Abstract
Purpose
Diabetes insipidus (DI) develops commonly after endoscopic transsphenoidal surgery (ETS). We retrospectively investigated the incidence, onset, duration and predictors of DI after ETS in patients with non-functioning pituitary adenoma (NFPA).
Methods
A total of 168 patients who underwent ETS to remove NFPAs were included. Various perioperative data on demographics, comorbidities, previous treatments, perioperative hormone deficiencies, tumor characteristics, surgery, anesthesia, intraoperative fluid balance, perioperative laboratory findings, postoperative complications, readmission and hospital length of stay were collected and analyzed. Patients were diagnosed with DI and treated with desmopressin when they showed urine output > 5 mL/kg/hr with a serum sodium concentration > 145 mmol/L or an increase ≥ 3 mmol/L in serum sodium concentration between two consecutive tests after surgery. DI was considered permanent when desmopressin was prescribed for > 6 months after surgery.
Results
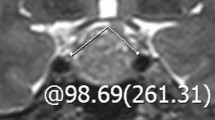
Seventy-seven (45.8%) patients experienced postoperative DI and 10 (6.0%) patients suffered from permanent DI. The median onset of DI and the median duration of transient DI were postoperative day 1 and 5 days, respectively. In multivariable logistic regression analysis, cephalocaudal tumor diameter (odds ratio [95% confidence interval] 2.59 [1.05–6.36], P = 0.038) was related to postoperative DI. In receiver operating characteristic analysis, its area under the curve was 0.68 (95% confidence interval 0.59–0.76, P < 0.001). Its optimal cutoff value that maximized the sum of sensitivity and specificity for postoperative DI was 2.7 cm.
Conclusions
Postoperative DI was observed in 45.8% of patients undergoing ETS to remove NFPAs. A large cephalocaudal tumor diameter was predictive of postoperative DI in such patients.

Similar content being viewed by others
Data availability
The data and materials of this study are available upon request to the corresponding author.
References
Lobatto DJ, de Vries F, Zamanipoor Najafabadi AH, Pereira AM, Peul WC, Vliet Vlieland TPM, Biermasz NR, van Furth WR (2018) Preoperative risk factors for postoperative complications in endoscopic pituitary surgery: a systematic review. Pituitary 21:84–97
Schreckinger M, Szerlip N, Mittal S (2013) Diabetes insipidus following resection of pituitary tumors. Clin Neurol Neurosurg 115:121–126
Seckl J, Dunger D (1989) Postoperative diabetes insipidus. BMJ 298:2–3
Makaryus AN, McFarlane SI (2006) Diabetes insipidus: diagnosis and treatment of a complex disease. Cleve Clin J Med 73:65–71
Sheehan JM, Sheehan JP, Douds GL, Page RB (2006) DDAVP use in patients undergoing transsphenoidal surgery for pituitary adenomas. Acta Neurochir (Wien) 148:287–291
Nayak P, Montaser AS, Hu J, Prevedello DM, Kirschner LS, Ghalib L (2018) Predictors of postoperative diabetes insipidus following endoscopic resection of pituitary adenomas. J Endocr Soc 2:1010–1019
Schreckinger M, Walker B, Knepper J, Hornyak M, Hong D, Kim JM, Folbe A, Guthikonda M, Mittal S, Szerlip NJ (2013) Post-operative diabetes insipidus after endoscopic transsphenoidal surgery. Pituitary 16:445–451
Sigounas DG, Sharpless JL, Cheng DM, Johnson TG, Senior BA, Ewend MG (2008) Predictors and incidence of central diabetes insipidus after endoscopic pituitary surgery. Neurosurgery 62:71–78
Ajlan AM, Abdulqader SB, Achrol AS, Aljamaan Y, Feroze AH, Katznelson L, Harsh GR (2018) Diabetes insipidus following endoscopic transsphenoidal surgery for pituitary adenoma. J Neurol Surg B Skull Base 79:117–122
Chuang CC, Lin SY, Pai PC, Yan JL, Toh CH, Lee ST, Wei KC, Liu ZH, Chen CM, Wang YC, Lee CC (2017) Different volumetric measurement methods for pituitary adenomas and their crucial clinical significance. Sci Rep 7:40792
