Abstract
Purpose
Health-related quality of life (HRQL) has been identified as one of the core outcomes most important to assess following pediatric critical care, yet there are no data on the use of HRQL in pediatric critical care research. We aimed to determine the HRQL instruments most commonly used to assess children surviving critical care and describe study methodology, patient populations, and instrument characteristics to identify areas of deficiency and guide investigators conducting HRQL research.
Methods
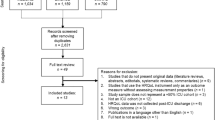
We queried PubMed, EMBASE, PsycINFO, Cumulative Index of Nursing and Allied Health Literature, and the Cochrane Registry for studies evaluating pediatric critical care survivors published 1970–2017. We used dual review for article selection and data extraction.
Results
Of 60,349 citations, 66 articles met inclusion criteria. The majority of studies were observational (89.4%) and assessed HRQL at one post-discharge time-point (86.4%), and only 10.6% of studies included a baseline assessment. Time to the first follow-up assessment ranged from 1 month to 10 years post-hospitalization (median 3 years, IQR 0.5–6). For 26 prospective studies, the median follow-up time was 0.5 years [IQR 0.25–1]. Parent/guardian proxy-reporting was used in 83.3% of studies. Fifteen HRQL instruments were employed, with four used in >5% of articles: the Health Utility Index (n = 22 articles), the Pediatric Quality of Life Inventory (n = 17), the Child Health Questionnaire (n = 16), and the 36-Item Short Form Survey (n = 9).
Conclusion
HRQL assessment in pediatric critical care research has been centered around four instruments, though existing literature is limited by minimal longitudinal follow-up and infrequent assessment of baseline HRQL.

Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
Burns, J. P., Sellers, D. E., Meyer, E. C., Lewis-Newby, M., & Truog, R. D. (2014). Epidemiology of death in the PICU at five U.S. teaching hospitals*. Critical Care Medicine, 42(9), 2101–2108. doi:https://doi.org/10.1097/CCM.0000000000000498
Pinto, N. P., Rhinesmith, E. W., Kim, T. Y., Ladner, P. H., & Pollack, M. M. (2017). Long-term function after pediatric critical illness: Results from the survivor outcomes study. Pediatric Critical Care Medicine, 18(3), e122–e130. https://doi.org/10.1097/pcc.0000000000001070
Manning, J. C., Pinto, N. P., Rennick, J. E., Colville, G., & Curley, M. A. Q. (2018). Conceptualizing post intensive care syndrome in children-the PICS-p framework. Pediatric Critical Care Medicine, 19(4), 298–300. https://doi.org/10.1097/pcc.0000000000001476
Rennick, J. E., & Childerhose, J. E. (2015). Redefining success in the PICU: New patient populations shift targets of care. Pediatrics, 135(2), e289-291. https://doi.org/10.1542/peds.2014-2174
Graham, R. J. (2005). An opportunity: Critical care beyond the intensive care unit. Pediatric Critical Care Medicine, 6(3), 327–328.
Maddux, A. B., Pinto, N., Fink, E. L., Hartman, M. E., Nett, S., Biagas, K., et al. (2020). Postdischarge outcome domains in pediatric critical care and the instruments used to evaluate them: A scoping review. Critical Care Medicine, 48(12), e1313–e1321. https://doi.org/10.1097/CCM.0000000000004595
Fink, E. L., Jarvis, J. M., Maddux, A. B., Pinto, N., Galyean, P., Olson, L. M., et al. (2020). Development of a core outcome set for pediatric critical care outcomes research. Contemporary Clinical Trials, 91, 105968. https://doi.org/10.1016/j.cct.2020.105968
Fink, E. L., Maddux, A. B., Pinto, N., Sorenson, S., Notterman, D., Dean, J. M., et al. (2020). A core outcome set for pediatric critical care. Critical Care Medicine. https://doi.org/10.1097/ccm.0000000000004660
Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J. G. (2009). Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Iwashyna, T. J., & Netzer, G. (2012). The burdens of survivorship: An approach to thinking about long-term outcomes after critical illness. Seminars in Respiratory and Critical Care Medicine, 33(4), 327–338. https://doi.org/10.1055/s-0032-1321982
Feeny, D., Furlong, W., Boyle, M., & Torrance, G. W. (1995). Multi-attribute health status classification systems Health Utilities Index. Pharmacoeconomics, 7(6), 490–502. https://doi.org/10.2165/00019053-199507060-00004
Varni, J. W., Seid, M., & Rode, C. A. (1999). The PedsQL: Measurement model for the pediatric quality of life inventory. Medical Care, 37(2), 126–139.
