Abstract
Purpose
To describe symptom clusters based on severity of co-occurring symptoms among adults with multiple sclerosis (MS) by age groups and to further examine symptom clusters as a correlate of quality of life (QOL) by age groups.
Methods
This cross-sectional study enrolled persons with MS between 20 and 79 years of age who completed measures of fatigue, depression, anxiety, sleep quality, and QOL using the 36-Item Short Form Health Survey. Bivariate correlation and partial correlation analyses examined associations among symptoms, QOL, and MS characteristics. K-means cluster analyses determined symptom clusters among the full sample and pre-determined age groups (i.e., 20–39, 40–59, and 60–79). One-way ANOVAs examined differences in QOL among clusters for the overall sample and by age groups.
Results
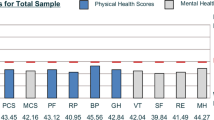
Among the overall sample of 205 participants, symptoms were significantly correlated with QOL and three distinct clusters were identified and differentiated by the magnitude of symptom experience (i.e., mild, moderate, and severe). Results were consistent among young and middle-aged adults; however, among older adults two severe sleep problem clusters were identified that were distinguished by moderate versus severe fatigue, depression, and anxiety. ANOVAs among the overall sample indicated that the three symptom clusters varied significantly for both physical component scores, F(2, 202) = 12.03, p < .001, η2 = .10, and mental component scores, F(2, 202) = 137.92, p < .001, η2 = .58; severe symptom cluster was associated with worse QOL. Patterns in the age subgroup ANOVAs were consistent.
Conclusions
Given the strong association between severity of symptom clusters and QOL, approaches for targeting co-occurring symptoms are critically needed.




Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
N/A.
References
Compston, A., & Coles, A. (2008). Multiple sclerosis. Lancet, 372(9648), 1502–1517. https://doi.org/10.1016/s0140-6736(08)61620-7
Wallin, M. T., Culpepper, W. J., Campbell, J. D., Nelson, L. M., Langer-Gould, A., Marrie, R. A., et al. (2019). The prevalence of MS in the United States: A population-based estimate using health claims data. Neurology, 92(10), e1029–e1040. https://doi.org/10.1212/wnl.0000000000007035
Klaren, R. E., Sebastiao, E., Chiu, C. Y., Kinnett-Hopkins, D., McAuley, E., & Motl, R. W. (2016). Levels and rates of physical activity in older adults with multiple sclerosis. Aging and Disease, 7(3), 278–284. https://doi.org/10.14336/AD.2015.1025
Baird, J. F., Cederberg, K. L., Sikes, E. M., Silveira, S. L., Jeng, B., Sasaki, J. E., et al. (2019). Physical activity and walking performance across the lifespan among adults with multiple sclerosis. Multiple Sclerosis and Related Disorders, 35, 36–41. https://doi.org/10.1016/j.msard.2019.07.003
Baird, J. F., Cederberg, K. L., Sikes, E. M., Jeng, B., Sasaki, J. E., Sandroff, B. M., & Motl, R. W. (2019). Changes in cognitive performance with age in adults with multiple sclerosis. Cognitive and Behavioral Neurology, 32(3), 201–207. https://doi.org/10.1097/WNN.0000000000000200
Bollaert, R. E., & Motl, R. W. (2019). Physical and cognitive functions, physical activity, and sedentary behavior in older adults with multiple sclerosis. Journal of Geriatric Physical Therapy, 42(4), 304–312. https://doi.org/10.1519/JPT.0000000000000163
Krupp, L. (2006). Fatigue is intrinsic to multiple sclerosis (MS) and is the most commonly reported symptom of the disease. Multiple Sclerosis Journal, 12(4), 367–368. https://doi.org/10.1191/135248506ms1373ed
Weiland, T. J., Jelinek, G. A., Marck, C. H., Hadgkiss, E. J., van der Meer, D. M., Pereira, N. G., & Taylor, K. L. (2015). Clinically significant fatigue: Prevalence and associated factors in an international sample of adults with multiple sclerosis recruited via the internet. PLoS One, 10(2), e0115541.
Marrie, R. A., Reingold, S., Cohen, J., Stuve, O., Trojano, M., Sorensen, P. S., et al. (2015). The incidence and prevalence of psychiatric disorders in multiple sclerosis: A systematic review. Multiple Sclerosis Journal, 21(3), 305–317. https://doi.org/10.1177/1352458514564487
Sakkas, G. K., Giannaki, C. D., Karatzaferi, C., & Manconi, M. (2019). Sleep abnormalities in multiple sclerosis. Current Treatment Options in Neurology, 21(1), 4. https://doi.org/10.1007/s11940-019-0544-7
Gray, V., & Arnett, P. (2014). Aging with multiple sclerosis: Cognitive, emotional and neuropathological considerations. Neurodegenerative Disease Management, 4(2), 187–194. https://doi.org/10.2217/nmt.14.12
Kneebone, I. I., Dunmore, E. C., & Evans, E. (2003). Symptoms of depression in older adults with multiple sclerosis (MS): Comparison with a matched sample of younger adults. Aging Mental Health, 7(3), 182–185. https://doi.org/10.1080/1360786031000101148
Jorm, A. F. (2000). Does old age reduce the risk of anxiety and depression? A review of epidemiological studies across the adult life span. Psychological Medicine, 30(1), 11–22. https://doi.org/10.1017/s0033291799001452
Dodd, M. J., Miaskowski, C., & Lee, K. A. (2004). Occurrence of symptom clusters. JNCI Monographs, 2004(32), 76–78.
