Abstract
Purpose
The aim of the present study was to evaluate the influence of emotional problems on health-related quality of life (HRQoL) according to the type of emotional problem, degree of limitation, and perceived control of the problem with treatment.
Method
A population-based cross-sectional study with probabilistic stratified cluster sampling was conducted in 2014 and 2015 in the city of Campinas, Brazil. A total of 2145 individuals aged 18 years or older participated in the study. HRQoL was evaluated using the SF-36® questionnaire. The dependent variables were the score of the eight scales of the SF-36®. The independent variables were self-perceived emotional problems, type of emotional problem (according to ICD 10), degree of limitation, and perceived control of the problem with treatment. Mean scores were calculated and regression coefficients were adjusted for sex, age, number of health problems, and chronic diseases using multiple linear regression analysis.
Results
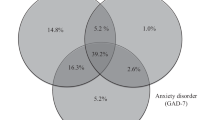
The prevalence of emotional problems was 32.7%. Among the individuals with a problem, the mean SF-36® scores were lower on all domains. Regarding the type of emotional problem, a complaint of depression exerted a stronger negative impact on HRQoL scores than anxiety. Moreover, a greater degree of limitation caused by the problem led to lower mean SF-36® scores. The negative impact on HRQoL was substantially greater among those who did not have the problem under control.
Conclusion
In conclusion, the findings underscore the importance of the prevention and control of emotional problems with the aim of reducing the impact on HRQoL.
Similar content being viewed by others
References
Vos, T., Abajobir, A. A., Abate, K. H., et al. (2017). Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. The Lancet, 390, 1211–1259.
Bloom, D. E, Cafiero, E. T., Jané-Llopis, E. et al. (2011). The global economic burden of non-communicable diseases.
World Bank Group, World Health Organization. (2016). Out of the shadows: Making mental health a global development priority. Retrieved from http://www.who.int/mental_health/advocacy/WB_event_2016/en/
Askari, M. S., Andrade, L. H., Filho, A. C., et al. (2017). Dual burden of chronic physical diseases and anxiety/mood disorders among São Paulo Megacity Mental Health Survey Sample, Brazil. Journal of Affective Disorders, 220, 1–7.
Prigent, A., Kamendje-Tchokobou, B., & Chevreul, K. (2017). Socio-demographic, clinical characteristics and utilization of mental health care services associated with SF-6D utility scores in patients with mental disorders: Contributions of the quantile regression. Quality of Life Research. https://doi.org/10.1007/s11136-017-1623-4.
Assunção, A. Á., de Lima, E., Guimarães, M. D. C., et al. (2017). Transtornos mentais e inserção no mercado de trabalho no Brasil: um estudo multicêntrico nacional. Cad Saude Publica, 33, e00166815.
Seidl, E. M. F., & da Zannon, C. M. L. (2004). Qualidade de vida e saúde: aspectos conceituais e metodológicos. Cad Saude Publica, 20, 580–588.
da Lima, A. F. B., & de Fleck, M. P. (2011). Quality of life, diagnosis, and treatment of patients with major depression: A prospective cohort study in primary care. Revista Brasileira de Psiquiatria, 33, 245–251.
Gallegos-Carrillo, K., García-Peña, C., Mudgal, J., et al. (2009). Role of depressive symptoms and comorbid chronic disease on health-related quality of life among community-dwelling older adults. Journal of Psychosomatic Research, 66, 127–135.
Schwab, B., Daniel, H. S., Lutkemeyer, C., et al. (2015). Variables associated with health-related quality of life in a Brazilian sample of patients from a tertiary outpatient clinic for depression and anxiety disorders. Trends in Psychiatry and Psychotherapy, 37, 202–208.
Zeng, Q., Xu, Y., & Chun Wang, W. (2013). Quality of life in outpatients with depression in China. Journal of Affective Disorders, 150, 513–521.
Lin, C.-H., Yen, Y.-C., Chen, M.-C., & Chen, C.-C. (2014). Depression and pain impair daily functioning and quality of life in patients with major depressive disorder. Journal of Affective Disorders, 166, 173–178.
Lin, C.-H., Yen, Y.-C., Chen, M.-C., & Chen, C.-C. (2013). Relief of depression and pain improves daily functioning and quality of life in patients with major depressive disorder. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 47, 93–98.