Landgraf, J. M., Maunsell, E., Speechley, K. N., Bullinger, M., Campbell, S., Abetz, L., et al. (1998). Canadian-French, German and UK versions of the Child Health Questionnaire: Methodology and preliminary item scaling results. Quality of Life Research, 7(5), 433–445. https://doi.org/10.1023/a:1008810004694
Ware, J. E., Jr., & Sherbourne, C. D. (1992). The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care, 30(6), 473–483.
Vogels, T., Verrips, G. H., Verloove-Vanhorick, S. P., Fekkes, M., Kamphuis, R. P., Koopman, H. M., et al. (1998). Measuring health-related quality of life in children: The development of the TACQOL parent form. Quality of Life Research, 7(5), 457–465. https://doi.org/10.1023/a:1008848218806
Achenbach, T. M. (2001). Manual for the ASEBA school-age forms and profiles. University of Vermont Research Center for Children, Youth, and Families.
Anderson, J. P., Kaplan, R. M., Berry, C. C., Bush, J. W., & Rumbaut, R. G. (1989). Interday reliability of function assessment for a health status measure. The quality of well-being scale. Medical Care, 27(11), 1076–1083. https://doi.org/10.1097/00005650-198911000-00008
Coster, W., Bedell, G., Law, M., Khetani, M. A., Teplicky, R., Liljenquist, K., et al. (2011). Psychometric evaluation of the participation and environment measure for children and youth. Developmental Medicine and Child Neurology, 53(11), 1030–1037. https://doi.org/10.1111/j.1469-8749.2011.04094.x
McKenna, S. P., Doward, L. C., Alonso, J., Kohlmann, T., Niero, M., Prieto, L., et al. (1999). The QoL-AGHDA: An instrument for the assessment of quality of life in adults with growth hormone deficiency. Quality of Life Research, 8(4), 373–383. https://doi.org/10.1023/a:1008987922774
Gemke, R. J., & Bonsel, G. J. (1996). Reliability and validity of a comprehensive health status measure in a heterogeneous population of children admitted to intensive care. Journal of Clinical Epidemiology, 49(3), 327–333. https://doi.org/10.1016/0895-4356(95)00528-5
Aspesberro, F., Fesinmeyer, M. D., Zhou, C., Zimmerman, J. J., & Mangione-Smith, R. (2016). Construct validity and responsiveness of the pediatric quality of life inventory 4.0 generic core scales and infant scales in the PICU. Pediatric Critical Care Medicine, 17(6), e272–e279. https://doi.org/10.1097/PCC.0000000000000727
Merritt, C., Menon, K., Agus, M. S. D., Choong, K., McNally, D., O’Hearn, K., et al. (2018). Beyond survival: Pediatric critical care interventional trial outcome measure preferences of families and healthcare professionals. Pediatric Critical Care Medicine, 19(2), e105–e111. https://doi.org/10.1097/pcc.0000000000001409
Spronk, I., Legemate, C. M., Polinder, S., & van Baar, M. E. (2018). Health-related quality of life in children after burn injuries: A systematic review. Journal of Trauma and Acute Care Surgery, 85(6), 1110–1118. https://doi.org/10.1097/ta.0000000000002072
Zimmerman, J. J., Banks, R., Berg, R. A., Zuppa, A., Newth, C. J., Wessel, D., et al. (2020). Trajectory of mortality and health-related quality of life morbidity following community-acquired pediatric septic shock. Critical Care Medicine, 48(3), 329–337. https://doi.org/10.1097/CCM.0000000000004123
Killien, E. Y., Watson, R. S., & Zimmerman, J. J. (2018). Inherent value of baseline measures when assessing the trajectory of health-related quality of life among children surviving critical illness. Intensive Care Medicine, 44(11), 1979–1981. https://doi.org/10.1007/s00134-018-5388-1
Killien, E. Y., Farris, R. W. D., Watson, R. S., Dervan, L. A., & Zimmerman, J. J. (2019). Health-related quality of life among survivors of pediatric sepsis. Pediatric Critical Care Medicine, 20(6), 501–509. https://doi.org/10.1097/PCC.0000000000001886
Edwards, J. D., Houtrow, A. J., Vasilevskis, E. E., Rehm, R. S., Markovitz, B. P., Graham, R. J., et al. (2012). Chronic conditions among children admitted to U.S. pediatric intensive care units: Their prevalence and impact on risk for mortality and prolonged length of stay*. Critical Care Medicine, 40(7), 2196–2203. doi:https://doi.org/10.1097/CCM.0b013e31824e68cf.