Barsevick, A. (2016). Defining the symptom cluster: How far have we come? Seminars in Oncology Nursing, 32(4), 334–350. https://doi.org/10.1016/j.soncn.2016.08.001
Motl, R. W., & McAuley, E. (2010). Symptom cluster and quality of life: Preliminary evidence in multiple sclerosis. The Journal of Neuroscience Nursing, 42(4), 212.
Motl, R. W., Suh, Y., & Weikert, M. (2010). Symptom cluster and quality of life in multiple sclerosis. Journal of Pain Symptom Management, 39(6), 1025–1032. https://doi.org/10.1016/j.jpainsymman.2009.11.312
Motl, R. W., Weikert, M., Suh, Y., & Dlugonski, D. (2010). Symptom cluster and physical activity in relapsing-remitting multiple sclerosis. Research in Nursing & Health, 33(5), 398–412.
Newland, P. K., Fearing, A., Riley, M., & Neath, A. (2012). Symptom clusters in women with relapsing-remitting multiple sclerosis. Journal of Neuroscience Nursing, 44(2), 66–71.
Shahrbanian, S., Duquette, P., Kuspinar, A., & Mayo, N. E. (2015). Contribution of symptom clusters to multiple sclerosis consequences. Quality of Life Research, 24(3), 617–629.
Roiland, R. A., & Heidrich, S. M. (2011). Symptom clusters and quality of life in older adult breast cancer survivors. Oncology Nursing Forum, 38(6), 672–680. https://doi.org/10.1188/11.ONF.672-680
Jenkins, J. B., & McCoy, T. P. (2015). Symptom clusters, functional status, and quality of life in older adults with osteoarthritis. Orthopaedic Nursing, 34(1), 36–42. https://doi.org/10.1097/nor.0000000000000112 (quiz 43–34)
Cheung, W. Y., Le, L. W., Gagliese, L., & Zimmermann, C. (2011). Age and gender differences in symptom intensity and symptom clusters among patients with metastatic cancer. Supportive Care in Cancer, 19(3), 417–423. https://doi.org/10.1007/s00520-010-0865-2
Yates, P., Miaskowski, C., Cataldo, J. K., Paul, S. M., Cooper, B. A., Alexander, K., et al. (2015). Differences in composition of symptom clusters between older and younger oncology patients. Journal of Pain Symptom Management, 49(6), 1025–1034. https://doi.org/10.1016/j.jpainsymman.2014.11.296
Krupp, L. B., LaRocca, N. G., Muir-Nash, J., & Steinberg, A. D. (1989). The fatigue severity scale: Application to patients with multiple sclerosis and systemic lupus erythematosus. Archives of Neurology, 46(10), 1121–1123.
Andreasen, A., Stenager, E., & Dalgas, U. (2011). The effect of exercise therapy on fatigue in multiple sclerosis. Multiple Sclerosis Journal, 17(9), 1041–1054.
Learmonth, Y., Dlugonski, D., Pilutti, L., Sandroff, B., Klaren, R., & Motl, R. W. (2013). Psychometric properties of the fatigue severity scale and the modified fatigue impact scale. Journal of Neurolgical Sciences, 331(1–2), 102–107.
Zigmond, A. S., & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), 361–370.
Watson, T. M., Ford, E., Worthington, E., & Lincoln, N. B. (2014). Validation of mood measures for people with multiple sclerosis. International Journal of MS Care, 16(2), 105–109. https://doi.org/10.7224/1537-2073.2013-013
Marrie, R. A., Zhang, L., Lix, L. M., Graff, L. A., Walker, J. R., Fisk, J. D., et al. (2018). The validity and reliability of screening measures for depression and anxiety disorders in multiple sclerosis. Multiple Sclerosis and Related Disorders, 20, 9–15.
Buysse, D. J., Reynolds, C. F., 3rd., Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213.
Carpenter, J. S., & Andrykowski, M. A. (1998). Psychometric evaluation of the Pittsburgh Sleep Quality Index. Journal of Psychosomatic Research, 45(1), 5–13.
Ware, J. E., Jr., & Sherbourne, C. D. (1992). The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Medical Care, 30, 473–483.
