Abstract
Purpose
End-stage renal disease patients’ experience of care is an integral part of the assessment of the quality of the care provided at hemodialysis centers and is needed to promote patient choice, quality improvement, and accountability. The purpose of this study is to evaluate the In-Center Hemodialysis Consumer Assessment of Healthcare Providers and Systems (ICH-CAHPS®) survey and its equivalence in different age, gender, race, and education subgroups.
Methods
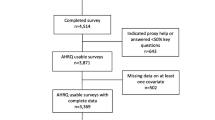
The ICH-CAHPS survey was administered to 1454 patients from 32 dialysis facilities. For the characteristics compared, the sample had 756 participants younger than 65 years old, 739 men, 516 Black, 567 White, and 970 with less than high school diploma. Three different patient experience constructs were studied including nephrologist’s communication and caring, quality of care and operations, and providing information to patients. We used item response theory analysis to examine the possibility of differential item functioning (DIF) by patient age, gender, race, and education separately after controlling for the other DIF characteristics and additional confounding variables including survey mode, mental, and general health status as well as duration on dialysis.
Results
The three constructs studied were unidimensional and no major DIF was observed on the composites. Some non-equivalences were observed when confounders were not controlled for, suggesting that such covariates can be important factors in understanding the possibility of disparity in patients’ experience.
Conclusions
The ICH-CAHPS is a promising survey to elicit hemodialysis patients’ experience that has good psychometric properties and provides a standardized tool for assessing age, gender, race, or education disparity.




Similar content being viewed by others
References
(USRDS), U. S. R. D. S. (2017). 2017 USRDS annual data report: Epidemiology of kidney disease in the United States. http://www.usrds.org. Accessed October 18, 2018.
Saran, R., Robinson, B., Abbott, K. C., Agodoa, L. Y. C., Bragg-Gresham, J., Balkrishnan, R., et al. (2018). US Renal Data System 2017 annual data report epidemiology of kidney disease in the United States. American Journal of Kidney Diseases, 71(3), S1–S676. https://doi.org/10.1053/j.ajkd.2018.01.002.
Couchoud, C., Kooman, J., Finne, P., Leivestad, T., Stojceva-Taneva, O., Ponikvar, J. B., et al. (2009). From registry data collection to international comparisons: Examples of haemodialysis duration and frequency. Nephrology, Dialysis, Transplantation, 24(1), 217–224. https://doi.org/10.1093/ndt/gfn442.
Kjellstrand, C. M. (1988). Age, sex, and race inequality in renal-transplantation. Archives of Internal Medicine, 148(6), 1305–1309.
Rosansky, S. J. (2012). The sad truth about early initiation of dialysis in elderly patients. Jama-Journal of the American Medical Association, 307(18), 1919–1920. https://doi.org/10.1001/jama.2012.3522.
Thorsteinsdottir, B., Swetz, K. M., Feely, M. A., Mueller, P. S., & Williams, A. W. (2012). Are there alternatives to hemodialysis for the elderly patient with end-stage renal failure? Mayo Clinic Proceedings, 87(6), 514–516. https://doi.org/10.1016/j.mayocp.2012.02.016.
Adler, N. E., Boyce, W. T., Chesney, M. A., Folkman, S., & Syme, S. L. (1993). Socioeconomic inequalities in health. No easy solution. Journal of the American Medical Association, 269, 3140–3145.
Nelson, E. C., Hays, R. D., Arnold, S., Kwoh, K., & Sherbourne, C. (1989). Age and functional health status. Santa Monica, CA: The RAND Corporation.
Khattak, M., Sandhu, G. S., Desilva, R., & Goldfarb-Rumyantzev, A. S. (2012). Association of education level with dialysis outcome. Hemodialysis International, 16(1), 82–88. https://doi.org/10.1111/j.1542-4758.2011.00615.x.
