Abstract
Purpose
To evaluate the association between acromegaly and pregnancy in terms of disease activity, maternal and fetal outcomes.
Methods
This systematic review was conducted according to the Joanna Briggs Institute methodology for systematic reviews of etiology and risk. We focused on observational studies that included pregnant women with acromegaly. The outcomes were acromegaly activity, preterm birth, gestational diabetes, hypertension, eclampsia/preeclampsia, miscarriage, perinatal mortality, low birthweight, small for gestational age, and congenital malformations. Embase, Medline, LILACS, and CENTRAL were our source databases. To perform proportional meta-analyses, we used Stata Statistical Software 17.
Results
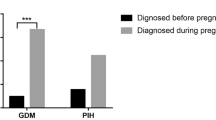
Nineteen studies were included encompassing a total of 273 pregnancies in 211 women with acromegaly. The overall frequency of control of acromegaly during pregnancy was 62%, and of tumor growth was 9%. No fetal or maternal deaths were reported. The overall frequency of worsening of previous diabetes or development of gestational diabetes was 9%, and of previous hypertension or preeclampsia/eclampsia was 6%. The overall frequency of premature labor was 9% [from 17 studies of 263 pregnancies; 95% confidence interval (CI), 5–13%]; of spontaneous miscarriage was 4% (from 19 studies of 273 pregnancies; 95% CI, 2–11%); of small for gestational age was 5% (from 15 studies of 216 newborns; 95% CI, 3–9%); and of congenital malformations was 1% (from 18 studies of 240 newborns; 95% CI, 0–7%).
Conclusion
Pregnancy in women with acromegaly is frequently associated with disease control and is safe in relation to fetal and maternal outcomes, as in women without acromegaly.




Similar content being viewed by others
References
Grynberg M, Salenave S, Young J, Chanson P (2010) Female gonadal function before and after treatment of acromegaly. J Clin Endocrinol Metab 95(10):4518–4525
Caron P, Broussaud S, Bertherat J, Borson-Chazot F, Brue T, Cortet-Rudelli C, Chanson P (2010) Acromegaly and pregnancy: a retrospective multicenter study of 59 pregnancies in 46 women. J Clin Endocrinol Metab 95(10):4680–4687
Caron P (2011) Acromegaly and pregnancy. Ann Endocrinol 72(4):282–286
Goluboff LG, Ezrin C (1969) Effect of pregnancy on the somatotroph and the prolactin cell of the human adenohypophysis. J Clin Endocrinol Metab 29(12):1533–1538
Montini M, Pagani G, Gianola D, Pagani MD, Piolini R, Camboni MG (1990) Acromegaly and primary amenorrhea: ovulation and pregnancy induced by SMS 201–995 and bromocriptine. J Endocrinol Invest 13(2):193
Hannon AM, O’Shea T, Thompson CA, Hannon MJ, Dineen R, Khattak A, Gibney J, O’Halloran DJ, Hunter S, Thompson CJ, Sherlock M (2019) Pregnancy in acromegaly is safe and is associated with improvements in IGF-1 concentrations. Eur J Endocrinol 180(4):K21–K29
Dias M, Boguszewski C, Gadelha M, Kasuki L, Musolino N, Vieira JG, Abucham J (2014) Acromegaly and pregnancy: a prospective study. Eur J Endocrinol 170(2):301–310
Jallad RS, Shimon I, Fraenkel M, Medvedovsky V, Akirov A, Duarte FH, Bronstein MD (2018) Outcome of pregnancies in a large cohort of women with acromegaly. Clin Endocrinol (Oxf) 88(6):896–907
Chanson P, Vialon M, Caron P (2019) An update on clinical care for pregnant women with acromegaly. Expert Rev Endocrinol Metab 14(2):85–96
Moola SMZ, Tufanaru C, Aromataris E, Sears K, Sfetcu R et al (2017) Chapter 7: systematic reviews of etiology and risk. In: Aromataris E, Munn Z (eds) Joanna Briggs Institute Reviewer’s Manual. The Joanna Briggs Institute, Adelaide
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med 151(4):W65-94
Bandeira DB, Olivatti TOF, Bolfi F, Boguszewski CL, dos Santos Nunes-Nogueira V (2020) Acromegaly and pregnancy: a systematic review protocol. Asian J Adv Res Rep 14(4):5
Katznelson L, Laws ER Jr, Melmed S, Molitch ME, Murad MH, Utz A, Wass JA, Endocrine S (2014) Acromegaly: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 99(11):3933–3951
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan—a web and mobile app for systematic reviews. Syst Rev 5(1):210
