Abstract
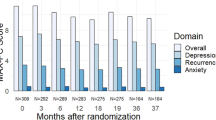
Our study aimed to detect the longitudinal prevalence of anxiety and depression in prostate cancer survivors post-resection and their risk factors. A total of 169 prostate cancer patients who underwent resection were included and followed up for 3 years. Then anxiety and depression were assessed by Zung’s Self-rating Anxiety Scale (SAS) or Zung’s Self-rating Depression Scale (SDS) from the day of discharging from hospital to the last follow up every 3 months. Overall survival (OS) was calculated and documented. In prostate cancer survivors post-resection, the SAS score, anxiety occurrence rate, SDS score and depression occurrence rate all gradually elevated from baseline to month 36. Multivariate logistic regression analysis disclosed that age ≥ 65 years, education duration<9 years, marry status of single/divorced/widowed, unemployment before surgery, diabetes, and hyperlipidemia, higher Gleason score, higher pathological T stage, higher pathological N stage, positive surgical margin status were independent factors related to higher anxiety risk in the 3 years follow-up duration. Additionally, unemployment before surgery, hyperlipidemia, higher pathological T stage, higher pathological N stage, positive surgical margin status were independently associated with depression risk in the 3 years follow-up duration. In addition, baseline anxiety, baseline depression, 1-year depression and 2-year depression associated with worse OS. In conclusion, post-resection anxiety and depression continuously worsen in prostate cancer survivors, and age, marriage status, education duration, complications, and tumor features can serve as their risk factors.


Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Litwin MS, Tan HJ. The diagnosis and treatment of prostate Cancer: a review. JAMA. 2017;317(24):2532–42. https://doi.org/10.1001/jama.2017.7248.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. https://doi.org/10.3322/caac.21492.
Ding T, Wang X, Fu A, Xu L, Lin J. Anxiety and depression predict unfavorable survival in acute myeloid leukemia patients. Medicine (Baltimore). 2019;98(43):e17314. https://doi.org/10.1097/MD.0000000000017314.
Valderrama Rios MC, Sanchez PR. Anxiety and depression disorders in relation to the quality of life of breast Cancer patients with locally advanced or disseminated stage. Rev Colomb Psiquiatr. 2018;47(4):211–20. https://doi.org/10.1016/j.rcp.2017.04.003.
Lardas M, Liew M, van den Bergh RC, De Santis M, Bellmunt J, Van den Broeck T, et al. Quality of life outcomes after primary treatment for clinically localised prostate Cancer: a systematic review. Eur Urol. 2017;72(6):869–85. https://doi.org/10.1016/j.eururo.2017.06.035.
Hughes S, Egger S, Carle C, Smith DP, Chambers S, Kahn C, et al. Factors associated with the use of diet and the use of exercise for prostate cancer by long-term survivors. PLoS One. 2019;14(10):e0223407. https://doi.org/10.1371/journal.pone.0223407.
Craske MG, Stein MB. Anxiety. Anxiety Lancet. 2016;388(10063):3048–59. https://doi.org/10.1016/S0140-6736(16)30381-6.
Malhi GS, Mann JJ. Depression. Depression Lancet. 2018;392(10161):2299–312. https://doi.org/10.1016/S0140-6736(18)31948-2.
Mitchell AJ, Chan M, Bhatti H, Halton M, Grassi L, Johansen C, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. 2011;12(2):160–74. https://doi.org/10.1016/S1470-2045(11)70002-X.
Cheng Y, Gao XH, Li XJ, Cao QH, Zhao DD, Zhou JR, et al. Depression promotes prostate cancer invasion and metastasis via a sympathetic-cAMP-FAK signaling pathway. Oncogene. 2018;37(22):2953–66. https://doi.org/10.1038/s41388-018-0177-4.
Chien CH, Chuang CK, Liu KL, Pang ST, Wu CT, Chang YH. Prostate cancer-specific anxiety and the resulting health-related quality of life in couples. J Adv Nurs. 2019;75(1):63–74. https://doi.org/10.1111/jan.13828.
Zung WW. A self-rating depression scale. Arch Gen Psychiatry. 1965;12:63–70. https://doi.org/10.1001/archpsyc.1965.01720310065008.
Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12(6):371–9. https://doi.org/10.1016/S0033-3182(71)71479-0.
