vanier, A., Oort, F. J., McClimans, L., Ow, N., Gulek, B. G., Bohnke, J. R., Sprangers, M., Sebille, V., Mayo, N., & Response Shift—In Sync Working, G. (2021). Response shift in patient-reported outcomes: Definition, theory, and a revised model. Quality of Life Research, 30(12), 3309–3322.
Rapkin, B. D., & Schwartz, C. E. (2004). Toward a theoretical model of quality-of-life appraisal: Implications of findings from studies of response shift. Health and Quality of Life Outcomes, 2, 14.
Ortega-Gomez, E., Vicente-Galindo, P., Martin-Rodero, H., & Galindo-Villardon, P. (2022). Detection of response shift in health-related quality of life studies: A systematic review. Health and Quality of Life Outcomes, 20(1), 20.
Brinksma, A., Tissing, W. J., Sulkers, E., Kamps, W. A., Roodbol, P. F., & Sanderman, R. (2014). Exploring the response shift phenomenon in childhood patients with cancer and its effect on health-related quality of life. Oncology Nursing Forum, 41(1), 48–56.
Sajobi, T. T., Speechley, K. N., Liang, Z., Goodwin, S. W., Ferro, M. A., & Wiebe, S. (2017). Response shift in parents’ assessment of health-related quality of life of children with new-onset epilepsy. Epilepsy and Behavior, 75, 97–101.
Gandhi, P. K., Schwartz, C. E., Reeve, B. B., DeWalt, D. A., Gross, H. E., & Huang, I. C. (2016). An item-level response shift study on the change of health state with the rating of asthma-specific quality of life: A report from the PROMIS[(R)] Pediatric Asthma Study. Quality of Life Research, 25(6), 1349–1359.
Postulart, D., & Adang, E. M. (2000). Response shift and adaptation in chronically ill patients. Medical Decision Making, 20(2), 186–193.
Kim-Cohen, J., Caspi, A., Moffitt, T. E., Harrington, H., Milne, B. J., & Poulton, R. (2003). Prior juvenile diagnoses in adults with mental disorder: Developmental follow-back of a prospective-longitudinal cohort. Archives of General Psychiatry, 60(7), 709–717.
Ferro, M. A., Gorter, J. W., & Boyle, M. H. (2015). Trajectories of depressive symptoms in Canadian emerging adults. American Journal of Public Health, 105(11), 2322–2327.
Ferro, M. A., Gorter, J. W., & Boyle, M. H. (2015). Trajectories of depressive symptoms during the transition to young adulthood: The role of chronic illness. Journal of Affective Disorders, 174(2015), 594–601.
Ferro, M. A., Lipman, E. L., Van Lieshout, R. J., Gorter, J. W., Shanahan, L., Boyle, M., Georgiades, K., & Timmons, B. (2019). Multimorbidity in children and youth across the life-course (MY LIFE): Protocol of a Canadian prospective study. British Medical Journal Open, 9(11), e034544.
Ferro, M. A., Lipman, E. L., Van Lieshout, R. J., Timmons, B., Shanahan, L., Gorter, J. W., Georgiades, K., & Boyle, M. (2021). Cohort profile: Multimorbidity in children and youth across the life-course (MY LIFE) study. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 30(2), 104–115.
Duncan, L., Georgiades, K., Wang, L., Comeau, J., Ferro, M. A., Van Lieshout, R. J., Szatmari, P., Bennett, K., MacMillan, H. L., Lipman, E. L., Janus, M., Kata, A., & Boyle, M. H. (2019). The 2014 Ontario Child Health study emotional behavioural scales (OCHS-EBS) part I: A checklist for dimensional measurement of selected DSM-5 Disorders. Canadian Journal of Psychiatry, 64(6), 423–433.
Boyle, M. H., Offord, D. R., Racine, Y., Fleming, J. E., Szatmari, P., & Sanford, M. (1993). Evaluation of the revised Ontario Child Health Study scales. Journal of Child Psychology and Psychiatry, 34(2), 189–213.
