Abstract
Purpose
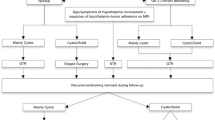
Patients suffering from craniopharyngiomas currently have good survival rates, but long-term sequelae, such as development of obesity, worsen their quality of life. Optimal treatment is still controversial and changed during the decades, becoming less aggressive. Transcranial (TC) surgery was the first approach to be used, followed by extended transsphenoidal (eTNS) access. This study aims to compare the two approaches in terms of risk of hypothalamic damage leading to obesity.
Methods
This is a monocentric retrospective analysis of post-puberal patients treated for primary craniopharyngioma. Postoperative obesity and percentual postsurgical BMI variation were considered proxy for hypothalamic function and used to fit regression models with basal BMI, type of surgery, tumor volume and hypothalamic involvement (anterior vs. anteroposterior).
Results
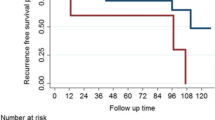
No difference in radicality was observed between the two approaches; eTNS was more effective in ameliorating visual function but was significantly associated with CSF leaks. The TC approach was associated with a higher incidence of diabetes insipidus. Regression analysis showed only tumor volume and basal BMI resulted as independent predictors for both postoperative obesity (respectively, OR 1.15, P = 0.041, and OR 1.57, P < 0.001) and percentual BMI variation (respectively, + 0.92%, P = 0.005, and − 1.49%, P = 0.001).
Conclusions
Larger lesions portend a higher risk to develop postoperative obesity, independently of hypothalamic involvement. Interestingly, basal BMI is independent of lesional volume and is associated with postoperative obesity, but lesser postoperative BMI variation. The surgical approach does not influence the obesity risk. However, eTNS proves valid in managing large tumors with important hypothalamic invasion.




Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study are secured in the institution archive and are available from the corresponding author on reasonable request.
Code availability
The R code scripts used for the current study analyses are available from the corresponding author on reasonable request.
References
Honegger J, Tatagiba M (2008) Craniopharyngioma surgery. Pituitary 11:361–373. https://doi.org/10.1007/s11102-008-0137-z
Rickert CH, Paulus W (2001) Epidemiology of central nervous system tumors in childhood and adolescence based on the new WHO classification. Child’s Nerv Syst 17:503–511. https://doi.org/10.1007/s003810100496
Mortini P (2017) Craniopharyngiomas: a life-changing tumor. Endocrine 57:191–192. https://doi.org/10.1007/s12020-016-1192-2
Mortini P, Losa M, Pozzobon G et al (2011) Neurosurgical treatment of craniopharyngioma in adults and children: early and long-term results in a large case series—clinical article. J Neurosurg 114:1350–1359. https://doi.org/10.3171/2010.11.JNS10670
Buchfelder M, Schlaffer SM, Lin F, Kleindienst A (2013) Surgery for craniopharyngioma. Pituitary 16:18–25. https://doi.org/10.1007/s11102-012-0414-8
Mortini P, Gagliardi F, Boari N, Losa M (2013) Surgical strategies and modern therapeutic options in the treatment of craniopharyngiomas. Crit Rev Oncol Hematol 88:514–529. https://doi.org/10.1016/j.critrevonc.2013.07.013
Alli S, Isik S, Rutka JT (2016) Microsurgical removal of craniopharyngioma: endoscopic and transcranial techniques for complication avoidance. J Neurooncol 130:299–307. https://doi.org/10.1007/s11060-016-2147-4
Chakrabarti I, Amar AP, Couldwell W, Weiss MH (2005) Long-term neurological, visual, and endocrine outcomes following transnasal resection of craniopharyngioma. J Neurosurg 102:650–657. https://doi.org/10.3171/jns.2005.102.4.0650
