Abstract
Purpose
The purpose of this investigation was to determine if it was possible to separate fatigue self-reports into two distinct types of fatigue symptom clusters in research subjects with chronic liver disease (CLD). It was hypothesized that when items from the Medical Outcomes Study Short-Form (SF-36v2) are combined with items from the Fatigue Severity Scale (FSS), these distinct factors will emerge.
Methods
Confirmatory and exploratory factor analyses from data collected in a prospective, natural history study of CLD patients were conducted. Items were selected from the SF-36v2 and the FSS for entry into the factor analyses. In order to establish convergent and discriminant validity, derived factor scores were correlated with subscale scores of the Human Activity Profile (HAP), Mental Component Score (MCS) from the SF-36v2, and the Emotional Functioning Subscale of the Chronic Liver Disease Questionnaire (CLDQ-EF).
Results
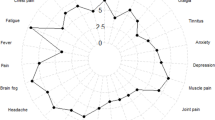
106 participants with CLD were included (50% female; age: 51 ± 10). Two factors were identified. The factors included one that clustered around questions addressing fatigue related to physical activity (peripheral fatigue) and the other to the questions addressing generalized fatigue that did not require physical tasks to produce the fatigue (central fatigue). The standardized factor loadings of all items were greater than 0.6 on their underlying constructs. Moreover, all factor loadings are significant at p < 0.01. Peripheral fatigue was related to HAP (r = 0.26, r = 0.24, p < 0.01), as was central fatigue (r = −0.34, r = −0.33, p < 0.01). Central fatigue was related to MCS and CLDQ-EF (r = −0.60; r = −0.63, p < 0.01), whereas peripheral fatigue was not (r = 0.07, p > 0.40). We then tested the original scales to determine if the newly created factors correlated better with the validity measures. The full FSS did not correlate as well as the newly created central fatigue scale, while the original peripheral fatigue scale (the SF-36v2 physical functioning) was more related to HAP than the newly created scale.
Conclusions
In individuals with CLD, two separate factors pertaining to fatigue were identified. This recognition of the multifaceted nature of fatigue may help increase the specificity of self-reports of fatigue and lead to treatments that can specifically address the underlying factors contributing to fatigue.
Similar content being viewed by others
References
Swain, M.G. (2006). Fatigue in liver disease: Pathophysiology and clinical management. Canadian Journal of Gastroenterology, 20(3), 181–188.
Kumar, D., & Tandon, R K. (2002). Fatigue in cholestatic liver disease–a perplexing symptom. Postgraduate Medical Journal, 78(921), 404–407.
Milkiewicz, P., & Heathcote, E.J. (2004). Fatigue in chronic cholestasis. Gut, 53(4), 475–477.
Poynard, T., Cacoub, P., Ratziu, V., Myers, R.P., Dezailles, M.H., Mercadier, A., … Multivirc Group (2002). Fatigue in patients with chronic hepatitis C. Journal of Viral Hepatitis, 9(4), 295–303.
Cauch-Dudek, K., Abbey, S., Stewart, D., & Heathcote, E. (1998). Fatigue in primary biliary cirrhosis. Gut, 43(5), 705–710.
Huet, P.M., Deslauriers, J., Tran, A., Faucher, C., & Charbonneau, J. (2000). Impact of fatigue on the quality of life of patients with primary biliary cirrhosis. The American Journal of Gastroenterology, 95(3), 760–767. doi:10.1111/j.1572-0241.2000.01857.x.
Newton, J.L., Jones, D.E.J., Henderson, E., Kane, L., Wilton, K., Burt, A.D., et al. (2008). Fatigue in non-alcoholic fatty liver disease (NAFLD) is significant and associates with inactivity and excessive daytime sleepiness but not with liver disease severity or insulin resistance. Gut, 57(6), 807–813. doi:10.1136/gut.2007.139303.
Younossi, Z.M., Kiwi, M.L., Boparai, N., Price, L.L., & Guyatt, G. (2000). Cholestatic liver diseases and health-related quality of life. The American Journal of Gastroenterology, 95(2), 497–502. doi:10.1111/j.1572-0241.2000.01774.x.
Tiesinga, L.J., Dassen, T.W., & Halfens, R.J. (1996). Fatigue: A summary of the definitions, dimensions, and indicators. Nursing Diagnosis: ND: The Official Journal of the North American Nursing Diagnosis Association, 7(2), 51–62.
Gandevia, S.C., Allen, G.M., & McKenzie, D.K. (1995). Central fatigue. Critical issues, quantification and practical implications. Advances in Experimental Medicine and Biology, 384, 281–294.
Chaudhuri, A., & Behan, P. O. (2000). Fatigue and basal ganglia. Journal of the Neurological Sciences, 179(1–2), 34–42.
Chaudhuri, A., & Behan, P.O. (2004). Fatigue in neurological disorders. Lancet, 363(9413), 978–988. doi:10.1016/S0140-6736(04)15794-2.
Wessely, S., Hotopf, M., & Sharpe, M. (1998). Chronic fatigue and its syndromes (1st ed.). Oxford: Oxford University Press.
Leavitt, V.M., & DeLuca, J. (2010). Central fatigue: Issues related to cognition, mood and behavior, and psychiatric diagnoses. PM & R: The Journal of Injury, Function, and Rehabilitation, 2(5), 332–337. doi:10.1016/j.pmrj.2010.03.027.