Boyle, M. H., Duncan, L., Georgiades, K., Wang, L., Comeau, J., Ferro, M. A., Van Lieshout, R. J., Szatmari, P., MacMillan, H. L., Bennett, K., Janus, M., Lipman, E. L., & Kata, A. (2019). The 2014 Ontario Child Health Study Emotional Behavioural Scales (OCHS-EBS) Part II: psychometric adequacy for categorical measurement of selected DSM-5 Disorders. Canadian Journal of Psychiatry, 64(6), 434–442.
Kline, R. B. (2016). Principles and practice of structural equation modeling (4th ed.). The Guilford Press.
Cohen, J. (1992). A power primer. Psychological Bulletin, 112(1), 155–159.
Browne, M. W., & Cudeck, R. (1993). Alternative ways of assessing model fit. In K. A. Bollen & J. S. Long (Eds.), Testing structural equation models. Sage.
Bentler, P. M. (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107(2), 238–246.
Hu, L., & Bentler, P. M. (1999). Cut-off criteria for fit indices in covariance structure analysis: Conventional critieria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55.
Hooper, D., Coughlan, J., & Mullen, M. R. (2008). Structural equation modelling: Guidelines for determining model fit. Electronic Journal of Business Research Methods, 6(1), 53–60.
Bollen, K. A. (1989). A new incremental fit index for general structural equation models. Sociological Methods and Research, 17(3), 303–316.
Oort, F. J. (2005). Using structural equation modeling to detect response shifts and true change. Quality of Life Research, 14(3), 587–598.
Chen, F. F. (2007). Sensitivity of goodness of fit indices to lack of measurement invariance. Structural Equation Modeling: A Multidisciplinary Journal, 14(3), 464–504.
Oreel, T. H., Nieuwkerk, P. T., Hartog, I. D., Netjes, J. E., Vonk, A. B. A., Lemkes, J., van Laarhoven, H. W. M., Scherer-Rath, M., Henriques, J. P. S., Oort, F. J., Sprangers, M. A. G., & Verdam, M. G. E. (2022). Response shift after coronary revascularization. Quality of Life Research, 31(2), 437–450.
McDonald, E., Whitney, S., Horricks, L., Lipman, E. L., & Ferro, M. A. (2021). Parent–child agreement on the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID). Journal of Canadian Academy of Child and Adolescent Psychiatry, 30(4), 264–272.
Ferro, M. A., Qureshi, S. A., Shanahan, L., Otto, C., & Ravens-Sieberer, U. (2021). Health-related quality of life in children with and without physical-mental multimorbidity. Quality of Life Research, 30(12), 3449–3461.
Oltean, I. I., & Ferro, M. A. (2019). Agreement of child and parent-proxy reported health-related quality of life in children with mental disorder. Quality of Life Research, 28(3), 703–712.
Council on Children with, D., & Medical Home Implementation Project Advisory, C. (2014). Patient- and family-centered care coordination: A framework for integrating care for children and youth across multiple systems. Pediatrics, 133(5), e1451-1460.
Sturgiss, E. A., Peart, A., Richard, L., Ball, L., Hunik, L., Chai, T. L., Lau, S., Vadasz, D., Russell, G., & Stewart, M. (2022). Who is at the centre of what? A scoping review of the conceptualisation of “centredness” in healthcare. British Medical Journal Open, 12(5), e059400.
Kindratt, T. B., Lark, P., Ray, M., & Brannon, G. E. (2022). Disparities in patient- and family-centered care among children with health conditions. Journal of Patient Experience, 9, 23743735221092496.
Bele, S., Chugh, A., Mohamed, B., Teela, L., Haverman, L., & Santana, M. J. (2020). Patient-reported outcome measures in routine pediatric clinical care: A systematic review. Frontiers in Pediatrics, 8, 364.
Edbrooke-Childs, J., & Deighton, J. (2020). Problem severity and waiting times for young people accessing mental health services. BJPsych Open, 6(6), e118.
