Abstract
Background
Stroke survivors face various problems that affect their health-related quality of life (HRQoL). Reduced activities of daily living (ADL) may contribute to post-stroke depression (PSD) and low HRQoL, and depression might be associated with low HRQoL. However, these relationships are not well known. This study aimed to analyze correlations among ADL, PSD, and HRQoL in stroke survivors and further explore the mediating role of PSD between ADL and HRQoL.
Methods
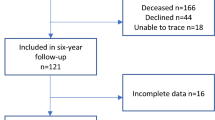
This study utilized meta-analytic structural equation modeling (MASEM) on systematically searched articles from six electronic databases, namely PubMed, Embase, the Cochrane Library, China National Knowledge Infrastructure (China), Wanfang database (China), and SinoMed (China), from inception up to July 31, 2021. Two researchers independently assessed study eligibility, and data from the eligible studies were encoded and assessed for quality. MASEM was utilized to examine correlations among ADL, PSD, and HRQoL, with an estimation of a pooled correlation matrix under a random-effects model. The matrix was directly fitted to a structural equation model using webMASEM.
Results
In total, 8580 articles were screened, and data from 27 studies involving 33 effect sizes were used in the MASEM analysis. Correlations among the three variables were significant (both P < 0.01). Furthermore, PSD partially mediated the correlation between ADL and HRQoL (β = 0.24, 95% confidence interval 0.15–0.30).
Conclusions
The findings suggest that both decreased ADL and PSD may reduce HRQoL, while a decrease in ADL tends to cause depression after stroke. Therefore, ADL and PSD reductions should be improved to achieve better HRQoL of stroke survivors. Future studies should continue to discuss other factors affecting HRQoL to achieve optimal recovery in stroke survivors.


Similar content being viewed by others

Abbreviations
- MASEM:
-
Meta-analytic structural equation modeling
- ADL:
-
Activities of daily living
- PSD:
-
Post-stroke depression
- QoL:
-
Quality of life
- HRQoL:
-
Health-related quality of life
- CMV:
-
Common method variance
References
Johnson, W., Onuma, O., Owolabi, M., & Sachdev, S. (2016). Stroke: A global response is needed. Bulletin of the World Health Organization, 94(9), 634-634A. https://doi.org/10.2471/BLT.16.181636
GBD. (2021). Global, regional, and national burden of stroke and its risk factors, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. The Lancet Neurology, 20(10), 795–820. https://doi.org/10.1016/s1474-4422(21)00252-0
Wan, X., Chau, J. P. C., Mou, H., & Liu, X. (2021). Effects of peer support interventions on physical and psychosocial outcomes among stroke survivors: A systematic review and meta-analysis. International Journal of Nursing Studies, 121, 104001. https://doi.org/10.1016/j.ijnurstu.2021.104001
Ahmed, T., Kumar, R., & Bahurupi, Y. (2020). Factors affecting quality of life among post-stroke patients in the sub-Himalayan region. Journal of Neurosciences in Rural Practice, 11(4), 616–622. https://doi.org/10.1055/s-0040-1716927
Oliveira, C., de Silva, N. T., Ungar, W. J., Bayoumi, A. M., Avitzur, Y., Hoch, J. S., et al. (2020). Health-related quality of life in neonates and infants: A conceptual framework. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 29(5), 1159–1168. https://doi.org/10.1007/s11136-020-02432-6
Zhu, W., & Jiang, Y. (2019). Determinants of quality of life in patients with hemorrhagic stroke; A path analysis. Medicine (United States). https://doi.org/10.1097/MD.0000000000013928
Wilson, I. B., & Cleary, P. D. (1995). Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA, 273(1), 59–65.
