Abstract
Objective
To develop machine learning (ML) models that predict postoperative remission, remission at last visit, and resistance to somatostatin receptor ligands (SRL) in patients with acromegaly and to determine the clinical features associated with the prognosis.
Methods
We studied outcomes using the area under the receiver operating characteristics (AUROC) values, which were reported as the performance metric. To determine the importance of each feature and easy interpretation, Shapley Additive explanations (SHAP) values, which help explain the outputs of ML models, are used.
Results
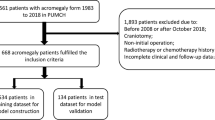
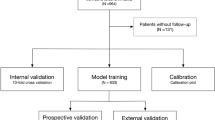
One-hundred fifty-two patients with acromegaly were included in the final analysis. The mean AUROC values resulting from 100 independent replications were 0.728 for postoperative 3 months remission status classification, 0.879 for remission at last visit classification, and 0.753 for SRL resistance status classification. Extreme gradient boosting model demonstrated that preoperative growth hormone (GH) level, age at operation, and preoperative tumor size were the most important predictors for early remission; resistance to SRL and preoperative tumor size represented the most important predictors of remission at last visit, and postoperative 3-month insulin-like growth factor 1 (IGF1) and GH levels (random and nadir) together with the sparsely granulated somatotroph adenoma subtype served as the most important predictors of SRL resistance.
Conclusions
ML models may serve as valuable tools in the prediction of remission and SRL resistance.



Similar content being viewed by others
References
Melmed S (2009) Acromegaly pathogenesis and treatment. J Clin Invest 119(11):3189–3202 Epub 2009/11/04. doi: https://doi.org/10.1172/jci39375. PubMed PMID: 19884662; PubMed Central PMCID: PMCPMC2769196.
Colao A, Ferone D, Marzullo P, Lombardi G (2004) Systemic complications of acromegaly: epidemiology, pathogenesis, and management. Endocr Rev 25(1):102–152
Sherlock M, Ayuk J, Tomlinson JW, Toogood AA, Aragon-Alonso A, Sheppard MC et al (2010) Mortality in patients with pituitary disease. Endocr Rev 31(3):301–342
Renehan AG, O’Connell J, O’Halloran D, Shanahan F, Potten CS, O’Dwyer ST et al (2003) Acromegaly and colorectal cancer: a comprehensive review of epidemiology, biological mechanisms, and clinical implications. Horm Metab Res 35(11/12):712–725
Babu H, Ortega A, Nuno M, Dehghan A, Schweitzer A, Bonert HV et al (2017) Long-term endocrine outcomes following endoscopic endonasal transsphenoidal surgery for acromegaly and associated prognostic factors. Neurosurgery 81(2):357–366
Shimon I, Cohen ZR, Ram Z, Hadani M (2001) Transsphenoidal surgery for acromegaly: endocrinological follow-up of 98 patients. Neurosurgery 48(6):1239–1245
Aydin S, Ozoner B, Sahin S, Alizada O, Comunoglu N, Oz B et al (2020) A follow-up study on outcomes of endoscopic transsphenoidal approach for acromegaly. Clin Neurol Neurosurg 198:106201 Epub 2020/09/15. doi: https://doi.org/10.1016/j.clineuro.2020.106201. PubMed PMID: 32927330.
Haliloglu O, Kuruoglu E, Ozkaya HM, Keskin FE, Gunaldi O, Oz B et al (2016) Multidisciplinary Approach for Acromegaly: A Single Tertiary Center’s Experience. World Neurosurg 88:270–276 Epub 2016/01/26. doi: https://doi.org/10.1016/j.wneu.2015.12.092. PubMed PMID: 26806060.