Zacharia BE, Amine M, Anand V, Schwartz TH (2016) Endoscopic endonasal management of craniopharyngioma. Otolaryngol Clin North Am 49:201–212. https://doi.org/10.1016/j.otc.2015.09.013
Jeon C, Kim S, Shin HJ et al (2011) The therapeutic efficacy of fractionated radiotherapy and gamma-knife radiosurgery for craniopharyngiomas. J Clin Neurosci 18:1621–1625. https://doi.org/10.1016/j.jocn.2011.03.028
Yang I, Sughrue ME, Rutkowski MJ et al (2010) Craniopharyngioma: a comparison of tumor control with various treatment strategies. Neurosurg Focus 28:1–11. https://doi.org/10.3171/2010.1.FOCUS09307
Maira G, Anile C, Rossi GF, Colosimo C (1995) Surgical treatment of craniopharyngiomas: an evaluation of the transsphenoidal and pterional approaches. Neurosurgery 36:715–724
Evans J, Kenning T (2014) Craniopharyngiomas: comprehensive diagnosis, treatment and outcome, 6th edn. Elsevier, Oxford
Flitsch J, Aberle J, Burkhardt T (2015) Surgery for pediatric craniopharyngiomas: is less more? J Pediatr Endocrinol Metab 28:27–33. https://doi.org/10.1515/jpem-2014-0417
Abe T, Lüdecke DK (1999) Transnasal surgery for infradiaphragmatic craniopharyngiomas in pediatric patients. Neurosurgery 44:957–964
Weiss MH, Apuzzo MJL (1987) The transnasal transsphenoidal approach. Williams & Wilkins, Baltimore
Kato T, Sawamura Y, Abe H, Nagashima M (1998) Transsphenoidal-transtuberculum sellae approach for supradiaphragmatic tumours: technical note. Acta Neurochir (Wien) 140:715–719. https://doi.org/10.1007/s007010050167
Laufer I, Anand VK, Schwartz TH (2007) Endoscopic, endonasal extended transsphenoidal, transplanum transtuberculum approach for resection of suprasellar lesions. J Neurosurg 106:400–406. https://doi.org/10.3171/jns.2007.106.3.400
Gardner PA, Kassam AB, Snyderman CH et al (2008) Outcomes following endoscopic, expanded endonasal resection of suprasellar craniopharyngiomas: a case series. J Neurosurg 109:6–16. https://doi.org/10.3171/JNS/2008/109/7/0006
Couldwell WT, Weiss MH, Rabb C et al (2004) Variations on the standard transsphenoidal approach to the sellar region, with emphasis on the extended approaches and parasellar approaches: surgical experience in 105 cases. Neurosurgery 55:539–547. https://doi.org/10.1227/01.NEU.0000134287.19377.A2
Maira G, Anile C, Albanese A et al (2004) The role of transsphenoidal surgery in the treatment of craniopharyngiomas. J Neurosurg 100:445–451. https://doi.org/10.3171/jns.2004.100.3.0445
Müller HL, Reichel J, Boekhoff S et al (2018) Low concordance between surgical and radiological assessment of degree of resection and treatment-related hypothalamic damage: results of KRANIOPHARYNGEOM 2007. Pituitary 21:371–378. https://doi.org/10.1007/s11102-018-0883-5
Müller HL, Gebhardt U, Teske C et al (2011) Post-operative hypothalamic lesions and obesity in childhood craniopharyngioma: results of the multinational prospective trial KRANIOPHARYNGEOM 2000 after 3-year follow-up. Eur J Endocrinol 165:17–24. https://doi.org/10.1530/EJE-11-0158
Van Gompel JJ, Nippoldt TB, Higgins DM, Meyer FB (2010) Magnetic resonance imaging-graded hypothalamic compression in surgically treated adult craniopharyngiomas determining postoperative obesity. Neurosurg Focus 28:1–8. https://doi.org/10.3171/2010.1.FOCUS09303
Cohen LE (2016) Update on childhood craniopharyngiomas. Curr Opin Endocrinol Diabetes Obes 23:339–344. https://doi.org/10.1097/MED.0000000000000264
Müller HL (2015) Craniopharyngioma: long-term consequences of a chronic disease. Expert Rev Neurother 15:1241–1244. https://doi.org/10.1586/14737175.2015.1100078
Bogusz A, Boekhoff S, Warmuth-Metz M et al (2019) Posterior hypothalamus-sparing surgery improves outcome after childhood craniopharyngioma. Endocr Connect 8:481–492. https://doi.org/10.1530/ec-19-0074
Müller HL (2011) Consequences of craniopharyngioma surgery in children. J Clin Endocrinol Metab 96:1981–1991. https://doi.org/10.1210/jc.2011-0174
