Abstract
Purpose
Hypothalamic-pituitary axis dysfunction and mass effect symptoms in the pediatric population can indicate a pituitary region tumor. Herein, we evaluate the epidemiology and management of this rare entity.
Methods
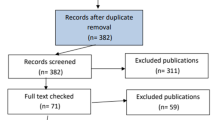
Pediatric patients (≤ 21yo) who presented from 2004 to 2017 with a pituitary tumor were evaluated from the U.S. National Cancer Database. The distributions and management patterns of pituitary tumors were assessed by patients’ tumor type, age, sex, race/ethnicity, tumor size, and insurance status.
Results
19.7% of intracranial tumors in the pediatric population originated in the pituitary region. 7653 pediatric patients with pituitary region tumors were identified, 68.2% of whom were female, with the tumors predominantly occurring in early adolescence (46.9%) and late adolescence (34.8%). The majority of pediatric pituitary region tumors were pituitary adenomas (77.9%), followed by craniopharyngiomas (18.1%) and germ cell tumors (1.6%). Girls demonstrated higher proportions of pituitary adenomas across all ages than boys. Asian/Pacific Islander patients were independently more likely to present at younger ages (mean 13.9yrs) and with germ cell tumors than patients of other races/ethnicities. Only 5.5% of patients were uninsured (referent), but they were independently more likely to present at older ages (mean 17.9yrs) and less likely to undergo surgery than patients with private insurance (OR = 1.93, 95% CI = 1.47–2.52, p < 0.001) or Medicaid (OR = 1.51, 95% CI = 1.14–2.00, p = 0.004).
Conclusion
Pituitary region tumors comprise a significant fraction of intracranial pediatric tumors, particularly in adolescent girls. The differential diagnosis of pituitary tumor types differed significantly by patients’ age, sex, and race/ethnicity. Uninsured patients were associated with delays in care and less surgical management.


Similar content being viewed by others
Data availability
The NCDB PUF is available by application from the Commission on Cancer.
References
Jagannathan J, Dumont AS, Jane JA, Laws ER (2005) Pediatric sellar tumors: diagnostic procedures and management. Neurosurg Focus 18:E6
Keil MF, Stratakis CA (2008) Pituitary tumors in childhood: an update in their diagnosis, treatment and molecular genetics. Expert Rev Neurother 8:563–574. https://doi.org/10.1586/14737175.8.4.563
Ostrom QT, Cioffi G, Gittleman H et al (2019) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2012–2016. Neuro Oncol 21:v1–v100. https://doi.org/10.1093/neuonc/noz150
Ostrom QT, de Blank PM, Kruchko C et al (2015) Alex’s lemonade stand foundation infant and childhood primary brain and central nervous system tumors diagnosed in the United States in 2007–2011. Neuro Oncol 16(Suppl 10):x1–x36. https://doi.org/10.1093/neuonc/nou327
Lloyd RV, Osamura RY, Klöppel G et al (2017) WHO classification of tumours of endocrine organs, 4th edn. International Agency for Research on Cancer, Lyon
Kaltsas GA, Kolomodi D, Randeva H, Grossman A (2019) Nonneuroendocrine neoplasms of the pituitary region. J Clin Endocrinol Metab 104:3108–3123. https://doi.org/10.1210/jc.2018-01871
Aghi MK, Chen CC, Fleseriu M et al (2016) Congress of neurological surgeons systematic review and evidence-based guidelines on the management of patients with nonfunctioning pituitary adenomas: executive summary. Neurosurgery 79:521–523. https://doi.org/10.1227/NEU.0000000000001386
Fleseriu M, Biller BMK, Freda PU et al (2020) A pituitary society update to acromegaly management guidelines. Pituitary. https://doi.org/10.1007/s11102-020-01091-7
Boffa DJ, Rosen JE, Mallin K et al (2017) Using the national cancer database for outcomes research: a review. JAMA Oncol 3:1722–1728. https://doi.org/10.1001/jamaoncol.2016.6905
Gupta S, Iorgulescu JB, Hoffman S et al (2020) The diagnosis and management of primary and iatrogenic soft tissue sarcomas of the sella. Pituitary 23:558–572. https://doi.org/10.1007/s11102-020-01062-y
Iorgulescu JB, Torre M, Harary M et al (2019) The misclassification of diffuse gliomas: rates and outcomes. Clin Cancer Res 25:2656–2663. https://doi.org/10.1158/1078-0432.CCR-18-3101
Iorgulescu JB, Harary M, Zogg CK et al (2018) Improved risk-adjusted survival for melanoma brain metastases in the Era of checkpoint blockade immunotherapies: results from a national cohort. Cancer Immunol Res. https://doi.org/10.1158/2326-6066.CIR-18-0067
Ciccarelli A, Daly AF, Beckers A (2005) The epidemiology of prolactinomas. Pituitary 8:3–6. https://doi.org/10.1007/s11102-005-5079-0
Arafah BM, Nasrallah MP (2001) Pituitary tumors: pathophysiology, clinical manifestations and management. Endocr Relat Cancer. https://doi.org/10.1677/erc.0.0080287
Chentli F, Belhimer F, Kessaci F, Mansouri B (2012) Congenital craniopharyngioma: a case report and literature review. J Pediatr Endocrinol Metab 25:1181–1183. https://doi.org/10.1515/jpem-2012-0251
Scagliotti V, Avagliano L, Gualtieri A et al (2016) Histopathology and molecular characterisation of intrauterine-diagnosed congenital craniopharyngioma. Pituitary 19:50–56. https://doi.org/10.1007/s11102-015-0682-1
Kageji T, Miyamoto T, Kotani Y et al (2017) Congenital craniopharyngioma treated by radical surgery: case report and review of the literature. Childs Nerv Syst 33:357–362. https://doi.org/10.1007/s00381-016-3249-1
Jung KW, Ha J, Lee SH et al (2013) An updated nationwide epidemiology of primary brain tumors in republic of Korea. Brain Tumor Res Treat 1:16–23. https://doi.org/10.14791/btrt.2013.1.1.16
Suh Y-L, Koo H, Kim TS et al (2002) Tumors of the central nervous system in Korea: a multicenter study of 3221 cases. J Neuro Oncol 56:251–259. https://doi.org/10.1023/a:1015092501279
Giantini Larsen AM, Cote DJ, Zaidi HA et al (2018) Spindle cell oncocytoma of the pituitary gland. J Neurosurg 131:517–525. https://doi.org/10.3171/2018.4.JNS18211
Saeger W, Lüdecke DK, Buchfelder M et al (2007) Pathohistological classification of pituitary tumors: 10 years of experience with the German pituitary tumor registry. Eur J Endocrinol 156:203–216. https://doi.org/10.1530/eje.1.02326
Acknowledgements
JBI gratefully acknowledges funding support from the National Cancer Institute (K12CA090354) and Conquer Cancer Foundation. LEC acknowledges funding support from the National Institute of Diabetes and Digestive and Kidney (3R01DK119699-01S1). The National Cancer Data Base (NCDB) is a joint project of the Commission on Cancer (CoC) of the American College of Surgeons and the American Cancer Society. The CoC’s NCDB and the hospitals participating in the CoC NCDB are the source of the de-identified data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Funding
This work received no funding support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest.
Ethical approval
This study was approved by the Mass General Brigham institutional review board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Castellanos, L.E., Misra, M., Smith, T.R. et al. The epidemiology and management patterns of pediatric pituitary tumors in the United States. Pituitary 24, 412–419 (2021). https://doi.org/10.1007/s11102-020-01120-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-020-01120-5