Abstract
Purpose
Transsphenoidal surgery (TSS) is the first-line treatment for patients with Cushing’s Disease (CD). Recurrence rates after a first TSS range between 3 and 22% within 3 years. Management of recurrent or persistent CD may include repeat TSS or stereotactic radiosurgery (SRS). We performed a meta-analysis to explore the overall efficacy of TSS and SRS for patients with CD after an initial surgical intervention.
Methods
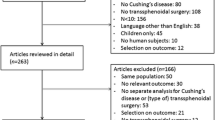
EMBASE, PubMed, SCOPUS, and Cochrane databases were searched from their dates-of-inception up to December 2021. Inclusion criteria were comprised of patients with an established diagnosis of CD who presented with persistent or biochemically recurrent disease after a first TSS for tumor resection and were treated with a second TSS or SRS.
Results
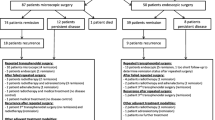
Search criteria yielded 2,116 studies of which 37 articles from 15 countries were included for analysis. Mean age ranged between 29.9 and 47.9 years, and mean follow-up was 11–104 months. TSS was used in 669 (67.7%) patients, while SRS was used in 320 (32.4%) patients, and remission rates for CD were 59% (95%CI 0.49–0.68) and 74% (95%CI 0.54–0.88), respectively. There was no statistically significant difference in the remission rate between TSS and SRS (P = 0.15). The remission rate of patients with recurrent CD undergoing TSS was 53% (95%CI 0.32–0.73), and for persistent CD was 41% (95%CI 0.28–0.56) (P = 0.36).
Conclusion
Both TSS and SRS are possible approaches for the treatment of recurrent or persistent CD after a first TSS. Our data show that either TSS or SRS represent viable treatment options to achieve remission for this subset of patients.




Similar content being viewed by others
References
Fleseriu M, Auchus R, Bancos I, Ben-Shlomo A, Bertherat J, Biermasz NR et al (2021) Consensus on diagnosis and management of Cushing’s disease: a guideline update. Lancet Diabetes Endocrinol 9(12):847–875
Fleseriu M, Hamrahian AH, Hoffman AR, Kelly DF, Katznelson L (2016) American Association of clinical endocrinologists and American College of Endocrinology disease state clinical review: diagnosis of recurrence in cushing disease. Endocr Pract 22(12):1436–1448
Hofmann BM, Hlavac M, Martinez R, Buchfelder M, Müller OA, Fahlbusch R (2008) Long-term results after microsurgery for Cushing disease: experience with 426 primary operations over 35 years. J Neurosurg 108(1):9–18
Valassi E, Biller BM, Swearingen B, Pecori Giraldi F, Losa M, Mortini P et al (2010) Delayed remission after transsphenoidal surgery in patients with Cushing’s disease. J Clin Endocrinol Metab 95(2):601–610
Tritos NA, Biller BM, Swearingen B (2011) Management of Cushing disease. Nat Rev Endocrinol 7(5):279–289
Patil CG, Veeravagu A, Prevedello DM, Katznelson L, Vance ML, Laws ER, Jr (2008) Outcomes after repeat transsphenoidal surgery for recurrent Cushing's disease. Neurosurgery 63(2):266–270; discussion 70–71.
Chee GH, Mathias DB, James RA, Kendall-Taylor P (2001) Transsphenoidal pituitary surgery in Cushing’s disease: can we predict outcome? Clin Endocrinol (Oxf) 54(5):617–626
Hofmann BM, Hlavac M, Kreutzer J, Grabenbauer G, Fahlbusch R (2006) Surgical treatment of recurrent Cushing's disease. Neurosurgery 58(6):1108–1118; discussion -18.