Munn ZBT, Moola S, Tufanaru C, Stern C, McArthur A, Stephenson M, Aromataris E (2020) Methodological quality of case series studies. JBI Evid Synth 18(10):2127–2133
Riley RD, Higgins JP, Deeks JJ (2011) Interpretation of random effects meta-analyses. BMJ (Clin Res Ed) 342:d549
Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, Vist GE, Falck-Ytter Y, Meerpohl J, Norris S, Guyatt GH (2011) GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 64(4):401–406
Assal A, Malcolm J, Lochnan H, Keely E (2016) Preconception counselling for women with acromegaly: more questions than answers. Obstet Med 9(1):9–14
Atmaca A, Dagdelen S, Erbas T (2006) Follow-up of pregnancy in acromegalic women: different presentations and outcomes. Exp Clin Endocrinol Diabetes 114(3):135–139
Cheng V, Faiman C, Kennedy L, Khoury F, Hatipoglu B, Weil R, Hamrahian A (2012) Pregnancy and acromegaly: a review. Pituitary 15(1):59–63
Cozzi R, Attanasio R, Barausse M (2006) Pregnancy in acromegaly: a one-center experience. Eur J Endocrinol 155(2):279–284
Dias M, Bouszewski C, Gadelha M, Kasuki L, Musolino N, Vieira JGH, Abucham J (2014) Acromegaly and pregnancy: a prospective study. Eur J Endocrinol 170(2):301–310
Dogansen SC, Tanrikulu S, Yalin GY, Yarman S (2018) Female gonadal functions and ovarian reserve in patients with acromegaly: experience from a single tertiary center. Endocrine 60(1):167–174
Guitelman MA, Tkatch J, Rosmino J, Pingel J (2018) Acromegaly: a single center retrospective study of 11 pregnancies. Endocr Rev 39(2)
Haliloglu O, Dogangun B, Ozcabi B, Kural HU, Keskin FE, Ozkaya HM, Pamukcu FC, Bektas E, Poyraz BC, Buber H, Evliyaoglu O, Kadioglu P (2016) General health status and intelligence scores of children of mothers with acromegaly do not differ from those of healthy mothers. Pituitary 19(4):391–398
Herman-Bonert V, Seliverstov M, Melmed S (1998) Pregnancy in acromegaly: successful therapeutic outcome. J Clin Endocrinol Metab 83(3):727–731
Karaca Z, Yarman S, Ozbas I, Kadioglu P, Akturk M, Kilicli F, Dokmetas HS, Colak R, Atmaca H, Canturk Z, Altuntas Y, Ozbey N, Hatipoglu N, Tanriverdi F, Unluhizarci K, Kelestimur F (2018) How does pregnancy affect the patients with pituitary adenomas: a study on 113 pregnancies from Turkey. J Endocrinol Invest 41(1):129–141
Guarda FJ, Gong W, Ghajar A, Guitelman M, Nachtigall LB (2020) Preconception use of pegvisomant alone or as combination therapy for acromegaly: a case series and review of the literature. Pituitary 23(5):498–506
Önder E, Aydın Y, Soysal T, Tuna M, Güngör A (2017) Acromegaly and pregnancy: five new cases. Akromegali ve gebelik: beş yeni vaka. Turk J Endocrinol Metab 21(4):136–139
Persechini ML, Gennero I, Grunenwald S, Vezzosi D, Bennet A, Caron P (2014) Acromegaly and pregnancy: report of six new cases. J Gynecol Obstet Biol Reprod 43(9):704–712
Van Der Lely AJ, Gomez R, Heissler JF, Åkerblad AC, Jönsson P, Camacho-Hübner C, Kołtowska-Häggström M (2014) Pregnancy in acromegaly patients treated with pegvisomant. Growth Hormon IGF Res 24:S40
Vialon M, Grunenwald S, Mouly C, Vezzosi D, Bennet A, Gourdy P, Caron PJ (2019) Gestational diabetes and acromegaly: single-centre experience of 14 pregnancies. Clin Endocrinol (Oxf) 91(6):805–809
Colao A, Merola B, Ferone D, Lombardi G (1997) Acromegaly. J Clin Endocrinol Metab 82(9):2777–2781
Andreeva M, Tomova A, Shterev A (1990) Acromegaly and pregnancy. Vutr Boles 29(1):94–99
Rees K, Lambert K, Seed P, Dhanjal MK, Knight M, McCance DR, Williamson C (2016) Pituitary tumours in pregnancy: a 3-year prospective UK national cohort study. BJOG Int J Obstet Gynaecol 123:19
Lambert K, Rees K, Seed PT, Dhanjal MK, Knight M, McCance DR, Williamson C (2017) Macroprolactinomas and nonfunctioning pituitary adenomas and pregnancy outcomes. Obstet Gynecol 129(1):185–194
Muhammad A, Neggers SJ, van der Lely AJ (2017) Pregnancy and acromegaly. Pituitary 20(1):179–184
Abucham J, Bronstein MD, Dias ML (2017) Acromegaly and pregnancy: a contemporary review. Eur J Endocrinol 177(1):R1–R12
Marques JVO, Boguszewski CL (2020) Fertility issues in aggressive pituitary tumors. Rev Endocr Metab Disord 21(2):225–233