Duntley, S. (2005). Fatigue and sleep. In J. DeLuca (Ed.), Fatigue as a window to the brain (pp. 209–228). MIT Press.
Secher, N. (1992). Central nervous influence on fatigue. In Endurance in sport (pp. 96–106). Boston, MA: Blackwell Scientific.
Bigland-Ritchie, B., Furbush, F., & Woods, J.J. (1986). Fatigue of intermittent submaximal voluntary contractions: Central and peripheral factors. Journal of Applied Physiology (Bethesda, Md.: 1985), 61(2), 421–429.
Enoka, R.M., & Stuart, D.G. (1992). Neurobiology of muscle fatigue. Journal of Applied Physiology (Bethesda, Md.: 1985), 72(5), 1631–1648.
Cella, D., Lai, J.-S., & Stone, A. (2011). Self-reported fatigue: One dimension or more? lessons from the functional assessment of chronic illness therapy–fatigue (FACIT-F) questionnaire. Supportive Care in Cancer: Official Journal of the Multinational Association of Supportive Care in Cancer, 19(9), 1441–1450. doi:10.1007/s00520-010-0971-1.
McHorney, C.A., Ware, J.E., & Raczek, A.E. (1993). The MOS 36-Item short-form health survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Medical Care, 31(3), 247–263.
Kleinman, L., Zodet, M.W., Hakim, Z., Aledort, J., Barker, C., Chan, K., et al. (2000). Psychometric evaluation of the fatigue severity scale for use in chronic hepatitis C. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 9(5), 499–508.
Loria, A., Doyle, K., Weinstein, A.A., Winter, P., Escheik, C., Price, J., et al. (2014). Multiple factors predict physical performance in people with chronic liver disease. American Journal of Physical Medicine & Rehabilitation Association of Academic Physiatrists. doi:10.1097/PHM.0000000000000050.
Staniute, M., Bunevicius, A., Brozaitiene, J., & Bunevicius, R. (2014). Relationship of health-related quality of life with fatigue and exercise capacity in patients with coronary artery disease. European Journal of Cardiovascular Nursing, 13(4), 338–344.
Krupp, L.B., LaRocca, N.G., Muir-Nash, J., & Steinberg, A.D. (1989). The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Archives of Neurology, 46(10), 1121–1123.
Fix, A., & Daughton, D. (1988). Human activity profile professional manual. Odessa, FL: Psychological Assessment Resources, Inc.
Younossi, Z.M., Guyatt, G., Kiwi, M., Boparai, N., & King, D. (1999). Development of a disease specific questionnaire to measure health related quality of life in patients with chronic liver disease. Gut, 45(2), 295–300.
Pedhazur, E.J., & Schmelkin, L.P. (1991). Measurement, design, and analysis: An integrated approach (Student edition.). Hillsdale: Psychology Press.
Nunnally, J.C., & Bernstein, I.H. (1994). Psychometric theory (3rd ed.). New York: McGraw-Hill.
Hair, J., Black, W., Babin, B., & Anderson, R. (2010). Multivariate data analysis: A global perspective (7th ed.). Saddle River, NJ: Pearson Education, Inc.
Kline, R.B. (2005). Principles and practice of structural equation modeling (2nd edition). New York: The Guilford Press.
Jöreskog, K., & Sörbom, D. (1993). LISREL 8: Structural equation modeling with the SIMPLIS command language. Chicago, IL: Scientific Software International Inc.
Tabachnick, B.G. & Fidell, L.S. (2007). Using multivariate statistics (5th ed.). New York: Allyn and Bacon.
Hu, L.T., & Bentler, P.M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6(1), 1–55.
Bentler, P.M., & Bonnet, D.C. (1980). Significance tests and goodness of fit in the analysis of covariance structures. Psychological Bulletin, 88(3), 588–606.
Steiger, J.H. (1990). Structural model evaluation and modification: An interval estimation approach. Multivariate Behavioral Research, 25(2), 173–180.
Marcora, S.M., Staiano, W., & Manning, V. (2009). Mental fatigue impairs physical performance in humans. Journal of Applied Physiology (Bethesda, Md.: 1985), 106(3), 857–864. doi:10.1152/japplphysiol.91324.2008.
Davidson, M., & de Morton, N. (2007). A systematic review of the human activity profile. Clinical Rehabilitation, 21(2), 151–162.
Jason, L.A., Evans, M., Brown, M., & Porter, N. (2010). What is fatigue? pathological and nonpathological fatigue. PM & R: The Journal of Injury, Function, and Rehabilitation, 2(5), 327–331. doi:10.1016/j.pmrj.2010.03.028.
MacCallum, R.C., Widaman, K.F., Zhang, S., & Hong, S. (1999). Sample size in factor analysis. Psychological Methods, 4(1), 84–89.
Acknowledgements
This work was supported by the Betty and Guy Beatty Center for Integrated Research.
Funding
This work was funded by the Betty and Guy Beatty Center for Integrated Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Weinstein, A.A., Diao, G., Baghi, H. et al. Demonstration of two types of fatigue in subjects with chronic liver disease using factor analysis. Qual Life Res 26, 1777–1784 (2017). https://doi.org/10.1007/s11136-017-1516-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-017-1516-6