McGorry, P. D., Mei, C., Chanen, A., Hodges, C., Alvarez-Jimenez, M., & Killackey, E. (2022). Designing and scaling up integrated youth mental health care. World Psychiatry, 21(1), 61–76.
Kowalewski, K., McLennan, J. D., & McGrath, P. J. (2011). A preliminary investigation of wait times for child and adolescent mental health services in Canada. Journal of Canadian Academy of Child and Adolescent Psychiatry, 20(2), 112–119.
Stormacq, C., Van den Broucke, S., & Wosinski, J. (2019). Does health literacy mediate the relationship between socioeconomic status and health disparities? Integrative review. Health Promotion International, 34(5), E1–E17.
Ferro, M. A., Basque, D., Elgie, M., & Dol, M. (2022). Agreement of the 12-item World Health Organization Disability Assessment Schedule (WHODAS) 2.0 in parents and youth with physical illness living in Canada. Disability and Rehabilitation, 2022, 1–10.
Tompke, B. K., & Ferro, M. A. (2021). Measurement invariance and informant discrepancies of the KIDSCREEN-27 in children with mental disorder. Applied Research in Quality of Life, 16(4), 891–910.
Norman, G. R., Sloan, J. A., & Wyrwich, K. W. (2003). Interpretation of changes in health-related quality of life: The remarkable universality of half a standard deviation. Medical Care, 41(5), 582–592.
Wyrwich, K. W., Tierney, W. M., & Wolinsky, F. D. (1999). Further evidence supporting an SEM-based criterion for identifying meaningful intra-individual changes in health-related quality of life. Journal of Clinical Epidemiology, 52(9), 861–873.
Blanchin, M., Sebille, V., Guilleux, A., & Hardouin, J. B. (2016). The Guttman errors as a tool for response shift detection at subgroup and item levels. Quality of Life Research, 25(6), 1385–1393.
Guilleux, A., Blanchin, M., Vanier, A., Guillemin, F., Falissard, B., Schwartz, C. E., Hardouin, J. B., & Sebille, V. (2015). RespOnse Shift ALgorithm in Item response theory (ROSALI) for response shift detection with missing data in longitudinal patient-reported outcome studies. Quality of Life Research, 24(3), 553–564.
Verdam, M. G., Oort, F. J., & Sprangers, M. A. (2016). Using structural equation modeling to detect response shifts and true change in discrete variables: An application to the items of the SF-36. Quality of Life Research, 25(6), 1361–1383.
Acknowledgements
The authors gratefully acknowledge the children, parents, and health professionals and their staff without whose participation this study would not have been possible. We thank Jessica Zelman, Robyn Wojcicki, and Charlene Attard for coordinating the study.
Funding
This study was funded by the Canadian Institutes of Health Research (PJT-148602). Dr. Ferro holds the Canada Research Chair in Youth Mental Health.
Author information
Authors and Affiliations
Contributions
Dr. MAF conceptualized and designed the study, obtained study funding, supervised data collection, and contributed to writing the manuscript. Dr. TTS conceptualized and supervised analysis of the data, interpreted findings, and contributed to writing the manuscript. Dr. OFA conducted the data analysis, interpreted findings, and contributed to writing the manuscript. Ms. GKD conducted the literature review and contributed to writing the manuscript. All authors critically reviewed the manuscript for important intellectual content, edited the manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest relevant to this article to disclose.
Consent to participate
All participants 16 years and older provided informed consent, children 7–15 provided assent, and children 6 and younger were consented by their parents.
Consent for publication
Not applicable.
Ethics approval
MY LIFE received ethical approval from the University of Waterloo Human Research Ethics Board (ORE-22183) and the Hamilton Integrated Research Ethics Board (2797).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sajobi, T.T., Ayilara, O.F., Dhuga, G.K. et al. Response shift in parent-reported psychopathology in children with chronic physical illness. Qual Life Res 32, 3099–3108 (2023). https://doi.org/10.1007/s11136-023-03458-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-023-03458-2