Abstract
Background
Studies have identified numerous factors that may affect the sleep quality and quality of life (QOL) in outpatients with schizophrenia. However, the clinically stable inpatients who represent a large proportion of the population with schizophrenia in China have not received enough attention. The present study was performed to explore the sociodemographic and clinical correlates of sleep disturbance and QOL in clinically stable inpatients with schizophrenia in rural China.
Methods
A cross-sectional study was designed, and 207 clinically stable inpatients with schizophrenia were selected from Chifeng Anding Hospital, located in Inner Mongolia Autonomous Region, in northern China. All subjects were interviewed by the same investigator using standardized assessment instruments. QOL and sleep disturbance were measured using the Schizophrenia Quality of Life Scale (SQLS) and Pittsburgh Sleep Quality Index (PSQI), respectively. Univariate and multiple regression analyses were used to identify the factors influencing sleep disturbance and QOL. Antipsychotics taken by individuals were converted into olanzapine equivalent doses as the main confounding factor to be controlled.
Results
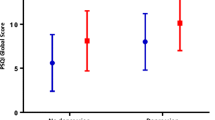
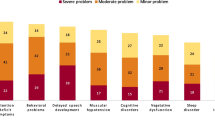
The prevalence of sleep disturbance was 58%, and sleep disturbance was significantly associated with depression (OR 1.33, 95% CI 1.17–1.52) and coping mechanisms (OR 0.95, 95% CI 0.91–0.98). We observed large differences between the sexes: the QOL of male inpatients with schizophrenia was substantially better than that of female inpatients, with a standard coefficient of 0.19 ± 1.62. Other factors related to QOL were depression (0.42 ± 0.30), hope (− 0.21 ± 0.19), general psychopathology symptoms (0.21 ± 0.24) and personal and social performance (− 0.12 ± 0.07).
Conclusions
The depressive symptoms of inpatients with schizophrenia should receive more attention. More targeted interventions, such as the early identification and treatment of depression, should be promptly administered to improve the patient’s hospitalization experience.
Similar content being viewed by others
References
Hofstetter, J. R., Lysaker, P. H., & Mayeda, A. R. (2005). Quality of sleep in patients with schizophrenia is associated with quality of life and coping. BMC Psychiatry, 5(1), 13–13.
Cohrs, S. (2008). Sleep disturbances in patients with schizophrenia. CNS Drugs, 22(11), 939–962.
Bromundt, V., Köster, M., Georgiev-Kill, A., Opwis, K., Wirz-Justice, A., Stoppe, G., et al. (2011). Sleep-wake cycles and cognitive functioning in schizophrenia. British Journal of Psychiatry the Journal of Mental Science, 198(4), 269.
Waters, F., Sinclair, C., Rock, D., Jablensky, A., Foster, R. G., & Wulff, K. (2011). Daily variations in sleep-wake patterns and severity of psychopathology: A pilot study in community-dwelling individuals with chronic schizophrenia. Psychiatry Research, 187(1), 304–306.
Nakamae, T., Kitabayashi, Y., Okamura, A., et al. (2010). Insight and quality of life in long-term hospitalized Japanese patients with chronic schizophrenia. Psychiatry and Clinical Neurosciences, 64(4), 372–376.
Domenech, C., Altamura, C., Bernasconi, C., et al. (2018). Health-related quality of life in outpatients with schizophrenia: Factors that determine changes over time. Social Psychiatry and Psychiatric Epidemiology, 53(3), 239–248.
Nakanishi, M., Setoya, Y., Kodaka, M., et al. (2007). Symptom dimensions and needs of care among patients with schizophrenia in hospital and the community. Psychiatry and Clinical Neurosciences, 61(5), 495–501.
McInerney, S. J., Finnerty, S., Walsh, E., et al. (2018). Quality of life and social functioning of former long-stay psychiatric patients transferred into the community: A 10 year follow up study. Social Psychiatry and Psychiatric Epidemiology, 53(8), 795–801.
