Abstract
Objective
To collect and assess the extant empirical literature assessing disease-specific health-related quality of life (HRQOL) in pediatric transplant recipients using the PedsQL 3.0 Transplant Module (PedsQL-TM) assessment.
Study design
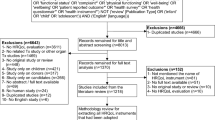
A systematic search and review procedure was conducted of research reporting use and results of the PedsQL-TM with samples of pediatric heart, liver, kidney, and lung transplantation. Searches were conducted in nine scholarly databases and two additional sources to identify unpublished research. Multiple reviewers screened studies meeting inclusion criteria in accordance with PRISMA guidelines.
Results
A final sample of nine studies reported findings for the PedsQL-TM with pediatric organ transplant recipients. Most studies relied on either kidney or liver transplant recipients from single pediatric transplant centers. Factor validity of the PedsQL-TM and inter-rater reliability (IRR) between patients and parents have not been adequately determined. Internal consistency reliability was found as acceptable or excellent across multiple studies. PedsQL-TM scores were found to vary with other HRQOL issues, yet few studies examined their association with medication adherence or posttransplant health outcomes.
Conclusions
With the goal of enhancing and sustaining HRQOL in pediatric organ transplant recipients, the need for a psychometrically valid and reliable measure of transplant-specific HRQOL is apparent. Research on the PedsQL-TM supports the promise of this measure although future efforts should be taken to examine measurement issues such as factor validity and IRR. Assessing transplant-specific HRQOL in these patients is paramount for their care and appropriate decision-making by patients, families, and the transplant team.

Similar content being viewed by others
Abbreviations
- HRQOL:
-
Health-related quality of life
- PedsQL-TM:
-
PedsQL 3.0 Transplant Module
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- ICC:
-
Intraclass correlations
- IRR:
-
Inter-rater reliability
References
Fredericks, E. M., et al. (2014). Post-transplant adjustment—The later years. Pediatric Transplantation,18(7), 675–688.
Parmar, A., Vandriel, S. M., & Ng, V. L. (2017). Health-related quality of life after pediatric liver transplantation: A systematic review. Liver Transplantation,23(3), 361–374.
Hart, A., et al. (2019). OPTN/SRTR 2017 annual data report: Kidney. American Journal of Transplantation,19, 19–123.
Kim, W., et al. (2019). OPTN/SRTR 2017 annual data report: Liver. American Journal of Transplantation,19, 184–283.
Colvin, M., et al. (2019). OPTN/SRTR 2017 annual data report: Heart. American Journal of Transplantation,19, 323–403.
Valapour, M., et al. (2019). OPTN/SRTR 2017 annual data report: Lung. American Journal of Transplantation,19, 404–484.
WH Organization. Constitution of the world health organization. 1995.
Varni, J. W., Seid, M., & Kurtin, P. S. (1999). Pediatric health-related quality of life measurement technology: A guide for health care decision makers. JCOM-WAYNE PA-,6, 33–44.
Qvist, E., Jalanko, H., & Holmberg, C. (2003). Psychosocial adaptation after solid organ transplantation in children. Pediatric Clinics of North America,50, 1505–1519.
Varni, J. W., Seid, M., & Kurtin, P. S. (2001). PedsQL™ 4.0: Reliability and validity of the pediatric quality of Life Inventory™ Version 4.0 generic core scales in healthy and patient populations. Medical Care,39, 800–812.
HealthActCHQ. (2008). Child Health Questionnaire Scoring and Interpretation Manual. Cambridge, MA: HealthActCHQ Inc.
Annunziato, R. A., et al. (2014). Strategies for measuring quality of life among pediatric solid-organ transplant recipients. Prog Transplant,24(3), 247–256.
Ng, V., et al. (2014). Development and validation of the pediatric liver transplantation quality of life: A disease-specific quality of life measure for pediatric liver transplant recipients. Journal of Pediatrics,165, 547.e7–555.e7.
Weissberg-Benchell, J., et al. (2010). Pediatric health-related quality of life: Feasibility, reliability and validity of the PedsQL™ transplant module. American Journal of Transplantation,10(7), 1677–1685.
Varni, J. W., et al. (2003). The PedsQL 4.0 as a pediatric population health measure: Feasibility, reliability, and validity. Ambulatory Pediatrics,3, 329–341.
Varni, J. W., et al. (2002). The PedsQL™ in pediatric cancer: Reliability and validity of the pediatric quality of life inventory™ generic core scales, multidimensional fatigue scale, and cancer module. Cancer,94(7), 2090–2106.
Varni, J. W., et al. (2004). The PedsQL™ in pediatric asthma: Reliability and validity of the Pediatric Quality of Life Inventory™ generic core scales and asthma module. Journal of Behavioral Medicine,27(3), 297–318.
Varni, J. W., Thompson, K. L., & Hanson, V. (1987). The Varni/thompson pediatrie pain questionnaire. I. Chronic musculoskeletal pain in juvenile rheumatoid arthritis. Pain,28(1), 27–38.