Hughes JD, Young WF, Chang AY, Link MJ, Garces YI, Laack NN et al (2020) Radiosurgical management of patients with persistent or recurrent cushing disease after prior transsphenoidal surgery: a management algorithm based on a 25-year experience. Neurosurgery 86(4):557–564
Yuen KCJ (2021) Osilodrostat: a review of recent clinical studies and practical recommendations for its use in the treatment of Cushing disease. Endocr Pract 27(9):956–965
Truong HL, Nellesen D, Ludlam WH, Neary MP (2014) Budget impact of pasireotide for the treatment of Cushing’s disease, a rare endocrine disorder associated with considerable comorbidities. J Med Econ 17(4):288–295
Moher D, Liberati A, Tetzlaff J, Altman DG (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8(5):336–341
Wagenmakers MA, Netea-Maier RT, van Lindert EJ, Timmers HJ, Grotenhuis JA, Hermus AR (2009) Repeated transsphenoidal pituitary surgery (TS) via the endoscopic technique: a good therapeutic option for recurrent or persistent Cushing’s disease (CD). Clin Endocrinol (Oxf) 70(2):274–280
Netea-Maier RT, van Lindert EJ, den Heijer M, van der Eerden A, Pieters GF, Sweep CG et al (2006) Transsphenoidal pituitary surgery via the endoscopic technique: results in 35 consecutive patients with Cushing’s disease. Eur J Endocrinol 154(5):675–684
Locatelli M, Vance ML, Laws ER (2005) Clinical review: the strategy of immediate reoperation for transsphenoidal surgery for Cushing’s disease. J Clin Endocrinol Metab 90(9):5478–5482
Feng M, Liu Z, Liu X, Bao X, Yao Y, Deng K et al (2018) Diagnosis and outcomes of 341 patients with Cushing’s disease following transsphenoid surgery: a single-center experience. World Neurosurg 109:e75–e80
Serban AL, Del Sindaco G, Sala E, Carosi G, Indirli R, Rodari G et al (2020) Determinants of outcome of transsphenoidal surgery for Cushing disease in a single-centre series. J Endocrinol Invest 43(5):631–639
Bodaghabadi M, Riazi H, Aran S, Bitaraf MA, Alikhani M, Alahverdi M et al (2014) Repeated transsphenoidal surgery or gamma knife radiosurgery in recurrent cushing disease after transsphenoidal surgery. J Neurol Surg A Cent Eur Neurosurg 75(2):91–97
Kara M, Güdük M, Samanci Y, Yilmaz M, Şengöz M, Peker S (2020) Gamma knife radiosurgery in patients with Cushing’s disease: comparison of aggressive pituitary corticotroph tumor versus corticotroph adenoma. Clin Neurol Neurosurg 197:106151
Pollock BE, Brown PD, Nippoldt TB, Young WF Jr (2008) Pituitary tumor type affects the chance of biochemical remission after radiosurgery of hormone-secreting pituitary adenomas. Neurosurgery 62(6):1271–1276
Sheehan JP, Xu Z, Salvetti DJ, Schmitt PJ, Vance ML (2013) Results of gamma knife surgery for Cushing’s disease: clinical article. J Neurosurg 119(6):1486–1492
Trifiletti DM, Xu Z, Dutta SW, Quiñones-Hinojosa A, Peterson J, Vance ML et al (2018) Endocrine remission after pituitary stereotactic radiosurgery: differences in rates of response for matched cohorts of cushing disease and acromegaly patients. Int J Radiat Oncol Biol Phys 101(3):610–617
Moore JM, Sala E, Amorin A, Martinez H Jr, Bhowmik AC, Chang SD et al (2018) CyberKnife radiosurgery in the multimodal management of patients with cushing disease. World Neurosurg 112:e425–e430
Petit JH, Biller BM, Yock TI, Swearingen B, Coen JJ, Chapman P et al (2008) Proton stereotactic radiotherapy for persistent adrenocorticotropin-producing adenomas. J Clin Endocrinol Metab 93(2):393–399
Hofmann BM, Fahlbusch R (2006) Treatment of Cushing's disease: a retrospective clinical study of the latest 100 cases. In: Laws Jr ER, Sheehan JP, editors. Front Hormone Res 158–184
Dimopoulou C, Schopohl J, Rachinger W, Buchfelder M, Honegger J, Reincke M et al (2014) Long-term remission and recurrence rates after first and second transsphenoidal surgery for Cushing’s disease: care reality in the Munich Metropolitan Region. Eur J Endocrinol 170(2):283–292
Burke WT, Penn DL, Repetti CS, Iuliano S, Laws ER (2019) Outcomes after repeat transsphenoidal surgery for recurrent Cushing disease: updated. Neurosurgery 85(6):E1030–E1036
Almeida JP, de Andrade E, Reghin-Neto M, Radovanovic I, Recinos PF, Kshettry VR. From above and below: the microsurgical anatomy of endoscopic endonasal and transcranial microsurgical approaches to the parasellar region. World Neurosurg 2021.
