Abstract
Purpose
Loneliness is a known risk factor for poor mental and physical health outcomes and quality of life in the general population, and preliminary research suggests that loneliness is linked to poorer health outcomes in cancer patients as well. Various aspects of the cancer experience contribute to patients feeling alone and misunderstood. Furthermore, loneliness theory suggests that negative social expectations, which may specifically relate to the cancer experience, precipitate and sustain loneliness. Cancer-specific tools are needed to assess key constructs of this theory. In the current study, we developed and tested measures of (1) loneliness attributed to cancer (i.e., cancer-related loneliness) and (2) negative social expectations related to cancer.
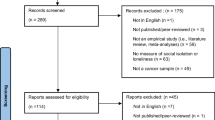
Methods
First, we developed the items for the measures based on theory, prior research, and expert feedback. Next, we assessed the measures’ psychometric properties (i.e., internal consistency and construct validity) in a diverse sample of cancer patients.
Results
The final products included a 7-item unidimensional Cancer Loneliness Scale and a 5-item unidimensional Cancer-related Negative Social Expectations Scale. Evidence of excellent reliability and validity was found for both measures.
Conclusions
The resulting measures have both clinical and research utility.


Similar content being viewed by others
References
Hawkley, L. C., & Cacioppo, J. T. (2003). Loneliness and pathways to disease. Brain, Behavior, and Immunity, 17(1), 98–105. doi:10.1016/S0889-1591(02)00073-9.
Cacioppo, J. T., & Hawkley, L. C. (2009). Perceived social isolation and cognition. Trends in Cognitive Sciences, 13(10), 447–454. doi:10.1016/j.tics.2009.06.005.
Cacioppo, J. T., Hawkley, L. C., & Thisted, R. A. (2010). Perceived social isolation makes me sad: 5-Year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychology and Aging, 25(2), 453–463. doi:10.1037/a0017216.
Hawkley, L. C., Thisted, R. A., Masi, C. M., & Cacioppo, J. T. (2010). Loneliness predicts increased blood pressure: 5-Year cross-lagged analyses in middle-aged and older adults. Psychology and Aging, 25(1), 132–141. doi:10.1037/a0017805.
Jaremka, L. M., Andridge, R. R., Fagundes, C. P., Alfano, C. M., Povoski, S. P., Lipari, A. M., et al. (2014). Pain, depression, and fatigue: Loneliness as a longitudinal risk factor. Health Psychology, 33(9), 948–957. doi:10.1037/a0034012.
Jaremka, L. M., Fagundes, C. P., Peng, J., Bennett, J. M., Glaser, R., Malarkey, W. B., et al. (2013). Loneliness promotes inflammation during acute stress. Psychological Science, 24(7), 1089–1097. doi:10.1177/0956797612464059.
Drageset, J., Eide, G. E., Kirkevold, M., & Ranhoff, A. H. (2013). Emotional loneliness is associated with mortality among mentally intact nursing home residents with and without cancer: A 5-year follow-up study. Journal of Clinical Nursing, 22(1–2), 106–114. doi:10.1111/j.1365-2702.2012.04209.x.
Nausheen, B., Carr, N. J., Peveler, R. C., Moss-Morris, R., Verrill, C., Robbins, E., et al. (2010). Relationship between loneliness and proangiogenic cytokines in newly diagnosed tumors of colon and rectum. Psychosomatic Medicine, 72(9), 912–916. doi:10.1097/PSY.0b013e3181f0bc1c.
Peplau, L. A., & Perlman, D. (1982). Perspectives on loneliness. In L. A. Peplau & D. Perlman (Eds.), Loneliness: A sourcebook of current theory, research and therapy (pp. 1–18). New York: Wiley.
Russell, D. W. (1996). UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. Journal of Personality Assessment, 66(1), 20–40. doi:10.1207/s15327752jpa6601.
Deckx, L., van den Akker, M., & Buntinx, F. (2014). Risk factors for loneliness in patients with cancer: A systematic literature review and meta-analysis. European Journal of Oncology Nursing, 18(5), 466–477. doi:10.1016/j.ejon.2014.05.002.
Adams, R. N., Mosher, C. E., Abonour, R., Robertson, M. J., Champion, V. L., & Kroenke, K. (2016). Cognitive and situational precipitants of loneliness among patients with cancer: A qualitative analysis. Oncology Nursing Forum, 43(2), 156–163. doi:10.1188/16.ONF.156-163.
Rosedale, M. (2009). Survivor loneliness of women following breast cancer. Oncology Nursing Forum, 36, 175–183. doi:10.1188/09.ONF.175-183.
Lepore, S., & Revenson, T. (2007). Social constraints on disclosure and adjustment to cancer. Social and Personality Psychology Compass, 1(1), 313–333. doi:10.1111/j.1751-9004.2007.00013.x.