Müller, M. J., Olschinski, C., Kundermann, B., & Cabanel, N. (2016). Subjective sleep quality and sleep duration of patients in a psychiatric hospital. Sleep Science, 9(3), 202–206.
Chiu, V. W., Ree, M., Janca, A., & Waters, F. (2016). Sleep in schizophrenia: Exploring subjective experiences of sleep problems, and implications for treatment. Psychiatric Quarterly, 87(4), 633–648.
Tang, Y. L., Sevigny, R., Mao, P. X., Jiang, F., & Cai, Z. (2007). Help-seeking behaviors of chinese patients with schizophrenia admitted to a psychiatric hospital. Administration & Policy in Mental Health & Mental Health Services Research, 34(2), 101–107.
Krystal, A. D., Goforth, H. W., & Roth, T. (2008). Effects of antipsychotic medications on sleep in schizophrenia. International Clinical Psychopharmacology, 23(3), 150–160.
Afonso, P., Brissos, S., Cañas, F., Bobes, J., & Bernardo-Fernandez, I. (2014). Treatment adherence and quality of sleep in schizophrenia outpatients. International Journal of Psychiatry in Clinical Practice, 18(1), 70–76.
Kilicaslan, E. E., Esen, A. T., Kasal, M. I., Ozelci, E., Boysan, M., & Gulec, M. (2017). Childhood trauma, depression, and sleep quality and their association with psychotic symptoms and suicidality in schizophrenia. Psychiatry Research, 258, 557.
Ma, X. R., Song, G. R., Xu, X. B., Tian, T., & Chang, S. H. (2018). The prevalence of sleep disturbance and its socio-demographic and clinical correlates in first-episode individuals with schizophrenia in rural China. Perspective Psychiatric Care, 54, 31.
Gong, W., Xu, D., Zhou, L., Shelton, B. I. H., Smith, K. L., & Xiao, S. (2014). Village doctor-assisted case management of rural patients with schizophrenia: Protocol for a cluster randomized control trial. Implementation Science, 9(1), 13–13.
Alessandrini, M., Lançon, C., Fond, G., Faget-Agius, C., Richieri, R., Faugere, M., et al. (2016). A structural equation modelling approach to explore the determinants of quality of life in schizophrenia. Schizophrenia Research, 171(1–3), 27–34.
Ritsner, M., Kurs, R., Ponizovsky, A., & Hadjez, J. (2004). Perceived quality of life in schizophrenia: Relationships to sleep quality. Quality of Life Research, 13(4), 783–791.
Zhang, Q., Li, X., Parker, G. J., Hong, X. H., Wang, Y., Lui, S. S., et al. (2016). Theory of mind correlates with clinical insight but not cognitive insight in patients with schizophrenia. Psychiatry Research, 237, 188–195.
Lobana, A., Mattoo, S. K., Basu, D., & Gupta, N. (2010). Quality of life in schizophrenia in India: Comparison of three approaches. Acta Psychiatrica Scandinavica, 104(1), 51–55.
Leucht, S., Samara, M., Heres, S., & Davis, J. M. (2016). Dose equivalents for antipsychotic drugs: The DDD method. Schizophrenia Bulletin, 42(suppl 1), S90.
Buysse, D. J., Rd, R. C., Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213.
Kay, S. R., Opler, L. A., & Lindenmayer, J. P. (1988). Reliability and validity of the positive and negative syndrome scale for schizophrenics. Psychiatry Research, 23(1), 99–110.
Tianmei, S. I., Yang, J., & Liang, S. (2004). The reliability, validity of PANSS and its implication. Chinese Mental Health Journal, 18(1), 45–47.
Wilkinson, G., Hesdon, B., Wild, D., Cookson, R., Farina, C., Sharma, V., et al. (2000). Self-report quality of life measure for people with schizophrenia: The SQLS. British Journal of Psychiatry, 177(177), 42–46.