Fahlbusch R, Honegger J, Paulus W et al (1999) Surgical treatment of craniopharyngiomas: experience with 168 patients. J Neurosurg 90:237–250. https://doi.org/10.3171/jns.1999.90.2.0237
Di Rocco C, Caldarelli M, Tamburrini G, Massimi L (2006) Surgical management of craniopharyngiomas–experience with a pediatric series. J Pediatr Endocrinol Metab 19(Suppl):1
Van Effenterre R, Boch AL (2002) Craniopharyngioma in adults and children: a study of 122 surgical cases. J Neurosurg 97:3–11. https://doi.org/10.3171/jns.2002.97.1.0003
Pierre-Kahn A, Recassens C, Pinto G et al (2005) Social and psycho-intellectual outcome following radical removal of craniopharyngiomas in childhood. A prospective series. Child’s Nerv Syst 21:817–824. https://doi.org/10.1007/s00381-005-1205-6
Morisako H, Goto T, Goto H et al (2016) Aggressive surgery based on an anatomical subclassification of craniopharyngiomas. Neurosurg Focus 41:1–15. https://doi.org/10.3171/2016.9.FOCUS16211
Müller HL, Faldum A, Etavard-Gorris N et al (2003) Functional capacity, obesity and hypothalamic involvement: cross-sectional study on 212 patients with childhood craniopharyngioma. Klin Padiatr 215:310–314
Hofmann BM, Höllig A, Strauss C et al (2012) Results after treatment of craniopharyngiomas: further experiences with 73 patients since 1997. Clinical article. J Neurosurg 116:373–384. https://doi.org/10.3171/2011.6.JNS081451
Hoffmann A, Boekhoff S, Gebhardt U et al (2015) History before diagnosis in childhood craniopharyngioma: associations with initial presentation and long-term prognosis. Eur J Endocrinol 173:853–862. https://doi.org/10.1530/EJE-15-0709
Vinchon M, Weill J, Delestret I, Dhellemmes P (2009) Craniopharyngioma and hypothalamic obesity in children. Child’s Nerv Syst 25:347–352. https://doi.org/10.1007/s00381-008-0754-x
van Iersel L, Meijneke RWH, Schouten-van Meeteren AYN et al (2018) The development of hypothalamic obesity in craniopharyngioma patients: a risk factor analysis in a well-defined cohort. Pediatr Blood Cancer 65:1–9. https://doi.org/10.1002/pbc.26911
Zhang Y, Wang J, Zhang G et al (2015) The neurobiological drive for overeating implicated in Prader-Willi syndrome. Brain Res 1620:72–80. https://doi.org/10.1016/j.brainres.2015.05.008
Müller HL, Gebhardt U, Etavard-Gorris N et al (2004) Prognosis and sequela in patients with childhood craniopharyngioma—results of HIT-ENDO and update on KRANIOPHARYNGEOM 2000. Klin Padiatr 216:343–348
Wannemuehler TJ, Rubel KE, Hendricks BK et al (2016) Outcomes in transcranial microsurgery versus extended endoscopic endonasal approach for primary resection of adult craniopharyngiomas. Neurosurg Focus. https://doi.org/10.3171/2016.9.FOCUS16314
Funding
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
Conceptualization: ALG, LRB, ML; Methodology: ALG, LRB, ML; Formal analysis and investigation: ALG; Writing—original draft preparation: ALG; Writing—review and editing: ALG, LRB, ML, MM, LA, FG, PM; Supervision: PM.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
This type of study does not require specific consent for data publication; however all participants signed a general consent to publish results obtained from studies involving their data.
Ethical approval
This is an observational study. The Vita-Salute University, I.R.C.C.S. San Raffaele Scientific Institute Research Ethics Committee has confirmed that no ethical approval is required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gallotti, A.L., Barzaghi, L.R., Albano, L. et al. Comparison between extended transsphenoidal and transcranial surgery for craniopharyngioma: focus on hypothalamic function and obesity. Pituitary 25, 74–84 (2022). https://doi.org/10.1007/s11102-021-01171-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-021-01171-2