Adams, R. N., Winger, J. G., & Mosher, C. E. (2015). A meta-analysis of the relationship between social constraints and distress in cancer patients. Journal of Behavioral Medicine, 38(2), 294–305. doi:10.1007/s10865-014-9601-6.
Mosher, C. E., Lepore, S., Wu, L., Austin, J., Valdimarsdottir, H., Rowley, S., et al. (2012). Social correlates of distress following hematopoietic stem cell transplantation: Exploring the role of loneliness and cognitive processing. Journal of Health Psychology, 17(7), 1022–1032. doi:10.1177/1359105311432490.
Masi, C. M., Chen, H.-Y., Hawkley, L. C., & Cacioppo, J. T. (2010). A meta-analysis of interventions to reduce loneliness. Personality and Social Psychology Review, 15, 219–266. doi:10.1177/1088868310377394.
Cutrona, C. E. (1982). Transition to college: Loneliness and the process of social adjustment. In L. A. Peplau & D. Perlman (Eds.), Loneliness: A sourcebook of current theory, research, and therapy (pp. 291–309). New York: Wiley.
Cacioppo, J. T., Hawkley, L. C., Ernst, J. M., Burleson, M., Berntson, G. G., Nouriani, B., et al. (2006). Loneliness within a nomological net: An evolutionary perspective. Journal of Research in Personality, 40(6), 1054–1085. doi:10.1016/j.jrp.2005.11.007.
de Jong-Gierveld, J. (1987). Developing and testing a model of loneliness. Journal of Personality and Social Psychology, 53(1), 119–128. doi:10.1037//0022-3514.53.1.119.
de Jong-Gierveld, J., & Van Tilburg, T. (2006). A 6-item scale for overall, emotional, and social loneliness confirmatory tests on survey data. Research on Aging, 28(5), 582–598. doi:10.1177/0164027506289723.
Vincenzi, H., & Grabosky, F. (1987). Measuring the emotional/social aspects of loneliness and isolation. Journal of Social Behavior & Personality, 2(2), 257–270.
Sand, L., Strang, P., & Milberg, A. (2008). Dying cancer patients’ experiences of powerlessness and helplessness. Supportive Care in Cancer, 16(7), 853–862. doi:10.1007/s00520.
Lepore, S. (2001). A social–cognitive processing model of emotional adjustment to cancer. In A. Baum & B. L. Andersen (Eds.), Psychosocial interventions for cancer (pp. 99–118). Washington, DC: American Psychological Association.
Manne, S., Norton, T. R., Ostroff, J. S., Winkel, G., Fox, K., & Grana, G. (2007). Protective buffering and psychological distress among couples coping with breast cancer: The moderating role of relationship satisfaction. Journal of Family Psychology, 21(3), 380–388. doi:10.1037/0893-3200.21.3.380.
Langer, S. L., Brown, J. D., & Syrjala, K. L. (2009). Intrapersonal and interpersonal consequences of protective buffering among cancer patients and caregivers. Cancer, 115(S18), 4311–4325. doi:10.1002/cncr.24586.
Lepore, S., & Helgeson, V. (1998). Social constraints, intrusive thoughts, and mental health after prostate cancer. Journal of Social and Clinical Psychology, 17(1), 89–106. doi:10.1521/jscp.1998.17.1.89.
Manne, S., Sherman, M., Ross, S., Ostroff, J., Heyman, R. E., & Fox, K. (2004). Couples’ support-related communication, psychological distress, and relationship satisfaction among women with early stage breast cancer. Journal of Consulting and Clinical Psychology, 72(4), 660–670. doi:10.1037/0022-006X.72.4.660.
Cella, D., Riley, W., Stone, A., Rothrock, N., Reeve, B., Yount, S., et al. (2010). The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. Journal of Clinical Epidemiology, 63(11), 1179–1194. doi:10.1016/j.jclinepi.2010.04.011.
Cella, D., Yount, S., Rothrock, N., Gershon, R., Cook, K., Reeve, B., et al. (2007). The Patient-Reported Outcomes Measurement Information System (PROMIS): Progress of an NIH Roadmap cooperative group during its first two years. Medical Care, 45(5 Suppl 1), S3–S11. doi:10.1097/01.mlr.0000258615.42478.55.
Magasi, S., Ryan, G., Revicki, D., Lenderking, W., Hays, R. D., Brod, M., et al. (2012). Content validity of patient-reported outcome measures: Perspectives from a PROMIS meeting. Quality of Life Research, 21(5), 739–746. doi:10.1007/s11136-009-9496-9.
Badr, H., Smith, C. B., Goldstein, N. E., Gomez, J. E., & Redd, W. H. (2015). Dyadic psychosocial intervention for advanced lung cancer patients and their family caregivers: Results of a randomized pilot trial. Cancer, 121(1), 150–158. doi:10.1002/cncr.29009.