Luo, H., Nan, L., & Wang, Y. Q. (2003). Reliability and validity of the schizophrenia quality of life scale. Chinese Mental Health Journal, 17, 172–174.
Choe, K. (2014). Development and preliminary testing of the Schizophrenia Hope Scale, a brief scale to measure hope in people with schizophrenia. International Journal of Nursing Studies, 51(6), 927–933.
Morosini, P. L., Magliano, L., Brambilla, L., Ugolini, S., & Pioli, R. (2000). Development, reliability and acceptability of a new version of the DSM-IV social and occupational functioning assessment scale (SOFAS) to assess routine social functioning. Acta Psychiatrica Scandinavica, 101(4), 323–329.
Si, T. M., Shu, L., Tian, C. H., Ya, S. U., Yan, J., Cheng, J. L., et al. (2009). Evaluation of reliability and validity of the Chinese version of personal and social performance scale in patients with schizophrenia. Chinese Mental Health Journal, 23, 790–794.
Addington, D., Addington, J., & Schissel, B. (1990). A depression rating scale for schizophrenics. Schizophrenia Research, 3(4), 247–251.
Zhou, P., Liu, L. Y., Zhang, B., & Jia, F. J. (2009). Reliability and validity of the Chinese version of calgary depression scale for schizophrenia. Chinese Mental Health Journal., 23, 638–642.
Connor, K. M., & Davidson, J. R. T. (2010). Development of a new resilience scale: The Connor–Davidson Resilience Scale (CD-RISC). Depression & Anxiety, 18(2), 76–82.
Rosenberg, M. (1965). Self esteem and the adolescent. Economics and the social sciences: Society and the adolescent self-image. Science, 148, 177–196.
Xie, Y. N. (1999). Simplified coping style questionnaire. Chinese Mental Health Journal, 13(Suppl), 122–124.
Michael, H., Neter, J., & Nachtsheim, C. J. (2004). Applied linear statistical models (5th ed., pp. 407–410). New York: McGraw-Hill Higher Education.
Ohayon, M. M. (2007). Prevalence and comorbidity of sleep disorders in general population. La Revue Du Praticien, 57(14), 1521.
Lijun, C., Ke-Qing, L., Xiuli, S., Ze, C., Qinpu, J., Yanchao, H., et al. (2012). A survey of sleep quality in patients with 13 types of mental disorders. Primary Care Companion for Cns Disorders. https://doi.org/10.4088/PCC.11m01173.
Wesselius, H. M., van den Ende, E. S., Alsma, J., et al. (2018). Quality and quantity of sleep and factors associated with sleep disturbance in hospitalized patients. JAMA Internal Medicine, 178(9), 1201–1208.
Fekih-Romdhane, F., Jendoubi, J., Saguem, B. N., Ridha, R., & Cheour, M. (2019). The link between sleep disturbances and suicidal thoughts and behaviors in remitted bipolar I patients. Journal of Clinical Psychology, 75(9), 1643–1657.
Hartwig, E. M., Rufino, K. A., Palmer, C. A., et al. (2019). Trajectories of self-reported sleep disturbance across inpatient psychiatric treatment predict clinical outcome in comorbid major depressive disorder and generalized anxiety disorder. Journal of Affective Disorders, 251, 248–255.
Oles, S. K., Fukui, S., Rand, K. L., & Salyers, M. P. (2015). The relationship between hope and patient activation in consumers with schizophrenia: Results from longitudinal analyses. Psychiatry Research, 228(3), 272–276.
Xiao, W., Liu, H., Zhang, H., Liu, Q., Fu, P., Chen, J., et al. (2009). Reliability and validity of the Chinese version of the calgary depression scale for schizophrenia. Australian & New Zealand Journal of Psychiatry, 43(6), 548.
Xu, Y. M., Li, F., Liu, X. B., & Zhong, B. L. (2018). Depressive symptoms in Chinese male inpatients with schizophrenia: Prevalence and clinical correlates. Psychiatry Research, 264, 380–384.