Peipert, J. D., Bentler, P., Klicko, K., & Hays, R. D. (2018). Negligible impact of differential item functioning between Black and White dialysis patients on the Kidney Disease Quality of Life 36-item short form survey (KDQOL((TM))-36). Quality of Life Research, 27(10), 2699–2707. https://doi.org/10.1007/s11136-018-1879-3.
Salisbury, C. (2009). Using patient experience within pay for performance programmes. Bmj-British Medical Journal. https://doi.org/10.1136/bmj.b4224.
Al-Abri, R., & Al-Balushi, A. (2014). Patient satisfaction survey as a tool towards quality improvement. Oman Medical Journal, 29(1), 3–7. https://doi.org/10.5001/omj.2014.02.
Gleeson, H., Calderon, A., Swami, V., Deighton, J., Wolpert, M., & Edbrooke-Childs, J. (2016). Systematic review of approaches to using patient experience data for quality improvement in healthcare settings. BMJ Open. https://doi.org/10.1136/bmjopen-2016-011907.
Weidmer, B. A., Cleary, P. D., Keller, S., Evensen, C., Hurtado, M. P., Kosiak, B., et al. (2014). Development and evaluation of the CAHPS (Consumer Assessment of Healthcare Providers and Systems) survey for in-center hemodialysis patients. American Journal of Kidney Diseases, 64(5), 753–760. https://doi.org/10.1053/j.ajkd.2014.04.021.
Setodji, C. M., Reise, S. P., Morales, L. S., Fongwa, M. N., & Hays, R. D. (2011). Differential item functioning by survey language among older hispanics enrolled in medicare managed care a new method for anchor item selection. Medical Care, 49(5), 461–468. https://doi.org/10.1097/MLR.0b013e318207edb5.
Rosenbaum, P. R., & Rubin, D. B. (1983). The central role of the propensity score in observational studies for causal effects. Biometrika, 70(1), 41–55. https://doi.org/10.1093/biomet/70.1.41.
Wang, Y., Cai, H., Li, C., Jiang, Z., Wang, L., Song, J., et al. (2013). Optimal caliper width for propensity score matching of three treatment groups: A Monte Carlo study. PLoS ONE, 8(12), e81045. https://doi.org/10.1371/journal.pone.0081045.
Collins, L. M., Schafer, J. L., & Kam, C.-M. (2001). A comparison of inclusive and restrictive strategies in modern missing data procedures. Psychological Methods, 6(4), 330–351. https://doi.org/10.1037/1082-989X.6.4.330.
Reise, S. P., Cook, K. F., & Moore, T. M. (2015). Evaluating the impact of multidimensionality on unidimensional item response theory model parameters. In S. P. Reise & D. A. Revicki (Eds.), Multivariate applications series. Handbook of item response theory modeling: Applications to typical performance assessment. Taylor & Francis Group: New York, NY.
Hu, L. T., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling-A Multidisciplinary Journal, 6(1), 1–55. https://doi.org/10.1080/10705519909540118.
Samejima, F. (1996). Evaluation of mathematical models for ordered polychrotomous responses. Behaviormetrika, 23, 17–35. https://doi.org/10.2333/bhmk.23.17.
Wang, M., & Woods, C. M. (2017). Anchor selection using the wald test anchor-all-test-all procedure. Applied Psychological Measurement, 41(1), 17–29. https://doi.org/10.1177/0146621616668014.
Woods, C. M., Cai, L., & Wang, M. A. (2013). The langer-improved wald test for DIF testing with multiple groups: Evaluation and comparison to two-group IRT. Educational and Psychological Measurement, 73(3), 532–547. https://doi.org/10.1177/0013164412464875.
Kim, J., & Oshima, T. C. (2013). Effect of multiple testing adjustment in differential item functioning detection. Educational and Psychological Measurement, 73(3), 458–470. https://doi.org/10.1177/0013164412467033.
Benjamini, Y., & Hochberg, Y. (1995). Controlling the false discovery rate—A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society Series B-Methodological, 57(1), 289–300.