Vickrey, B., Hays, R. D., Harooni, R., Myers, L. W., & Ellison, G. W. (1995). A health-related quality of life measure for multiple sclerosis. Quality of Life Research, 4(3), 187–206.
Hohol, M., Orav, E., & Weiner, H. (1995). Disease steps in multiple sclerosis: A simple approach to evaluate disease progression. Neurology, 45(2), 251–255.
Learmonth, Y. C., Motl, R. W., Sandroff, B. M., Pula, J. H., & Cadavid, D. (2013). Validation of patient determined disease steps (PDDS) scale scores in persons with multiple sclerosis. BMC Neurology, 13(1), 37.
Motl, R. W., & McAuley, E. (2009). Symptom cluster as a predictor of physical activity in multiple sclerosis: Preliminary evidence. Journal of Pain Symptom Management, 38(2), 270–280.
Sarstedt, M., & Mooi, E. (2014). Cluster analysis. In B. R. Wainrib (Ed.), A concise guide to market research. The process, data, and methods using IBM SPSS statistics (pp. 274–324). New York: Springer.
Kim, H. J., & Abraham, I. L. (2008). Statistical approaches to modeling symptom clusters in cancer patients. Cancer Nursing, 31(5), E1–E10. https://doi.org/10.1097/01.NCC.0000305757.58615.c8
Barsevick, A. M., Whitmer, K., Nail, L. M., Beck, S. L., & Dudley, W. N. (2006). Symptom cluster research: Conceptual, design, measurement, and analysis issues. Journal of Pain Symptom Management, 31(1), 85–95.
Ghaem, H., & Haghighi, A. B. (2008). The impact of disability, fatigue and sleep quality on the quality of life in multiple sclerosis. Annals of Indian Academy of Neurology, 11(4), 236.
Marrie, R. A., Reider, N., Cohen, J., Trojano, M., Sorensen, P. S., Cutter, G., et al. (2015). A systematic review of the incidence and prevalence of sleep disorders and seizure disorders in multiple sclerosis. Multiple Sclerosis Journal, 21(3), 342–349.
Tabrizi, F. M., & Radfar, M. (2015). Fatigue, sleep quality, and disability in relation to quality of life in multiple sclerosis. International Journal of MS Care, 17(6), 268–274.
Landry, G. J., Best, J. R., & Liu-Ambrose, T. (2015). Measuring sleep quality in older adults: A comparison using subjective and objective methods. Frontiers in Aging Neuroscience, 7, 166.
Espiritu, J. R. D. (2008). Aging-related sleep changes. Clinics in Geriatric Medicine, 24(1), 1–14.
Benedict, R. H., Wahlig, E., Bakshi, R., Fishman, I., Munschauer, F., Zivadinov, R., et al. (2005). Predicting quality of life in multiple sclerosis: Accounting for physical disability, fatigue, cognition, mood disorder, personality, and behavior change. Journal of the Neurological Sciences, 231(1–2), 29–34.
Merlino, G., Fratticci, L., Lenchig, C., Valente, M., Cargnelutti, D., Picello, M., et al. (2009). Prevalence of ‘poor sleep’ among patients with multiple sclerosis: An independent predictor of mental and physical status. Sleep Medicine, 10(1), 26–34.
Fernández, O., Baumstarck-Barrau, K., Simeoni, M.-C., Auquier, P., & MusiQoL study group. (2011). Patient characteristics and determinants of quality of life in an international population with multiple sclerosis: Assessment using the MusiQoL and SF-36 questionnaires. Multiple Sclerosis Journal, 17(10), 1238–1249.
Motl, R. W., McAuley, E., Snook, E. M., & Gliottoni, R. C. (2009). Physical activity and quality of life in multiple sclerosis: Intermediary roles of disability, fatigue, mood, pain, self-efficacy and social support. Psychology, Health & Medicine, 14(1), 111–124.
Motl, R. W., & Sandroff, B. M. (2015). Benefits of exercise training in multiple sclerosis. Current Neurology and Neuroscience Reports, 15(9), 62.
Funding
Funding for this study was provided by the National Multiple Sclerosis Society [CA-1708-29059]. Research reported in this publication was supported, in part, by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health [F32HD101214; F31HD097903] and the National Heart, Lung, and Blood Institute of the National Institutes of Health [T32HL105349]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
RWM and BMS contributed to the study conception and design. All authors lead in material preparation and data collection. SLS lead data analyses with contributions from all authors. The first draft of the manuscript was written by SLS and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by University of Alabama at Birmingham Institutional Review Board and was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
N/A.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Silveira, S.L., Cederberg, K.L.J., Jeng, B. et al. Symptom clusters and quality of life in persons with multiple sclerosis across the lifespan. Qual Life Res 30, 1061–1071 (2021). https://doi.org/10.1007/s11136-020-02689-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-020-02689-x