Chung, K.-F., Tso, K.-C., Yeung, W.-F., & Li, W.-H. (2012). Quality of life in major depressive disorder: the role of pain and pain catastrophizing cognition. Comprehensive Psychiatry, 53, 387–395.
Beard, C., Weisberg, R. B., & Keller, M. B. (2010). Health-related Quality of Life across the anxiety disorders: Findings from a sample of primary care patients. Journal of Anxiety Disorders, 24, 559–564.
ten Doesschate, M. C., Koeter, M. W. J., Bockting, C. L. H., & Schene, A. H. (2010). Health related quality of life in recurrent depression: A comparison with a general population sample. Journal of Affective Disorders, 120, 126–132.
Jansen, K., Campos Mondin, T., da Costa, Ores L., et al. (2011). Transtornos mentais comuns e qualidade de vida em jovens: uma amostra populacional de Pelotas, Rio Grande do Sul, Brasil. Cad Saúde Pública, 27, 440–448.
Lima, M. G., de Barros, M. B., César, C. L. G., et al. (2009). Impact of chronic disease on quality of life among the elderly in the state of São Paulo, Brazil: A population-based study. Revista Panamericana de Salud Pública, 25, 314–321.
Steiner, A. J., Recacho, J., Vanle, B., et al. (2017). Quality of life, functioning, and depressive symptom severity in older adults with major depressive disorder treated with citalopram in the STAR*D Study. Journal of Clinical Psychiatry, 78, 897–903.
Mack, S., Jacobi, F., Beesdo-Baum, K., et al. (2015). Functional disability and quality of life decrements in mental disorders: Results from the Mental Health Module of the German Health Interview and Examination Survey for Adults (DEGS1-MH). European Psychiatry, 30, 793–800.
Lokkerbol, J., Adema, D., De Graaf, R., et al. (2013). Non-fatal burden of disease due to mental disorders in the Netherlands. Social Psychiatry and Psychiatric Epidemiology, 48, 1591–1599.
Sareen, J., Jacobi, F., Cox, B. J., et al. (2006). Disability and poor quality of life associated with comorbid anxiety disorders and physical conditions. Archives of Internal Medicine, 166, 2109.
Crempien, C., Grez, M., Valdés, C., et al. (2017). Role of personality functioning in the quality of life of patients with depression. The Journal of Nervous and Mental Disease, 205, 705–713.
Herzog, A., Shedden-Mora, M. C., Jordan, P., & Löwe, B. (2018). Duration of untreated illness in patients with somatoform disorders. Journal of Psychosomatic Research, 107, 1–6.
Alves, M. C. G. P., Escuder, M. M. L., Claro, R. M., & Da Silva, N. N. (2014). Sorteio intradomiciliar em inquéritos de saúde. Revista de Saude Publica, 48, 86–93.
McDowell, I. (2006). Measuring health: A guide to rating scales and questionnaires (3rd ed.). New York: Oxford University Press Inc.
Ware, J. E., Kosinski, M., Bjorner, J. B., et al. (2007). User’s manual for the 36v2 ® health survey (2nd ed.). Lincoln, RI: QualityMetric Incorporated.
Ciconelli, R. M., Ferraz, M. B., Santos, W., et al. (1999). Tradução para a língua portuguesa e validação do questionário genérico de avaliação de qualidade de vida SF-36 (Brasil SF-36). Revista Brasileira de Reumatologia, 39, 143–150.
Laguardia, J., Campos, M. R., Travassos, C., et al. (2013). Dados normativos brasileiros do questionário Short Form-36 versão 2. The Revista Brasileira de Epidemiologia, 16, 889–897.
Centro colaborador da OMS para a Classificação de Doenças em Português. (2018). Classificação Estatística Internacional de Doenças e Problemas Relacionados à Saúde - CID-10. Retrieved from http://www.datasus.gov.br/cid10/V2008/cid10.htm
Pappa, E., Chatzikonstantinidou, S., & Chalkiopoulos, G. (2015). Health-related quality of life of the Roma in Greece: The role of socio-economic characteristics and housing conditions. International Journal of Environmental Research and Public Health, 12, 6669–6681.
Bayliss, M., Rendas-baum, R., White, M. K., et al. (2012). Health-related quality of life (HRQL) for individuals with self-reported chronic physical and/or mental health conditions: Panel survey of an adult sample in the United States. Health and Quality of Life Outcomes, 10, 1.