Davenport ML, Clemmons DR, Miles MV, Camacho-Hubner C, D’Ercole AJ, Underwood LE (1990) Regulation of serum insulin-like growth factor-I (IGF-I) and IGF binding proteins during rat pregnancy. Endocrinology 127(3):1278–1286
Han VK, Carter AM (2000) Spatial and temporal patterns of expression of messenger RNA for insulin-like growth factors and their binding proteins in the placenta of man and laboratory animals. Placenta 21(4):289–305
Nayak NR, Giudice LC (2003) Comparative biology of the IGF system in endometrium, decidua, and placenta, and clinical implications for foetal growth and implantation disorders. Placenta 24(4):281–296
Wiesli P, Zwimpfer C, Zapf J, Schmid C (2006) Pregnancy-induced changes in insulin-like growth factor I (IGF-I), insulin-like growth factor binding protein 3 (IGFBP-3), and acid-labile subunit (ALS) in patients with growth hormone (GH) deficiency and excess. Acta Obstet Gynecol Scand 85(8):900–905
Leung KC, Johannsson G, Leong GM, Ho KK (2004) Estrogen regulation of growth hormone action. Endocr Rev 25(5):693–721
Alexopoulou O, Bex M, Kamenicky P, Mvoula AB, Chanson P, Maiter D (2014) Prevalence and risk factors of impaired glucose tolerance and diabetes mellitus at diagnosis of acromegaly: a study in 148 patients. Pituitary 17(1):81–89
Petrossians P, Daly AF, Natchev E, Maione L, Blijdorp K, Sahnoun-Fathallah M, Auriemma R, Diallo AM, Hulting AL, Ferone D, Hana V Jr, Filipponi S, Sievers C, Nogueira C, Fajardo-Montanana C, Carvalho D, Hana V, Stalla GK, Jaffrain-Rea ML, Delemer B, Colao A, Brue T, Neggers S, Zacharieva S, Chanson P, Beckers A (2017) Acromegaly at diagnosis in 3173 patients from the Liege Acromegaly Survey (LAS) Database. Endocr Relat Cancer 24(10):505–518
Federation ID (2019) IDF diabetes atlas ninth. IDF, Dunia
Vila G, Luger A, van der Lely AJ, Neggers S, Webb SM, Biller BMK, Valluri S, Hey-Hadavi J (2020) Hypertension in acromegaly in relationship to biochemical control and mortality: global ACROSTUDY outcomes. Front Endocrinol (Lausanne) 11:577173
Butwick AJ, Druzin ML, Shaw GM, Guo N (2020) Evaluation of US State-level variation in hypertensive disorders of pregnancy. JAMA Netw Open 3(10):e2018741
Berhe AK, Kassa GM, Fekadu GA, Muche AA (2018) Prevalence of hypertensive disorders of pregnancy in Ethiopia: a systemic review and meta-analysis. BMC Pregnancy Childbirth 18(1):34
Wang X, Chen C, Wang L, Chen D, Guang W, French J (2003) Conception, early pregnancy loss, and time to clinical pregnancy: a population-based prospective study. Fertil Steril 79(3):577–584
Walani SR (2020) Global burden of preterm birth. Int J Gynaecol Obstet Off Organ Int Federation Gynaecol Obstet 150(1):31–33
Black RE (2015) Global prevalence of small for gestational age births. Nestle Nutr Inst Workshop Ser 81:1–7
Ruiz M, Goldblatt P, Morrison J, Kukla L, Svancara J, Riitta-Jarvelin M, Taanila A, Saurel-Cubizolles MJ, Lioret S, Bakoula C, Veltsista A, Porta D, Forastiere F, van Eijsden M, Vrijkotte TG, Eggesbo M, White RA, Barros H, Correia S, Vrijheid M, Torrent M, Rebagliato M, Larranaga I, Ludvigsson J, Olsen Faresjo A, Hryhorczuk D, Antipkin Y, Marmot M, Pikhart H (2015) Mother’s education and the risk of preterm and small for gestational age birth: a DRIVERS meta-analysis of 12 European cohorts. J Epidemiol Community Health 69(9):826–833
Dolk H, Loane M, Garne E (2010) The prevalence of congenital anomalies in Europe. Adv Exp Med Biol 686:349–364
Funding
This research was partially supported by the São Paulo Research Foundation (FAPESP) (Grant No. 2020/04818-1).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors have declared that no competing interests exist.
Ethical approval
As no primary data collection was undertaken, no formal ethical assessment is required in our institution.
Research involving human and animal rights
This study does not involve human participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bandeira, D.B., Olivatti, T.O.F., Bolfi, F. et al. Acromegaly and pregnancy: a systematic review and meta-analysis. Pituitary 25, 352–362 (2022). https://doi.org/10.1007/s11102-022-01208-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-022-01208-0