Baum, G., Basen-Engquist, K., Swartz, M. C., Parker, P. A., & Carmack, C. L. (2014). Comparing PROMIS computer-adaptive tests to the Brief Symptom Inventory in patients with prostate cancer. Quality of Life Research, 23(7), 2031–2035. doi:10.1007/s11136-014-0647-2.
Hays, R. D., Bjorner, J. B., Revicki, D. A., Spritzer, K. L., & Cella, D. (2009). Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Quality of Life Research, 18(7), 873–880. doi:10.1007/s11136-009-9496-9.
Hahn, E. A., DeWalt, D. A., Bode, R. K., Garcia, S. F., DeVellis, R. F., Correia, H., et al. (2014). New English and Spanish social health measures will facilitate evaluating health determinants. Health Psychology, 33(5), 490–499. doi:10.1037/hea0000055.
Choi, S. W., Reise, S. P., Pilkonis, P. A., Hays, R. D., & Cella, D. (2010). Efficiency of static and computer adaptive short forms compared to full-length measures of depressive symptoms. Quality of Life Research, 19(1), 125–136.
Pilkonis, P. A., Choi, S. W., Reise, S. P., Stover, A. M., Riley, W. T., & Cella, D. (2011). Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): Depression, anxiety, and anger. Assessment, 18(3), 263–283. doi:10.1177/1073191111411667.
Vassar, M., & Crosby, J. W. (2008). A reliability generalization study of coefficient alpha for the UCLA Loneliness Scale. Journal of Personality Assessment, 90(6), 601–607. doi:10.1080/00223890802388624.
Cohen, S., Doyle, W. J., Skoner, D. P., Rabin, B. S., & Gwaltney, J. M. (1997). Social ties and susceptibility to the common cold. JAMA: The Journal of the American Medical Association, 277(24), 1940–1944. doi:10.1001/jama.
Kline, R. B. (2011). Principles and practice of structural equation modeling (2nd ed.). New York: The Guilford Press.
Tukey, J. W. (1962). The future of data analysis. The Annals of Mathematical Statistics, 33(1), 1–67.
Little, R. J. A. (1988). A test of missing completely at random for multivariate data with missing values. Journal of the American Statistical Association, 83(404), 1198–1202. doi:10.1080/01621459.1988.10478722.
Hu, L., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6(1), 1–55. doi:10.1080/10705519909540118.
Egestad, H. (2013). The significance of fellow patients for head and neck cancer patients in the radiation treatment period. European Journal of Oncology Nursing, 17(5), 618–624. doi:10.1016/j.ejon.2013.01.001.
Beck, A. T., & Bredemeier, K. (2016). A unified model of depression integrating clinical, cognitive, biological, and evolutionary perspectives. Clinical Psychological Science. doi:10.1177/2167702616628523.
Pinquart, M., & Sorensen, S. (2001). Influences on loneliness in older adults: A meta-analysis. Basic and Applied Social Psychology, 23(4), 245–266. doi:10.1207/153248301753225702.
Eakin, E. G., & Strycker, L. A. (2001). Awareness and barriers to use of cancer support and information resources by HMO patients with breast, prostate, or colon cancer: Patient and provider perspectives. Psycho-Oncology, 10(2), 103–113. doi:10.1002/pon.500.
Wells, M., & Kelly, D. (2008). The loneliness of cancer. European Journal of Oncology Nursing, 12(5), 410–411. doi:10.1016/j.ejon.2008.11.003.
Jaremka, L. M., Fagundes, C. P., Glaser, R., Bennett, J. M., Malarkey, W. B., & Kiecolt-Glaser, J. K. (2013). Loneliness predicts pain, depression, and fatigue: Understanding the role of immune dysregulation. Psychoneuroendocrinology, 38(8), 1310–1317. doi:10.1016/j.psyneuen.2012.11.016.
Jaremka, L. M., Peng, J., Bornstein, R., Alfano, C. M., Andridge, R. R., Povoski, S. P., et al. (2014). Cognitive problems among breast cancer survivors: Loneliness enhances risk. Psycho-Oncology, 23(12), 1356–1364. doi:10.1002/pon.3544.
Acknowledgements
This project was supported by the American Psychological Association. Rebecca Adams’s work was supported by R25CA117865 (V. Champion, PI) from the National Cancer Institute. Catherine Mosher’s work was supported by the National Cancer Institute under Grants K05CA175048 and K07CA168883. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute. The authors would like to thank the study participants and Madison Stout for her assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Adams, R.N., Mosher, C.E., Rand, K.L. et al. The Cancer Loneliness Scale and Cancer-related Negative Social Expectations Scale: development and validation. Qual Life Res 26, 1901–1913 (2017). https://doi.org/10.1007/s11136-017-1518-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-017-1518-4