Kim JH, Lee JH, Lee JH, Hong AR, Kim YJ, Kim YH (2018) Endoscopic transsphenoidal surgery outcomes in 331 nonfunctioning pituitary adenoma cases after a single surgeon learning curve. World Neurosurg 109:e409–e416
Yoon HK, Lee HC, Kim YH, Lim YJ, Park HP (2019) Predictive factors for delayed hyponatremia after endoscopic transsphenoidal surgery in patients with nonfunctioning pituitary tumors: a retrospective observational study. World Neurosurg 122:e1457–e1464
Tape, T.G.: Interpreting Diagnostic Tests. University of Nebraska Medical Center. https://gim.unmc.edu/dxtests/Default.htm (2004). Accessed 15 June 2020
Senior BA, Ebert CS, Bednarski KK, Bassim MK, Younes M, Sigounas D, Ewend MG (2008) Minimally invasive pituitary surgery. Laryngoscope 118:1842–1855
Gubbi S, Hannah-Shmouni F, Koch CA, Verbalis JG (2000) Diagnostic Testing for Diabetes Insipidus. Endotext, South Dartmouth
Arieff AI, Guisado R (1976) Effects on the central nervous system of hypernatremic and hyponatremic states. Kidney Int 10:104–116
Dumont AS, Nemergut EC 2nd, Jane JA Jr, Laws ER Jr (2005) Postoperative care following pituitary surgery. J Intensive Care Med 20:127–140
Seckl JR, Dunger DB, Lightman SL (1987) Neurohypophyseal peptide function during early postoperative diabetes insipidus. Brain 110:737–746
Patel PN, Stafford AM, Patrinely JR, Smith DK, Turner JH, Russell PT, Weaver KD, Chambless LB, Chandra RK (2018) Risk factors for intraoperative and postoperative cerebrospinal fluid leaks in endoscopic transsphenoidal sellar surgery. Otolaryngol Head Neck Surg 158:952–960
Rose SR, Horne VE, Bingham N, Jenkins T, Black J, Inge T (2018) Hypothalamic obesity: 4 years of the international registry of hypothalamic obesity disorders. Obesity (Silver Spring) 26:1727–1732
Steele CA, Cuthbertson DJ, MacFarlane IA, Javadpour M, Das KS, Gilkes C, Wilding JP, Daousi C (2013) Hypothalamic obesity: prevalence, associations and longitudinal trends in weight in a specialist adult neuroendocrine clinic. Eur J Endocrinol 168:501–507
Bokhari AR, Davies MA, Diamond T (2013) Endoscopic transsphenoidal pituitary surgery: a single surgeon experience and the learning curve. Br J Neurosurg 27:44–49
Chi F, Wang Y, Lin Y, Ge J, Qiu Y, Guo L (2013) A learning curve of endoscopic transsphenoidal surgery for pituitary adenoma. J Craniofac Surg 24:2064–2067
Thawani JP, Ramayya AG, Pisapia JM, Abdullah KG, Lee JY, Grady MS (2017) Operative strategies to minimize complications following resection of pituitary macroadenomas. J Neurol Surg B Skull Base 78:184–190
Zhan R, Ma Z, Wang D, Li X (2015) Pure endoscopic endonasal transsphenoidal approach for nonfunctioning pituitary adenomas in the elderly: surgical outcomes and complications in 158 patients. World Neurosurg 84:1572–1578
Vimawala S, Chitguppi C, Reilly E, Fastenberg JH, Garzon-Muvdi T, Farrell C, Rabinowitz MR, Rosen MR, Evans J, Nyquist GG (2020) Predicting prolonged length of stay after endoscopic transsphenoidal surgery for pituitary adenoma. Int Forum Allergy Rhinol 10:785–790
Funding
This study was supported and funded by Seoul National University Hospital (Grant number: 0520200030, recipient: YH Kim).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Institutional Review Board of Seoul National University Hospital approved this study (Number: 2006-128-1133).
Informed consent
The requirement for written informed consent was waived because of the retrospective design of this study by the Institutional Review Board of Seoul National University Hospital.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Oh, H., Cheun, H., Kim, Y.J. et al. Cephalocaudal tumor diameter is a predictor of diabetes insipidus after endoscopic transsphenoidal surgery for non-functioning pituitary adenoma. Pituitary 24, 303–311 (2021). https://doi.org/10.1007/s11102-020-01108-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-020-01108-1