Campanha, A. M., Siu, E. R., Milhorança, I. A., et al. (2015). Use of psychotropic medications in São Paulo Metropolitan Area, Brazil: pattern of healthcare provision to general population. Pharmacoepidemiology and Drug Safety, 24, 1207–1214. https://doi.org/10.1002/pds.3826.
Ribeiro, W. S., de Mari, J., Quintana, M. I., et al. (2013). The impact of epidemic violence on the prevalence of psychiatric disorders in Sao Paulo and Rio de Janeiro, Brazil. PLoS ONE, 8, 1–13.
Kessler, R. C., Aguilar-Gaxiola, S., Alonso, J., et al. (2009). The global burden of mental disorders: an update from the WHO World Mental Health (WMH) surveys. Epidemiology and Psychiatric Sciences, 18, 23–33.
Guan, B., Deng, Y., Cohen, P., & Chen, H. (2011). Relative impact of Axis I mental disorders on quality of life among adults in the community. Journal of Affective Disorders, 131, 293–298. https://doi.org/10.1016/J.JAD.2011.01.010.
Brown, P. J., & Roose, S. P. (2011). Age and anxiety and depressive symptoms: the effect on domains of quality of life. International Journal of Geriatric Psychiatry, 26, 1260–1266.
Zhao, N., Wang, X., Wu, W., et al. (2017). Gender differences in quality of life and functional disability for depression outpatients with or without residual symptoms after acute phase treatment in China. Journal of Affective Disorders, 219, 141–148. https://doi.org/10.1016/J.JAD.2017.05.021.
Tavares, N. U. L., Costa, K. S., Mengue, S. S., et al. (2015). Uso de medicamentos para tratamento de doenças crônicas não transmissíveis no Brasil: resultados da Pesquisa Nacional de Saúde, 2013. Epidemiol e Serviços Saúde, 24, 315–323.
Malta, D. C., Bernal, R. T. I., de Souza, M., et al. (2016). Social inequalities in the prevalence of self-reported chronic non-communicable diseases in Brazil: national health survey 2013. International Journal for Equity in Health, 15, 153.
Navin Cristina, T. J., Stewart Williams, J. A., Parkinson, L., et al. (2016). Identification of diabetes, heart disease, hypertension and stroke in mid- and older-aged women: Comparing self-report and administrative hospital data records. Geriatrics & Gerontology International, 16, 95–102.
Muggah, E., Graves, E., Bennett, C., & Manuel, D. G. (2013). Ascertainment of chronic diseases using population health data: A comparison of health administrative data and patient self-report. BMC Public Health, 13, 16.
Barros, M., Lima, M., Azevedo, R., et al. (2017). Depression and health behaviors in Brazilian adults – PNS 2013 – PNS 2013. Rev Saúde Pública, 51(1), 8s.
Acknowledgements
The authors are grateful to State of São Paulo Research Assistance Foundation (FAPESP), for funding the fieldwork for ISACamp 2014/15. The Campinas Municipal Secretary of Health and Health Surveillance Secretary of the Health Ministry for financial support for the execution of the survey. The National Council of Technological and Scientific Development (CNPq) funded the productivity scholarship granted to M.B.A. Barros (Grant Number: 309073/2015-4); and FAPESP (Grant Number 2015/16161-9) for the doctoral grant awarded to C.S.E. Fernandes.
Funding
This study was funded by State of São Paulo Research Assistence Foundation (FAPESP), Grant Number: 2012/23324-3 and the Campinas Municipal Secretary of Health and Health Surveillance Secretary of the Health Ministry; and FAPESP funded doctoral grant awarded to C.S.E. Fernandes.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The ISACamp 2014/2015 Project received approval from the Human Research Ethics Committee of Campinas State University (Certificate Number: 409.714 of September 30th, 2013). This study was approved by the Human Research Ethics Committee of Campinas State University under number: CAAE: 02181418.9.0000.5404. All interviewees signed a statement of informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Estancial Fernandes, C.S., Lima, M.G. & Barros, M.B.A. Emotional problems and health-related quality of life: population-based study. Qual Life Res 28, 3037–3046 (2019). https://doi.org/10.1007/s11136-019-02230-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-019-02230-9