Wang G, Gislum M, Filippov G, Montgomery S. Comparison of vortioxetine versus venlafaxine XR in adults in Asia with major depressive disorder: a randomized, double-blind study. Curr Med Res Opin. 2015;31(4):785–94. https://doi.org/10.1185/03007995.2015.1014028.
Jimenez-Fonseca P, Calderon C, Hernandez R, Ramon YCT, Mut M, Ramchandani A, et al. Factors associated with anxiety and depression in cancer patients prior to initiating adjuvant therapy. Clin Transl Oncol. 2018;20(11):1408–15. https://doi.org/10.1007/s12094-018-1873-9.
Unseld M, Krammer K, Lubowitzki S, Jachs M, Baumann L, Vyssoki B, et al. Screening for post-traumatic stress disorders in 1017 cancer patients and correlation with anxiety, depression, and distress. Psychooncology. 2019;28(12):2382–8. https://doi.org/10.1002/pon.5239.
Sfanos KS, Yegnasubramanian S, Nelson WG, De Marzo AM. The inflammatory microenvironment and microbiome in prostate cancer development. Nat Rev Urol. 2018;15(1):11–24. https://doi.org/10.1038/nrurol.2017.167.
Peirce JM, Alvina K. The role of inflammation and the gut microbiome in depression and anxiety. J Neurosci Res. 2019;97(10):1223–41. https://doi.org/10.1002/jnr.24476.
Holmes SE, Hinz R, Conen S, Gregory CJ, Matthews JC, Anton-Rodriguez JM, et al. Elevated Translocator protein in anterior cingulate in major depression and a role for inflammation in suicidal thinking: a positron emission tomography study. Biol Psychiatry. 2018;83(1):61–9. https://doi.org/10.1016/j.biopsych.2017.08.005.
Felger JC, Li Z, Haroon E, Woolwine BJ, Jung MY, Hu X, et al. Inflammation is associated with decreased functional connectivity within corticostriatal reward circuitry in depression. Mol Psychiatry. 2016;21(10):1358–65. https://doi.org/10.1038/mp.2015.168.
Liu H, Yang L. Dynamic change of depression and anxiety after chemotherapy among patients with ovarian cancer. Medicine (Baltimore). 2019;98(31):e16620. https://doi.org/10.1097/MD.0000000000016620.
Park S, Kang CH, Hwang Y, Seong YW, Lee HJ, Park IK, et al. Risk factors for postoperative anxiety and depression after surgical treatment for lung cancerdagger. Eur J Cardiothorac Surg. 2016;49(1):e16–21. https://doi.org/10.1093/ejcts/ezv336.
Abad VC, Guilleminault C. Insomnia in elderly patients: recommendations for pharmacological management. Drugs Aging. 2018;35(9):791–817. https://doi.org/10.1007/s40266-018-0569-8.
Yu J, Rawtaer I, Fam J, Jiang MJ, Feng L, Kua EH, et al. Sleep correlates of depression and anxiety in an elderly Asian population. Psychogeriatrics. 2016;16(3):191–5. https://doi.org/10.1111/psyg.12138.
Apryatin SA, Sidorova YS, Shipelin VA, Balakina A, Trusov NV, Mazo VK. Neuromotor activity, anxiety and cognitive function in the in vivo model of alimentary hyperlipidemia and obesity. Bull Exp Biol Med. 2017;163(1):37–41. https://doi.org/10.1007/s10517-017-3732-z.
Moulton CD, Pickup JC, Ismail K. The link between depression and diabetes: the search for shared mechanisms. Lancet Diabetes Endocrinol. 2015;3(6):461–71. https://doi.org/10.1016/S2213-8587(15)00134-5.
Kumar M, Chail M. Sucrose and saccharin differentially modulate depression and anxiety-like behavior in diabetic mice: exposures and withdrawal effects. Psychopharmacology. 2019;236(11):3095–110. https://doi.org/10.1007/s00213-019-05259-3.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Consent for Publication
Not Applicable.
Conflict of Interest
The authors declare that they have no conflict of interest.
Research Involving Human Participants
The Institutional Review Board of our hospital approved this study.
Informed Consent
Patients signed written informed consents before enrollment.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yu, R., Li, H. Longitudinal Assessment of Prevalence and Risk Factors of Anxiety and Depression among Prostate Cancer Survivors Post-Resection. Psychiatr Q 92, 995–1009 (2021). https://doi.org/10.1007/s11126-020-09869-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11126-020-09869-5