Kyosti, E., Ala-Kokko, T. I., Ohtonen, P., Peltoniemi, O., Rautiainen, P., Kataja, J., et al. (2018). Factors associated with health-related quality of life 6 years after ICU discharge in a Finnish paediatric population: A cohort study. Intensive Care Medicine, 44(9), 1378–1387. https://doi.org/10.1007/s00134-018-5296-4
Watson, R. S., Asaro, L. A., Hertzog, J. H., Sorce, L. R., Kachmar, A. G., Dervan, L. A., et al. (2018). Long-term outcomes after protocolized sedation versus usual care in ventilated pediatric patients. American Journal of Respiratory and Critical Care Medicine, 197(11), 1457–1467. https://doi.org/10.1164/rccm.201708-1768OC
Varni, J. W., Limbers, C. A., & Burwinkle, T. M. (2007). Impaired health-related quality of life in children and adolescents with chronic conditions: a comparative analysis of 10 disease clusters and 33 disease categories/severities utilizing the PedsQL 4.0 Generic Core Scales. Health Qual Life Outcomes, 5, 43. https://doi.org/10.1186/1477-7525-5-43
Varni, J. W., Burwinkle, T. M., Seid, M., & Skarr, D. (2003). The PedsQL 4.0 as a pediatric population health measure: Feasibility, reliability, and validity. Ambulatory Pediatrics: The Official Journal of the Ambulatory Pediatrics Association, 3(6), 329–341.
Graham, R. J., Rodday, A. M., & Parsons, S. K. (2014). Family centered assessment and function for children with chronic mechanical respiratory support. Journal of Pediatric Health Care, 28(4), 295–304.
Rodday, A. M., Graham, R. J., Weidner, R. A., Terrin, N., Leslie, L. K., & Parsons, S. K. (2017). Predicting health care utilization for children with respiratory insufficiency using parent-proxy ratings of children’s health-related quality of life. Journal of Pediatric Health Care, 31(6), 654–662. https://doi.org/10.1016/j.pedhc.2017.04.021
Riley, W. T., Rothrock, N., Bruce, B., Christodolou, C., Cook, K., Hahn, E. A., et al. (2010). Patient-reported outcomes measurement information system (PROMIS) domain names and definitions revisions: Further evaluation of content validity in IRT-derived item banks. Quality of Life Research, 19(9), 1311–1321. https://doi.org/10.1007/s11136-010-9694-5
Parsons, S. K., Shih, M. C., Mayer, D. K., Barlow, S. E., Supran, S. E., Levy, S. L., et al. (2005). Preliminary psychometric evaluation of the Child Health Ratings Inventory (CHRIs) and Disease-Specific Impairment Inventory-Hematopoietic Stem Cell Transplantation (DSII-HSCT) in parents and children. Quality of Life Research, 14(6), 1613–1625. https://doi.org/10.1007/s11136-005-1004-2
Sintonen, H. (1994). The 15D-measure of health-related quality of life: Reliability, validity, and sensitivity of its health state descriptive system. National Centre for Health Program Evaluation.