Mlinac, M. E., & Feng, M. C. (2016). Assessment of activities of daily living, self-care, and independence. Archives of Clinical Neuropsychology, 31(6), 506–516. https://doi.org/10.1093/arclin/acw049
Zhang, Q., Schwade, M., Smith, Y., Wood, R., & Young, L. (2020). Exercise-based interventions for post-stroke social participation: A systematic review and network meta-analysis. International Journal of Nursing Studies, 111, 103738. https://doi.org/10.1016/j.ijnurstu.2020.103738
Medeiros, G. C., Roy, D., Kontos, N., & Beach, S. R. (2020). Post-stroke depression: A 2020 updated review. General Hospital Psychiatry, 66, 70–80. https://doi.org/10.1016/j.genhosppsych.2020.06.011
Mitchell, A. J., Sheth, B., Gill, J., Yadegarfar, M., Stubbs, B., Yadegarfar, M., et al. (2017). Prevalence and predictors of post-stroke mood disorders: A meta-analysis and meta-regression of depression, anxiety and adjustment disorder. General Hospital Psychiatry, 47, 48–60. https://doi.org/10.1016/j.genhosppsych.2017.04.001
Kirkevold, M., Bronken, B. A., Martinsen, R., & Kvigne, K. (2012). Promoting psychosocial well-being following a stroke: Developing a theoretically and empirically sound complex intervention. International Journal of Nursing Studies, 49(4), 386–397. https://doi.org/10.1016/j.ijnurstu.2011.10.006
He, M., Ma, J., Ren, Z., Zhou, G., Gong, P., Liu, M., et al. (2019). Association between activities of daily living disability and depression symptoms of middle-aged and older Chinese adults and their spouses: A community based study. Journal of Affective Disorders, 242, 135–142. https://doi.org/10.1016/j.jad.2018.08.060
De Ryck, A., Brouns, R., Fransen, E., Geurden, M., Van Gestel, G., Wilssens, I., et al. (2013). A prospective study on the prevalence and risk factors of poststroke depression. Cerebrovascular Diseases Extra, 3(1), 1–13. https://doi.org/10.1159/000345557
Kawada, S., & Goto, R. (2017). Relationship between psychophysiological factors and prognosis for activities of daily living in patients with stroke in a recovery rehabilitation unit: A preliminary study. Journal of Physical Therapy Science, 29(12), 2206–2209. https://doi.org/10.1589/jpts.29.2206
Vojtikiv-Samoilovska, D., & Arsovska, A. (2018). Prevalence and predictors of depression after stroke—Results from a prospective study. Open Access Macedonian Journal of Medical Sciences, 6(5), 824–828. https://doi.org/10.3889/oamjms.2018.182
Souza, A. C., Rocha, M. O., Teixeira, A. L., Dias Júnior, J. O., Sousa, L. A., & Nunes, M. C. (2013). Depressive symptoms and disability in chagasic stroke patients: Impact on functionality and quality of life. Journal of the Neurological Sciences, 324(1–2), 34–37. https://doi.org/10.1016/j.jns.2012.09.022
Hunter, J., & Schmidt, F. (2004). Methods of meta-analysis corrected error and bias in research findings. SAGE Publications Inc.
Langhammer, B., Stanghelle, J. K., & Lindmark, B. (2008). Exercise and health-related quality of life during the first year following acute stroke. A randomized controlled trial. Brain Injury, 22(2), 135–145. https://doi.org/10.1080/02699050801895423
Kim, J. S., Choi-Kwon, S., Kwon, S. U., Lee, H. J., Park, K. A., & Seo, Y. S. (2005). Factors affecting the quality of life after ischemic stroke: Young versus old patients. Journal of Clinical Neurology (Seoul, Korea), 1(1), 59–68. https://doi.org/10.3988/jcn.2005.1.1.59
Hartley, T., Burger, M., & Inglis-Jassiem, G. (2022). Post stroke health-related quality of life, stroke severity and function: A longitudinal cohort study. African Journal of Disability, 11, 947. https://doi.org/10.4102/ajod.v11i0.947
Naess, H., Lunde, L., & Brogger, J. (2012). The effects of fatigue, pain, and depression on quality of life in ischemic stroke patients: The Bergen Stroke Study. Vascular Health and Risk Management, 8, 407–413. https://doi.org/10.2147/vhrm.S32780