Varni, J., et al. (2019). Pediatric Quality of Life Inventory (Peds QL) 3.2 Diabetes Module for youth with Type 2 diabetes: Reliability and validity. Diabetic Medicine,36(4), 465–472.
Varni, J. W., et al. (2018). PedsQL 3.2 Diabetes Module for children, adolescents, and young adults: Reliability and validity in type 1 diabetes. Diabetes Care,41(10), 2064–2071.
Moher, D., et al. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLOS Medicine,6(7), e1000097.
Covidence systematic review software, Veritas Health Innovation, Melbourne. www.covidence.org.
Downs, S. H., & Black, N. (1998). The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. Journal of Epidemiology and Community Health,52(6), 377–384.
Dew, M. A., et al. (2009). Meta-analysis of medical regimen adherence outcomes in pediatric solid organ transplantation. Transplantation,88(5), 736–746.
Killian, M. O., et al. (2018). Psychosocial predictors of medication non-adherence in pediatric organ transplantation: A systematic review. Pediatric Transplantation,22(4), e13188.
Taybeh, E. O. (2016). Medicines use in children: Adherence and beyond. Ann Arbor: Queen’s University Belfast.
Splinter, K., et al. (2016). Impaired health-related quality of life in children and families affected by methylmalonic acidemia. Journal of Genetic Counseling,25(5), 936–944.
Kikuchi, R., et al. (2017). Development of the Japanese version of the Pediatric Quality of Life Inventory™ transplant module. Pediatrics International,59(1), 80–88.
Kikuchi, R., et al. (2018). Quality of life after living donor liver transplant for biliary atresia in Japan. Pediatrics International,60(2), 183–190.
Bamford, J., & Wirz, L. (2016). Piloting psychology annual reviews as a method of measuring psychological distress and quality of life in paediatric renal transplant patients. BioMed Research International. https://doi.org/10.1155/2016/1685362.
He, K., et al. (2015). Health-related quality of life and sleep among Chinese children after living donor liver transplantation. Pediatric Transplantation,19(5), 547–554.
Denny, B., et al. (2012). New insights into family functioning and quality of life after pediatric liver transplantation. Pediatric Transplantation,7, 711.
Osborne, J. W., Costello, A. B., & Kellow, J. T. (2008). Best practices in exploratory factor analysis. Best practices in quantitative methods (pp. 86–99). Los Angeles: Sage.
Cicchetti, D. V. (1994). Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychological Assessment,6(4), 284.
Varni, J. W., et al. (2002). The PedsQLTM 4.0 Generic Core Scales: Sensitivity, responsiveness, and impact on Clinical decision-making. Journal of Behavioral Medicine,25, 175–193.
Manworren, R. C., & Stinson, J. (2016). Pediatric pain measurement, assessment, and evaluation. Semin Pediatr Neurol,23, 189–200.
Eiser, C., & Varni, J. W. (2013). Health-related quality of life and symptom reporting: Similarities and differences between children and their parents. European Journal of Pediatrics,172(10), 1299–1304.
Haverman, L., et al. (2017). Paediatric health-related quality of life: What is it and why should we measure it? Archives of Disease in Childhood,102(5), 393–400.
Wolf, E. J., et al. (2013). Sample size requirements for structural equation models: An evaluation of power, bias, and solution propriety. Educ Psychol Meas,73(6), 913–934.
Sarwal, M. M., & Bagga, A. (2013). Quality of life after organ transplantation in children. Current Opinion in Organ Transplant,18(5), 563–568.
Devine, K. A., et al. (2011). Predictors of long-term health-related quality of life in adolescent solid organ transplant recipients. Journal of Pediatric Psychology,36(8), 891–901.
Alonso, E. M., et al. (2013). Factors predicting health-related quality of life in pediatric liver transplant recipients in the functional outcomes group. Pediatric Transplantation,17(7), 605–611.
Fredericks, E. M. (2012). Family roles and routines after pediatric liver transplantation: Implications for quality of life and beyond. Pediatric Transplantation,16(7), 688.
Fredericks, E. M., et al. (2007). Psychological functioning, nonadherence and health outcomes after pediatric liver transplantation. American Journal of Transplantation,7(8), 1974–1983.
Bunzel, B., & Laederach-Hofmann, K. (2000). Solid organ transplantation: Are there predictors for posttransplant non-compliance? A literature overview. Transplantation,70, 711–716.
Laederach-Hofmann, K., & Bunzel, B. (2000). Noncompliance in organ transplant recipients: A literature review. General Hospital Psychiatry,22(6), 412–424.
Mohammad, S., et al. (2012). Health status in young adults two decades after pediatric liver transplantation. American Journal of Transplantation,12(6), 1486–1495.
Funding
No funding supported this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors. No informed procedures were necessary or included this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Killian, M.O., Triplett, K.N., Masood, S.S. et al. Measurement of health-related quality of life in pediatric organ transplantation recipients: a systematic review of the PedsQL transplant module. Qual Life Res 29, 1137–1146 (2020). https://doi.org/10.1007/s11136-019-02398-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-019-02398-0