Teresi, J. A., Kleinman, M., & Ocepek-Welikson, K. (2000). Modern psychometric methods for detection of differential item functioning: Application to cognitive assessment measures. Statistics in Medicine, 19(11–12), 1651–1683. https://doi.org/10.1002/(SICI)1097-0258(20000615/30)19:11/12%3c1651:AID-SIM453%3e3.0.CO;2-H.
Raju, N. S., van der Linden, W. J., & Fleer, P. F. (1995). IRT-based internal measures of differential functioning of items and tests. Applied Psychological Measurement, 19, 353–368.
Flowers, C. P., Oshima, T. C., & Raju, N. S. (1999). A description and demonstration of the polytomous-DFIT framework. Applied Psychological Measurement, 23(4), 309–326. https://doi.org/10.1177/01466219922031437.
Raju, N. S. (1999). DFITP5: A Fortran program for calculating dichotomous DIF/DTF. Chicago: Illinois Institute of Technology.
Muthén, L., & Muthén, B. (2001). Mplus User’s Guide. CA: Los Angeles.
Cai, L. (2012). Vector Psychometric Group. WA: Seattle.
Wood, R., Paoli, C. J., Hays, R. D., Taylor-Stokes, G., Piercy, J., & Gitlin, M. (2014). Evaluation of the consumer assessment of healthcare providers and systems in-center hemodialysis survey. Clinical Journal of the American Society of Nephrology, 9(6), 1099–1108. https://doi.org/10.2215/Cjn.10121013.
Kjellstrand, C. (1997). All elderly patients should be offered dialysis. Geriatric Nephrology and Urology, 6, 129–136. https://doi.org/10.1007/BF00249628.
Avorn, J. (1984). Benefit and cost analysis in geriatric care. Turning age discrimination into health policy. New England Journal of Medicine, 310(20), 1294–1301. https://doi.org/10.1056/nejm198405173102005.
Veerappan, I., Arvind, R. M., & Ilayabharthi, V. (2012). Predictors of quality of life of hemodialysis patients in India. Indian Journal of Nephrology, 22(1), 18–25. https://doi.org/10.4103/0971-4065.91185.
Peipert, J. D., Bentler, P. M., Klicko, K., & Hays, R. D. (2018). Psychometric properties of the kidney disease quality of life 36-item short-form survey (KDQOL-36) in the United States. American Journal of Kidney Diseases, 71(4), 461–468. https://doi.org/10.1053/j.ajkd.2017.07.020.
Groves, R., Floyd, J., & Fowler, J. M. (2013). Survey methodology. Hoboken: Wiley.
Halbesleben, J. R. B., & Whitman, M. V. (2013). Evaluating survey quality in health services research: A decision framework for assessing nonresponse bias. Health Services Research, 48(3), 913–930. https://doi.org/10.1111/1475-6773.12002.
Richardson, M. M., & Grobert, M. E. (2014). ICH-CAHPS: What signal on the chadburn? American Journal of Kidney Diseases, 64(5), 670–672. https://doi.org/10.1053/j.ajkd.2014.09.002.
Peipert, J. D., & Hays, R. D. (2017). Methodological considerations in using patient reported measures in dialysis clinics. Journal of Patient-Reported Outcomes, 1(1), 11. https://doi.org/10.1186/s41687-017-0010-9.
Funding
This research was supported through cooperative agreements from the Agency for Healthcare Research and Quality: U18 HS016980 and U18 HS016978.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have conflicts of interest or any financial relationships relevant to this article to disclose.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Ethical approval
All data collection were approved by the RAND institutional review boards (FWA00003425, effective until June 22, 2023). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Setodji, C.M., Peipert, J.D. & Hays, R.D. Differential item functioning of the CAHPS® In-Center Hemodialysis Survey. Qual Life Res 28, 3117–3135 (2019). https://doi.org/10.1007/s11136-019-02250-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-019-02250-5