Bello, U. M., Chutiyami, M., Salihu, D., Abdu, S. I., Tafida, B. A., Jabbo, A. A., et al. (2021). Quality of life of stroke survivors in Africa: A systematic review and meta-analysis. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 30(1), 1–19. https://doi.org/10.1007/s11136-020-02591-6
Kim, E. S., Kim, J. W., Kang, H. J., Bae, K. Y., Kim, S. W., Kim, J. T., et al. (2018). Longitudinal impact of depression on quality of life in stroke patients. Psychiatry Investigation, 15(2), 141–146. https://doi.org/10.30773/pi.2017.10.11
Haghgoo, H. A., Pazuki, E. S., Hosseini, A. S., & Rassafiani, M. (2013). Depression, activities of daily living and quality of life in patients with stroke. Journal of the Neurological Sciences, 328(1–2), 87–91. https://doi.org/10.1016/j.jns.2013.02.027
Chan, S. H., Pan, Y., Xu, Y., & Yeung, K. C. (2021). Life satisfaction of 511 elderly Chinese stroke survivors: Moderating roles of social functioning and depression in a quality of life model. Clinical Rehabilitation, 35(2), 302–313. https://doi.org/10.1177/0269215520956908
Ayerbe, L., Ayis, S., Wolfe, C. D., & Rudd, A. G. (2013). Natural history, predictors and outcomes of depression after stroke: Systematic review and meta-analysis. The British Journal of Psychiatry: The Journal of Mental Science, 202(1), 14–21. https://doi.org/10.1192/bjp.bp.111.107664
Jak, S., & Cheung, M. W. (2020). Meta-analytic structural equation modeling with moderating effects on SEM parameters. Psychological Methods, 25(4), 430–455. https://doi.org/10.1037/met0000245
Kraft, P., & Bausch, A. (2016). How do transformational leaders promote exploratory and exploitative innovation? Examining the black box through MASEM. Journal of Product Innovation Management, 33(6), 687–707. https://doi.org/10.1111/jpim.12335
Gómez-Gallego, M., Gómez-García, J., & Ato-Lozano, E. (2017). The mediating role of depression in the association between disability and quality of life in Alzheimer’s disease. Aging & Mental Health, 21(2), 163–172. https://doi.org/10.1080/13607863.2015.1093603
Schwarzer, R. (1988). Meta-analysis programs. Behavior Research Methods, Instruments, & Computers, 20(3), 338–338. https://doi.org/10.3758/BF03203853
Peterson, R. A., & Brown, S. P. (2005). On the use of beta coefficients in meta-analysis. The Journal of Applied Psychology, 90(1), 175–181. https://doi.org/10.1037/0021-9010.90.1.175
Rupinski, M. T., & Dunlap, W. P. (2016). Approximating Pearson product-moment correlations from Kendall’s tau and Spearman’s rho. Educational and Psychological Measurement, 56(3), 419–429. https://doi.org/10.1177/0013164496056003004
Yonker, J. E., Schnabelrauch, C. A., & Dehaan, L. G. (2012). The relationship between spirituality and religiosity on psychological outcomes in adolescents and emerging adults: A meta-analytic review. Journal of Adolescence, 35(2), 299–314. https://doi.org/10.1016/j.adolescence.2011.08.010
Tehrani, H. D., & Yamini, S. (2020). Dataset of parenting practices, self-control and anti-social behaviors: Meta-analytic structural equation modeling. Data in Brief, 32, 106114. https://doi.org/10.1016/j.dib.2020.106114
Cicolini, G., Comparcini, D., & Simonetti, V. (2014). Workplace empowerment and nurses’ job satisfaction: A systematic literature review. Journal of Nursing Management, 22(7), 855–871. https://doi.org/10.1111/jonm.12028
Hunter, J., & Hamilton, M. (2006). The advantages of using standardized scores in causal analysis. Human Communication Research, 28, 552–561. https://doi.org/10.1111/j.1468-2958.2002.tb00823.x
Cheung, M. W., & Cheung, S. F. (2016). Random-effects models for meta-analytic structural equation modeling: Review, issues, and illustrations. Research Synthesis Methods, 7(2), 140–155. https://doi.org/10.1002/jrsm.1166
Borenstein, M., Hedges, L. V., Higgins, J. P. T., & Rothstein, H. R. (2009). Introduction to meta-analysis. Wiley.