Briceno V, Zaidi HA, Doucette JA, Onomichi KB, Alreshidi A, Mekary RA et al (2017) Efficacy of transsphenoidal surgery in achieving biochemical cure of growth hormone-secreting pituitary adenomas among patients with cavernous sinus invasion: a systematic review and meta-analysis. Neurol Res 39(5):387–398
Jane JA Jr, Starke RM, Elzoghby MA, Reames DL, Payne SC, Thorner MO et al (2011) Endoscopic transsphenoidal surgery for acromegaly: remission using modern criteria, complications, and predictors of outcome. J Clin Endocrinol Metabolism 96(9):2732–2740
Sun H, Brzana J, Yedinak CG, Gultekin SH, Delashaw JB, Fleseriu M (2014) Factors associated with biochemical remission after microscopic transsphenoidal surgery for acromegaly. J Neurol Surg Part B: Skull Base 75(01):047–52
Petrossians P, Borges-Martins L, Espinoza C, Daly A, Betea D, Valdes-Socin H et al (2005) Gross total resection or debulking of pituitary adenomas improves hormonal control of acromegaly by somatostatin analogs. Eur J Endocrinol 152(1):61–66
Kiseljak-Vassiliades K, Carlson NE, Borges MT, Kleinschmidt-DeMasters B, Lillehei KO, Kerr JM et al (2015) Growth hormone tumor histological subtypes predict response to surgical and medical therapy. Endocrine 49(1):231–241
Heck A, Ringstad G, Fougner SL, Casar-Borota O, Nome T, Ramm‐Pettersen J et al (2012) Intensity of pituitary adenoma on T2‐weighted magnetic resonance imaging predicts the response to octreotide treatment in newly diagnosed acromegaly. Clin Endocrinol 77(1):72–78
Nomikos P, Buchfelder M, Fahlbusch R (2005) The outcome of surgery in 668 patients with acromegaly using current criteria of biochemical ‘cure’. Eur J Endocrinol 152(3):379–387
Ahmed S, Elsheikh M, Stratton I, Page R, Adams C, Wass J (1999) Outcome of transphenoidal surgery for acromegaly and its relationship to surgical experience. Clin Endocrinol 50(5):561–567
Shen M, Zhang Q, Liu W, Wang M, Zhu J, Ma Z et al (2016) Predictive value of T2 relative signal intensity for response to somatostatin analogs in newly diagnosed acromegaly. Neuroradiology 58(11):1057–1065
van Bunderen CC, van Varsseveld NC, Baayen JC, van Furth WR, Aliaga ES, Hazewinkel MJ et al (2013) Predictors of endoscopic transsphenoidal surgery outcome in acromegaly: patient and tumor characteristics evaluated by magnetic resonance imaging. Pituitary 16(2):158–167
Mazal P, Czech T, Sedivy R, Aichholzer M, Wanschitz J, Klupp N et al (2001) Prognostic relevance of intracytoplasmic cytokeratin pattern, hormone expression profile, and cell proliferation in pituitary adenomas of akromegalic patients. Clin Neuropathol 20(4):163–171
Bakhtiar Y, Hirano H, Arita K, Yunoue S, Fujio S, Tominaga A et al (2010) Relationship between cytokeratin staining patterns and clinico-pathological features in somatotropinomae. Eur J Endocrinol 163(4):531
Bourdelot A, Coste J, Hazebroucq V, Gaillard S, Cazabat L, Bertagna X et al (2004) Clinical, hormonal and magnetic resonance imaging (MRI) predictors of transsphenoidal surgery outcome in acromegaly. Eur J Endocrinol 150(6):763–771
Starke RM, Raper DM, Payne SC, Vance ML, Oldfield EH, Jane JA Jr (2013) Endoscopic vs microsurgical transsphenoidal surgery for acromegaly: outcomes in a concurrent series of patients using modern criteria for remission. J Clin Endocrinol Metabolism 98(8):3190–3198
Antunes X, Ventura N, Camilo GB, Wildemberg LE, Guasti A, Pereira PJM et al (2018) Predictors of surgical outcome and early criteria of remission in acromegaly. Endocrine 60(3):415–422
Abosch A, Tyrrell JB, Lamborn KR, Hannegan LT, Applebury CB, Wilson CB (1998) Transsphenoidal microsurgery for growth hormone-secreting pituitary adenomas: initial outcome and long-term results. J Clin Endocrinol Metabolism 83(10):3411–3418
