Abstract
Objectives
This study explored the relationship between the M. D. Anderson Symptom Inventory (MDASI), an instrument measuring the severity of symptoms common to patients with cancer, and utility derived from the SF-36.
Methods
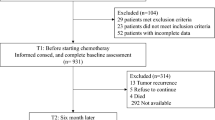
Cancer patients from Tianjin Cancer Hospital in China (n = 249) completed a demographic questionnaire and Chinese versions of the MDASI and SF-36. Using a published algorithm converting SF-36 scores to standard gamble (SG) utilities, we examined the association between utility and individual symptoms using Spearman’s rank correlation, and explored the association between utility and aggregate symptom scores through multivariate regression analyses.
Results
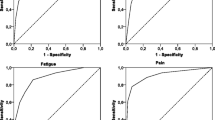
The mean SG utility was 0.81 (SD = 0.11); utilities were significantly but moderately correlated with the majority of symptoms, especially those of distress, sadness, fatigue, and pain. Regression models showed a significantly negative association between the total symptom score and the utility. After controlling for sociodemographics, cancer stage and performance status, a significantly negative association between the total symptom scores and utility was found in the multivariate analyses. We also found the total number of severe symptoms to be a stronger predictor of “disutility.”
Conclusions
Symptom measures were significantly albeit moderately associated with utility derived from the SF-36 scores, suggesting that a full study with rigorously collected utilities is worth exploring.
Similar content being viewed by others
References
Siegel JE, Weinstein MC, Russell LB, et al (1996). Recommendations for reporting cost-effectiveness analyses. Panel on cost-effectiveness in health and medicine. JAMA 276(16):1339–1341
Weinstein MC, Siegel JE, Gold MR, et al (1996). Recommendations of the panel on cost-effectiveness in health and medicine. JAMA 276(15):1253–1258
Gold MR, Siegel JE, Russell LB, Weinstein MC (1996). Cost-Effectiveness in Health and Medicine. New York, Oxford University Press
Earle CC, Chapman RH, Baker CS, et al. (2000). Systematic overview of cost-utility assessments in oncology. J Clin Oncol 18(18):3302–3317
Raiffa H (1968). Decision Analysis: Introductory Lectures on Choices under Uncertainty. New York, Random House
Cantor SB (1995). Decision analysis: Theory and application to medicine. Prim Care 22(2):261–270
Pliskin JS, Shepard DS, Weinstein MC (1980). Utility functions for life years and health status. Oper Res 28:206–224
Cleeland CS, Mendoza TR, Wang XS, et al (2000). Assessing symptom distress in cancer patients: The M. D. Anderson Symptom Inventory. Cancer 89(7):1634–1646
Kiebert GM, Curran D, Aaronson NK, et al. (1998). Quality of life after radiation therapy of cerebral low-grade gliomas of the adult: Results of a randomized phase III trail on dose response (CORTC trial 22844). EORTC Radiotherapy Co-operative Group. Eur J Cancer 34(12):1902–1909
Kramer JA, Curran D, Piccart M, et al (2000). Randomised trial of paclitaxel vs doxorubicin as first-line chemotherapy for advanced breast cancer: Quality of life evaluation using the EORTC QLQ-C30 and the Rotterdam symptom checklist. Eur J Cancer 36(12):1488–1497
Wang XS, Wang Y, Guo H, et al. (2004). Chinese version of the M. D. Anderson Symptom Inventory: Validation and application of symptom measurement in cancer patients. Cancer 101(8):1890–1901
Okuyama T, Wang XS, Akechi T, et al. (2003). Japanese version of the M. D. Anderson Symptom Inventory: A validation study. J Pain Symptom Manage 26(6):1093–1104
Mystakidou K, Cleeland CS, Tsilika E, et al. (2004). Greek M.D. Anderson Symptom Inventory: validation and utility in cancer patients. Oncology 67(3–4):203–210
Wang XS, Mendoza TR, Gao SZ, Cleeland CS (1996). The Chinese version of the Brief Pain Inventory (BPI-C): Its development and use in a study of cancer pain. Pain 67(2–3):407–416
Cleeland CS, Reyes-Gibby CC (2002). When is it justified to treat symptoms? Measuring symptom burden. Oncology 16(9):64–70
Brazier J, Usherwood T, Harper R, Thomas K (1998). Deriving a preference-based single index from the UK SF-36 Health Survey. J Clin Epidemiol 51(11):1115–1128
Brazier J, Roberts J, Deverill M (2002). The estimation of a preference-based measure of health from the SF-36. J Health Econ 21(2):271–292
Ware JE Jr, Sherbourne CD (1992). The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30(6):473–483
Wang XS, Cleeland CS, Mendoza TR, et al. (1999). The effects of pain severity on health-related quality of life: A study of Chinese cancer patients. Cancer 86(9):1848–1855
Ren XS, Wang XS, Liu S, Hao X (2003). Psychometric and clinical evaluation of the Chinese version of the SF-36 health survey among cancer patients in China. Qual Life Res Newslett 30:5–7
Brazier JE, Roberts J (2004) The estimation of a preference-based measure of health from the SF-12. Med Care 42(9):851–859
O’Brien BJ, Spath M, Blackhouse G, et al. (2003). A review from the bridge: Agreement between the SF-6D utility algorithm and the Health Utilities Index. Health Econ 12:975–981
Torrance GW (1986) Measurement of health state utilities for economic appraisal. J Health Econ 5(1):1–30. Review
Torrance GW, Feeny D (1989). Utilities and quality-adjusted life years. Int J Technol Assess Health Care 5(4):559–575
Oken MM, Creech RH, Tormey DC, et al. (1982). Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5(6):649–655
Revicki DA, Kaplan RM (1993). Relationship between psychometric and utility-based approaches to the measurement of health-related quality of life. Qual Life Res 2:477–487
Stiggelbout AM, de Haes JCJM (2001). Patient preference for cancer therapy: An overview of measurement approaches. J Clin Oncol 19(1):220–230
Cleeland CS, Serlin RC, Nakamura Y, et al. (1997). Effects of culture and language on ratings of cancer pain and patterns of functional interference. In: Jensen TS, Turner JA, Wiesenfeld-Hallin Z, (eds). Progress in Pain Research and Management. Seattle, IASP Press, pp. 35–51
Serlin RC, Mendoza TR, Nakamura Y, et al (1995). When is cancer pain mild, moderate or severe? Grading pain severity by its interference with function. Pain 61:277–284
Hui EC (2005). The centrality of patient-physician relationship to medical professionalism: An ethical evaluation of some contemporary models. Hong Kong Med J 11(3):222–223
Sloan JA, Loprinzi CL, Laurine JA, et al (2001). A simple stratification factor prognostic for survival in advanced cancer: The good/bad/uncertain index. J Clin Oncol 19(15):3539–3546
Acknowledgements
The authors would like to thank Dr. Xi-Shan Hau and Ms. Ying Wang at Tianjin Cancer Hospital, Tianjin Medical University, China, for their assistance in data collection.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shih, YC.T., Wang, X.S., Cantor, S.B. et al. The Association between Symptom Burdens and Utility in Chinese Cancer Patients. Qual Life Res 15, 1427–1438 (2006). https://doi.org/10.1007/s11136-006-0011-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-006-0011-2