Viswesvaran, C., & Ones, D. (1995). Theory testing: Combining psychometric meta-analysis and structural equations modeling. Personnel Psychology, 48, 865–885. https://doi.org/10.1111/j.1744-6570.1995.tb01784.x
Jak, S., Li, H., Kolbe, L., de Jonge, H., & Cheung, M. W. (2021). Meta-analytic structural equation modeling made easy: A tutorial and web application for one-stage MASEM. Research Synthesis Methods, 12(5), 590–606. https://doi.org/10.1002/jrsm.1498
Morris, J. H., van Wijck, F., Joice, S., & Donaghy, M. (2013). Predicting health related quality of life 6 months after stroke: The role of anxiety and upper limb dysfunction. Disability and Rehabilitation, 35(4), 291–299. https://doi.org/10.3109/09638288.2012.691942
Gunaydin, R., Karatepe, A. G., Kaya, T., & Ulutas, O. (2011). Determinants of quality of life (QoL) in elderly stroke patients: A short-term follow-up study. Archives of Gerontology and Geriatrics, 53(1), 19–23. https://doi.org/10.1016/j.archger.2010.06.004
Mou, H., Wong, M. S., & Chien, W. T. P. (2021). Effectiveness of dyadic psychoeducational intervention for stroke survivors and family caregivers on functional and psychosocial health: A systematic review and meta-analysis. International Journal of Nursing Studies, 120, 103969. https://doi.org/10.1016/j.ijnurstu.2021.103969
Wang, H., Wen, Q., Chen, X., Chen, L., & Li, H. (2016). Analysis of depression status and influencing factors in senile stroke patients. Chinese Journal of Rehabilitation Medicine, 27(4), 339–343. https://doi.org/10.16460/j.issn1008-9969.2016.23.048
Byeon, H., & Koh, H. W. (2016). The relationship between communication activities of daily living and quality of life among the elderly suffering from stroke. Journal of Physical Therapy Science, 28(5), 1450–1453. https://doi.org/10.1589/jpts.28.1450
Žikić, T. R., Mirjana, J., Semnic, M., Slankamenac, P., Žarkov, M., & Žikić, M. (2014). The effect of post stroke depression on functional outcome and quality of life. Acta Clinica Croatica, 53(3), 294–301.
Pan, J. H., Song, X. Y., Lee, S. Y., & Kwok, T. (2008). Longitudinal analysis of quality of life for stroke survivors using latent curve models. Stroke, 39(10), 2795–2802. https://doi.org/10.1161/strokeaha.108.515460
Perna, R., & Harik, L. (2020). The role of rehabilitation psychology in stroke care described through case examples. NeuroRehabilitation, 46(2), 195–204. https://doi.org/10.3233/nre-192970
Ahlsiö, B., Britton, M., Murray, V., & Theorell, T. (1984). Disablement and quality of life after stroke. Stroke, 15(5), 886–890. https://doi.org/10.1161/01.str.15.5.886
Salter, K., Foley, N., & Teasell, R. (2010). Social support interventions and mood status post stroke: A review. International Journal of Nursing Studies, 47(5), 616–625. https://doi.org/10.1016/j.ijnurstu.2009.12.002
Jak, S. (2015). Introduction to meta-analysis and structural equation modeling. In S. Jak (Ed.), Meta-analytic structural equation modelling. SpringerBriefs in research synthesis and meta-analysis. Springer. https://doi.org/10.1007/978-3-319-27174-3_1
Lo Buono, V., Corallo, F., Bramanti, P., & Marino, S. (2017). Coping strategies and health-related quality of life after stroke. Journal of Health Psychology, 22(1), 16–28. https://doi.org/10.1177/1359105315595117
da Rocha, N. S., Power, M. J., Bushnell, D. M., & Fleck, M. P. (2009). Is there a measurement overlap between depressive symptoms and quality of life? Comprehensive Psychiatry, 50(6), 549–555. https://doi.org/10.1016/j.comppsych.2008.11.015
Jakobsen, M., & Jensen, R. (2015). Common method bias in public management studies. International Public Management Journal. https://doi.org/10.1080/10967494.2014.997906
George, B., & Pandey, S. K. (2017). We know the Yin-But where is the Yang? Toward a balanced approach on common source bias in public administration scholarship. Review of Public Personnel Administration, 37(2), 245–270. https://doi.org/10.1177/0734371x17698189
Conway, J. M., & Lance, C. E. (2010). What reviewers should expect from authors regarding common method bias in organizational research. Journal of Business and Psychology, 25(3), 325–334. https://doi.org/10.1007/s10869-010-9181-6
Funding
This work was supported by the Natural Science Foundation of Shandong province (Grant No. ZR2021MG031).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interests.
Research involving human and/or animal participants
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, J., Yang, L., Lv, R. et al. Mediating effect of post-stroke depression between activities of daily living and health-related quality of life: meta-analytic structural equation modeling. Qual Life Res 32, 331–338 (2023). https://doi.org/10.1007/s11136-022-03225-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-022-03225-9