Shirvani M, Motiei-Langroudi R (2014) Transsphenoidal surgery for growth hormone–secreting pituitary adenomas in 130 patients. World Neurosurg 81(1):125–130
Kovacs K, Horvath E (1986) Pathology of growth hormone-producing tumors of the human pituitary. Semin Diagn Pathol 3(1):18–33 Epub 1986/02/01. PubMed PMID: 3303228
Krieger MD, Couldwell WT, Weiss MH (2003) Assessment of long-term remission of acromegaly following surgery. J Neurosurg 98(4):719–724
Dutta P, Korbonits M, Sachdeva N, Gupta P, Srinivasan A, Devgun JS et al (2016) Can immediate postoperative random growth hormone levels predict long-term cure in patients with acromegaly? Neurology India 64(2):252–8
Feelders R, Bidlingmaier M, Strasburger C, Janssen J, Uitterlinden P, Hofland L et al (2005) Postoperative evaluation of patients with acromegaly: clinical significance and timing of oral glucose tolerance testing and measurement of (free) insulin-like growth factor I, acid-labile subunit, and growth hormone-binding protein levels. J Clin Endocrinol Metabolism 90(12):6480–6489
Hazer DB, Işık S, Berker D, Güler S, Gürlek A, Yücel T et al (2013) Treatment of acromegaly by endoscopic transsphenoidal surgery: surgical experience in 214 cases and cure rates according to current consensus criteria. J Neurosurg 119(6):1467–1477
Cleophas TJ (2016) Machine learning in therapeutic research: the hard work of outlier detection in large data. Am J Ther 23(3):e837–e43
Hollon TC, Parikh A, Pandian B, Tarpeh J, Orringer DA, Barkan AL et al (2018) A machine learning approach to predict early outcomes after pituitary adenoma surgery. NeuroSurg Focus 45(5):E8
Staartjes VE, Serra C, Muscas G, Maldaner N, Akeret K, van Niftrik CH et al (2018) Utility of deep neural networks in predicting gross-total resection after transsphenoidal surgery for pituitary adenoma: a pilot study. NeuroSurg Focus 45(5):E12
Fan Y, Li Y, Li Y, Feng S, Bao X, Feng M et al (2020) Development and assessment of machine learning algorithms for predicting remission after transsphenoidal surgery among patients with acromegaly. Endocrine 67(2):412–422
Dai C, Fan Y, Li Y, Bao X, Li Y, Su M et al (2020) Development and interpretation of multiple machine learning models for predicting postoperative delayed remission of acromegaly patients during long-term follow-up.Frontiers in endocrinology. 2020;11:643.
Qiao N, Shen M, He W, He M, Zhang Z, Ye H et al (2021) Machine learning in predicting early remission in patients after surgical treatment of acromegaly: a multicenter study. Pituitary 24(1):53–61
Katznelson L, Laws ER Jr, Melmed S, Molitch ME, Murad MH, Utz A et al (2014) Acromegaly: an endocrine society clinical practice guideline. J Clin Endocrinol Metabolism 99(11):3933–3951
Katznelson L, Laws ER Jr, Melmed S, Molitch ME, Murad MH, Utz A et al (2014) Acromegaly: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metabolism 99(11):3933–3951. doi: https://doi.org/10.1210/jc.2014-2700
Lombardi G, Colao A, Marzullo P, Biondi B, Palmieri E, Fazio S (2002) Improvement of left ventricular hypertrophy and arrhythmias after lanreotide-induced GH and IGF-I decrease in acromegaly. A prospective multi-center study. J Endocrinol Invest 25(11):971–976 Epub 2003/01/30. doi: https://doi.org/10.1007/bf03344070. PubMed PMID: 12553557.
Polat Korkmaz O, Gurcan M, Nuhoglu Kantarci FE, Haliloglu O, Ozkaya HM, Sahin S et al (2019) The effects of pre-operative somatostatin analogue therapy on treatment cost and remission in acromegaly. Pituitary 22(4):387–396 Epub 2019/05/18. doi: https://doi.org/10.1007/s11102-019-00968-6. PubMed PMID: 31098838.