Ravens-Sieberer, U., Gosch, A., Rajmil, L., Erhart, M., Bruil, J., Duer, W., et al. (2005). KIDSCREEN-52 quality-of-life measure for children and adolescents. Expert Review of Pharmacoeconomics & Outcomes Research, 5(3), 353–364. https://doi.org/10.1586/14737167.5.3.353
Ravens-Sieberer, U., & Bullinger, M. (1998). Assessing health-related quality of life in chronically ill children with the German KINDL: First psychometric and content analytical results. Quality of Life Research, 7(5), 399–407. https://doi.org/10.1023/a:1008853819715
Mok, M. M., & Flynn, M. (2002). Establishing longitudinal factorial construct validity of the quality of school life scale for secondary students. Journal of Applied Measurement, 3(4), 400–420.
Acknowledgements
We would like to acknowledge the outstanding work of our additional library scientists including Tisha Mentnech at North Carolina University, Mary McFarland at the University of Utah, Carolyn Biglow at the University of Pittsburgh Medical Center, and Richard James at the University of Pennsylvania and the support of Martha A.Q. Curley, PhD, RN, FAAN at the University of Pennsylvania for the methodological advising and library scientist support. We acknowledge Daniel Notterman, MD (Princeton University); J. Michael Dean, MD (University of Utah); Joseph A Carcillo, MD (UPMC Children’s Hospital of Pittsburgh);Robert A Berg, MD (Children’s Hospital of Philadelphia); Athena Zuppa, MD (Children’s Hospital of Philadelphia); Murray M Pollack, MD (Children’s National Hospital); Kathleen L Meert, MD (Children’s Hospital of Michigan,); Mark W Hall, MD (Nationwide Children’s Hospital); Anil Sapru, MD (Mattel Children’s Hospital, University of California Los Angeles); Patrick S McQuillen, MD (Benioff Children’s Hospital, University of California); Peter M Mourani, MD (Children’s Hospital Colorado, University of Colorado); David Wessel, MD (Children’s National Hospital); Samuel Sorenson, BS (University of Utah); Lenora Olson, PhD (University of Utah) of the PICU-COS Investigators of the Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Network and Tammara L. Jenkins, MSN, RN,PCNS-BC, FCCM (Program Officer, Pediatric Trauma and Critical Illness Branch) and Robert Tamburro, MD, MSc (Medical Officer, Pediatric Trauma and Critical Illness Branch) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Funding
Supported in part by NICHD K23HD096018 (Maddux) and the Francis Family Foundation (Maddux). Additional funding was provided by the Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network. It was approved by the CPCCRN Steering Committee and funded by UG1-HD049983 (Fink) and U01-HD049934 (Dean).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial conflicts of interest to disclose.
Ethical approval
Institutional Review Board approval was not required as the study did not include human subjects.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
11136_2021_2928_MOESM1_ESM.pdf
Supplementary file1—Online Resource 1: Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) POST-PICU Scoping Review Investigators (PDF 116 kb)
11136_2021_2928_MOESM3_ESM.pdf
Supplementary file3—Online Resource 3: Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist (PDF 108 kb)
11136_2021_2928_MOESM4_ESM.pdf
Supplementary file4—Online Resource 4: Identification of eligible health-related quality of life (HRQL) articles (PDF 31 kb)
11136_2021_2928_MOESM5_ESM.pdf
Supplementary file5—Online Resource 5: Characteristics of health-related quality of life articles included, listed by year of publication (PDF 239 kb)
Rights and permissions
About this article
Cite this article
Killien, E.Y., Loftis, L.L., Clark, J.D. et al. Health-related quality of life outcome measures for children surviving critical care: a scoping review. Qual Life Res 30, 3383–3394 (2021). https://doi.org/10.1007/s11136-021-02928-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-021-02928-9