Upthegrove, R., Marwaha, S., & Birchwood, M. (2017). Depression and schizophrenia: Cause, consequence, or trans-diagnostic issue? Schizophrenia Bulletin, 43(2), 240–244.
Verma, D., Srivastava, M. K., Singh, S. K., Bhatia, T., & Deshpande, S. N. (2016). Lifetime suicide intent, executive function and insight in schizophrenia and schizoaffective disorders. Schizophrenia Research, 178(1–3), 12.
Lysaker, P. H., Pattison, M. L., Leonhardt, B. L., Phelps, S., & Vohs, J. L. (2018). Insight in schizophrenia spectrum disorders: Relationship with behavior, mood and perceived quality of life, underlying causes and emerging treatments. World Psychiatry, 17(1), 12–23.
Marksteiner, J., Adlassnig, C., Weiss, E. M., Gasser, M., & Aichhorn, W. (2005). Gender differences in pharmacokinetics and side effects of second generation antipsychotic drugs. Current Neuropharmacology, 3(1), 73.
Xiang, Y. T., Weng, Y. Z., Leung, C. M., Tang, W. K., Chan, S. S., Wang, C. Y., et al. (2010). Gender differences in sociodemographic and clinical characteristic and the quality of life of Chinese schizophrenia patients. Australian and New Zealand Journal of Psychiatry, 44(5), 450–455.
Brissos, S., Balanza-Martinez, V., Dias, V. V., Carita, A. I., & Figueira, M. L. (2011). Is personal and social functioning associated with subjective quality of life in schizophrenia patients living in the community? European Archives of Psychiatry and Clinical Neuroscience, 261(7), 509–517.
Vrbova, K., Prasko, J., Ociskova, M., Kamaradova, D., Marackova, M., Holubova, M., et al. (2017). Quality of life, self-stigma, and hope in schizophrenia spectrum disorders: A cross-sectional study. Neuropsychiatric Disease & Treatment, 13, 567–576.
Sumskis, S., Moxham, L., & Caputi, P. (2017). Meaning of resilience as described by people with schizophrenia. International Journal of Mental Health Nursing, 26(3), 273–284.
Wartelsteiner, F., Mizuno, Y., Frajoapor, B., Kemmler, G., Pardeller, S., Sondermann, C., et al. (2016). Quality of life in stabilized patients with schizophrenia is mainly associated with resilience and self-esteem. Acta Psychiatrica Scandinavica, 134(4), 360–367.
Arbinaga, F. (2018). Self-reported perceptions of sleep quality and resilience among dance students. Perceptual and Motor Skills, 15(2), 351–368.
Opel, N., Redlich, R., Dohm, K., Zaremba, D., Goltermann, J., Repple, J., et al. (2019). Mediation of the influence of childhood maltreatment on depression relapse by cortical structure: A 2-year longitudinal observational study. Lancet Psychiatry, 6(4), 318–326.
Wulff, K., Dijk, D. J., Middleton, B., Foster, R. G., & Joyce, E. M. (2012). Sleep and circadian rhythm disruption in schizophrenia. British Journal of Psychiatry, 200(4), 308–316.
Acknowledgements
We thank all the individuals who participated in the project and the staff who were involved in the recruitment of participants.
Funding
This study was supported by a grant from the National Natural Science Foundation of China (Grant Number: 71673070). The sponsor had no role in the study design, writing of the manuscript, or decision to submit this or future manuscripts for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare in relation to the subject of this study.
Ethical approval
This study was approved by the Medical Ethics Committee of Harbin Medical University (Daqing).
Informed consent
Informed consent was obtained from all individual participants (or their legal representative) prior to inclusion in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, WL., Zhou, YQ., Chai, NN. et al. Sleep disturbance and quality of life in clinically stable inpatients with schizophrenia in rural China. Qual Life Res 29, 2759–2768 (2020). https://doi.org/10.1007/s11136-020-02541-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-020-02541-2