Giustina A, Chanson P, Kleinberg D, Bronstein MD, Clemmons DR, Klibanski A et al (2014) Expert consensus document: a consensus on the medical treatment of acromegaly. Nat Reviews Endocrinol 10(4):243–248
Colao A, Auriemma RS, Lombardi G, Pivonello R (2011) Resistance to somatostatin analogs in acromegaly. Endocr Rev 32(2):247–271
Chen T, editor Guestrin C, Mining D (2016) (KDD’16);
Du M, Liu N, Hu X (2019) Techniques for interpretable machine learning. Commun ACM 63(1):68–77
Minniti G, Jaffrain-Rea M, Esposito V, Santoro A, Tamburrano G, Cantore G (2003) Evolving criteria for post-operative biochemical remission of acromegaly: can we achieve a definitive cure? An audit of surgical results on a large series and a review of the literature. Endocrine-related Cancer 10(4):611–619
Araujo-Castro M, Pascual-Corrales E, Martínez-Vaello V, Baonza Saiz G, Quiñones de Silva J, Acitores Cancela A et al (2021) Predictive model of surgical remission in acromegaly: age, presurgical GH levels and Knosp grade as the best predictors of surgical remission. J Endocrinol Investig 44:183–193
Asha MJ, Takami H, Velasquez C, Oswari S, Almeida JP, Zadeh G et al (2019) Long-term outcomes of transsphenoidal surgery for management of growth hormone–secreting adenomas: single-center results. J Neurosurg 133(5):1360–1370
Fusco A, Zatelli MC, Bianchi A, Cimino V, Tilaro L, Veltri F et al (2008) Prognostic significance of the Ki-67 labeling index in growth hormone-secreting pituitary adenomas. J Clin Endocrinol Metabolism 93(7):2746–2750
Wang M, Mou C, Jiang M, Han L, Fan S, Huan C et al (2012) The characteristics of acromegalic patients with hyperprolactinemia and the differences in patients with merely GH-secreting adenomas: clinical analysis of 279 cases. Eur J Endocrinol 166(5):797–802
Rick J, Jahangiri A, Flanigan PM, Chandra A, Kunwar S, Blevins L et al (2018) Growth hormone and prolactin-staining tumors causing acromegaly: a retrospective review of clinical presentations and surgical outcomes. J Neurosurg 131(1):147–153
Park SH, Ku CR, Moon JH, Kim EH, Kim SH, Lee EJ (2018) Age-and sex-specific differences as predictors of surgical remission among patients with acromegaly. J Clin Endocrinol Metabolism 103(3):909–916
Albarel F, Castinetti F, Morange I, Conte-Devolx B, Gaudart J, Dufour H et al (2013) Outcome of multimodal therapy in operated acromegalic patients, a study in 115 patients. Clin Endocrinol 78(2):263–270
Cuevas-Ramos D, Fleseriu M (2014) Somatostatin receptor ligands and resistance to treatment in pituitary adenomas. J Mol Endocrinol 52(3):R223–R40
Brzana J, Yedinak CG, Gultekin SH, Delashaw JB, Fleseriu M (2013) Growth hormone granulation pattern and somatostatin receptor subtype 2A correlate with postoperative somatostatin receptor ligand response in acromegaly: a large single center experience. Pituitary 16(4):490–498
Gadelha MR, Kasuki L, Korbonits M (2013) Novel pathway for somatostatin analogs in patients with acromegaly. Trends in Endocrinology & Metabolism 24(5):238–246
Wildemberg LE, da Silva Camacho AH, Miranda RL, Elias PC, de Castro Musolino NR, Nazato D et al (2021) Machine learning-based prediction model for treatment of acromegaly with first-generation somatostatin receptor ligands. J Clin Endocrinol Metabolism 106(7):2047–2056
Schwyzer L, Starke RM, Jane JA Jr, Oldfield EH (2015) Percent reduction of growth hormone levels correlates closely with percent resected tumor volume in acromegaly. J Neurosurg 122(4):798–802 Epub 2014/11/26. doi: https://doi.org/10.3171/2014.10.Jns14496. PubMed PMID: 25423276.
Melmed S (2006) Acromegaly. New England. J Med 355(24):2558–2573
Ben-Shlomo A, Schmid H, Wawrowsky K, Pichurin O, Hubina E, Chesnokova V et al (2009) Differential ligand-mediated pituitary somatostatin receptor subtype signaling: implications for corticotroph tumor therapy. J Clin Endocrinol Metabolism 94(11):4342–4350
Liu Y, Liu X, Hong X, Liu P, Bao X, Yao Y et al (2019) Prediction of recurrence after transsphenoidal surgery for Cushing’s disease: the use of machine learning algorithms. Neuroendocrinology 108(3):201–210
Wang X, Wang D, Yao Z, Xin B, Wang B, Lan C et al (2019) Machine learning models for multiparametric glioma grading with quantitative result interpretations. Front NeuroSci 12:1046
Lundberg SM, Lee S-I (eds) (2017) Proceedings of the 31st international conference on neural information processing systems;
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to conception and design, and/or acquisition of data, and/or analysis and interpretation of data; participated in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Disclosure Statement
The authors have nothing to disclose. Cem Sulu and Ayyüce Begüm Bektaş have equally contributed to this article.
Ethical approval
All procedures performed in studies involving human participants were in accordance with ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all living individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sulu, C., Bektaş, A.B., Şahin, S. et al. Machine learning as a clinical decision support tool for patients with acromegaly. Pituitary 25, 486–495 (2022). https://doi.org/10.1007/s11102-022-01216-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-022-01216-0