Sheehan JM, Vance ML, Sheehan JP, Ellegala DB, Laws ER Jr (2000) Radiosurgery for Cushing’s disease after failed transsphenoidal surgery. J Neurosurg 93(5):738–742
Espinosa-de-Los-Monteros AL, Sosa-Eroza E, Espinosa E, Mendoza V, Arreola R, Mercado M (2017) Long-term outcome of the different treatment alternatives for recurrent and persistent Cushing disease. Endocr Pract 23(7):759–767
Alahmadi H, Cusimano MD, Woo K et al (2013) Impact of technique on cushing disease outcome using strict remission criteria. Can J Neurol Sci 40(3):334–341
Benveniste RJ, King WA, Walsh J, Lee JS, Delman BN, Post KD (2005) Repeated transsphenoidal surgery to treat recurrent or residual pituitary adenoma. J Neurosurg 102(6):1004–1012
Brichard C, Costa E, Fomekong E, Maiter D, Raftopoulos C (2018) Outcome of transsphenoidal surgery for Cushing disease: a single-center experience over 20 years. World Neurosurg 119:e106–e117
Blevins LS Jr, Christy JH, Khajavi M, Tindall GT (1998) Outcomes of therapy for Cushing’s disease due to adrenocorticotropin-secreting pituitary macroadenomas. J Clin Endocrinol Metab 83(1):63–67
Carroll TB, Javorsky BR, Findling JW (2016) Postsurgical recurrent cushing disease: clinical benefit of early intervention in patients with normal urinary free cortisol. Endocr Pract 22(10):1216–1223
Dai C, Liang S, Liu X et al (2020) Outcomes of transsphenoidal surgery in cushing disease patients with negative pituitary magnetic resonance imaging findings: a single-center experience. Endocr Pract 26(11):1320–1330
Fomekong E, Maiter D, Grandin C, Raftopoulos C (2009) Outcome of transsphenoidal surgery for Cushing’s disease: a high remission rate in ACTH-secreting macroadenomas. Clin Neurol Neurosurg 111(5):442–449
Friedman RB, Oldfield EH, Nieman LK et al (1989) Repeat transsphenoidal surgery for Cushing’s disease. J Neurosurg 71(4):520–527
Hameed N, Yedinak CG, Brzana J et al (2013) Remission rate after transsphenoidal surgery in patients with pathologically confirmed Cushing’s disease, the role of cortisol, ACTH assessment and immediate reoperation: a large single center experience. Pituitary 16(4):452–458
Honegger J, Schmalisch K, Beuschlein F et al (2012) Contemporary microsurgical concept for the treatment of Cushing’s disease: endocrine outcome in 83 consecutive patients. Clin Endocrinol (Oxf) 76(4):560–567
Liu X, Dai C, Bao X et al (2021) Treatment and outcomes of recurrent/persistent Cushing’s disease: a single-center experience. Ann Palliat Med 10(3):2494–2504
Martinez Ortega AJ, Venegas-Moreno E, Dios E et al (2019) Surgical outcomes and comorbidities in Cushing disease: 30 years of experience in a referral center. World Neurosurgery 122:e436–e442
Mayberg M, Reintjes S, Patel A et al (2018) Dynamics of postoperative serum cortisol after transsphenoidal surgery for Cushing’s disease: implications for immediate reoperation and remission. J Neurosurg 129(5):1268–1277
Ram Z, Nieman LK, Cutler GB Jr, Chrousos GP, Doppman JL, Oldfield EH (1994) Early repeat surgery for persistent Cushing’s disease. J Neurosurg 80(1):37–45
Rollin G, Ferreira NP, Czepielewski MA (2007) Prospective evaluation of transsphenoidal pituitary surgery in 108 patients with Cushing’s disease. Arq Bras Endocrinol Metabol 51(8):1355–1361
Shimon I, Ram Z, Cohen ZR, Hadani M (2002) Transsphenoidal surgery for Cushing's disease: endocrinological follow-up monitoring of 82 patients. Neurosurgery 51(1):57–61; discussion 61–52.
Shirvani M, Motiei-Langroudi R, Sadeghian H (2016) Outcome of microscopic transsphenoidal surgery in Cushing disease: a case series of 96 patients. World Neurosurg 87:170–175
Valderrábano P, Aller J, García-Valdecasas L et al (2014) Results of repeated transsphenoidal surgery in Cushing’s disease Long-term follow-up. Endocrinol Nutr 61(4):176–183
Funding
No funding was provided to conduct the study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study. Conceptualization and design were performed by CPV, and SLS. Data collection and analysis were performed by CPV, ARF, ST, and RAD. The first draft of the manuscript was written by CPV, and SLS. Review and editing of the manuscript were performed by SLS, KR, JPA, JP, DMT, KLC, AQH. All authors read and approved the final manuscript for submission.
Corresponding author
Ethics declarations
Conflict of interest
Susan L. Samson has been a site principal investigator for clinical trials involving patients with Cushing’s disease for Novartis and Corcept. The remaining authors have no relevant financial or non-financial interest to disclose.
Ethical approval
This is a meta-analysis; no ethical approval or informed consent was required by the institutional review board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Perez-Vega, C., Ramos-Fresnedo, A., Tripathi, S. et al. Treatment of recurrent and persistent Cushing’s disease after first transsphenoidal surgery: lessons learned from an international meta-analysis. Pituitary 25, 540–549 (2022). https://doi.org/10.1007/s11102-022-01215-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-022-01215-1