Abstract
Objective
Implication of the tumor size on oncological and functional outcomes of craniopharyngioma is inconsistently reported. The aim of this study is to assess the postoperative outcome of giant craniopharyngiomas (> 4 cm in diameter) and to elucidate the impact of tumor size on various outcome parameters and survival.
Material and methods
Forty-four patients (children aged ≤ 18 years: 25; adults: 16) with giant craniopharyngioma, operated between January 2001 and December 2015, were included in this study. Various outcomes, progression-free survival (PFS) and overall survival (OS) were calculated.
Results
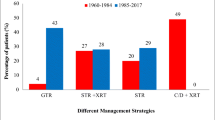
Gross total resection (GTR) was achieved in 17 (39%) and subtotal resection (STR) in 27 (61%) patients. Eleven patients (25%) received radiotherapy (RT) after STR. Postoperatively, new cranial nerve and motor deficits were noted in 12 (27%) and 9 (20%) patients, respectively. Tumor recurrence following GTR and STR without adjuvant RT was diagnosed in 3 (17%), and 5 (38%) patients, respectively. Following STR with RT, one (9%) experienced recurrence. PFS at 5-, and 10- year following GTR, STR, and STR + RT was 80.8%, 45.4%, and 90%, respectively. At 5- and 10- year, OS was 86.5%, 77.9% and 100% following GTR, STR, and STR + RT, respectively. The rate of GTR was significantly lower in patients with giant tumors (39% vs. 62%; Chi-square test, p value 0.008). Postoperatively, neurological deficit (20%), hypopituitarism (95%) and hypothalamic dysfunction (26%) were significantly higher for giant craniopharyngiomas. Hazards of recurrence were not significant between giant and non-giant tumors (hazard ratio 1.86; 95% CI 0.94–3.68; p 0.07). There was no significant difference in OS between the patients with giant and non-giant tumors (log-rank test 2.1; p value 0.14).
Conclusion
Tumor size should be considered as an important predictor of the postoperative functional outcome. Although the rate of GTR is less than that of small tumors, the recurrence rate, progression-free survival, and overall survival of the patients with giant tumor are comparable to non-giant tumors.






Similar content being viewed by others
References
Elliott RE, Wisoff JH (2010) Surgical management of giant pediatric craniopharyngiomas. J Neurosurg Pediatr 6(5):403–416
Eveslage M, Calaminus G, Warmuth-Metz M et al (2019) The postoperative quality of life in children and adolescents with craniopharyngioma—results of a prospective, multicenter study. Dtsch Arztebl Int 116:321–328
Lo AC, Howard AF, Nichol A, Sidhu K, Abdulsatar F, Hasan H, Goddard K (2014) Long-term outcomes and complications in patients with craniopharyngioma: the British Columbia cancer agency experience. Int J Radiat Oncol Biol Phys 88:1011–1018
Müller HL (2015) Craniopharyngioma: long-term consequences of a chronic disease. Expert Rev Neurother 15(11):1241–1244
Erfurth EM, Holmer H, Fjalldal SB (2013) Mortality and morbidity in adult craniopharyngioma. Pituitary 16(1):46–55
Sughrue ME, Yang I, Kane AJ, Fang S, Clark AJ, Aranda D, Barani IJ, Parsa AT (2011) Endocrinologic, neurologic, and visual morbidity after treatment for craniopharyngioma. J Neurooncol 101:463–476
Wijnen M, van den Heuvel-Eibrink MM, Janssen JAMJL, Catsman-Berrevoets CE et al (2017) Very long-term sequelae of craniopharyngioma. Eur J Endocrinol 176(6):755–767
Caldarelli M, Massimi L, Tamburrini G, Cappa M, Di Rocco C (2005) Long-term results of the surgical treatment of craniopharyngioma: the experience at the Policlinico Gemelli, Catholic University, Rome. Childs Nerv Syst 21(8–9):747–757
De Vile CJ, Grant DB, Kendall BE, Neville BG, Stanhope R, Watkins KE et al (1996) Management of childhood craniopharyngioma: can the morbidity of radical surgery be predicted? J Neurosurg 85:73–81
Fischer EG, Welch K, Shillito J Jr, Winston KR, Tarbell NJ (1990) Craniopharyngiomas in children. Long-term effects of conservative surgical procedures combined with radiation therapy. J Neurosurg 73(4):534–540
Karavitaki N, Brufani C, Warner JT, Adams CB, Richards P, Ansorge O, Shine B, Turner HE, Wass JA (2005) Craniopharyngiomas in children and adults: systematic analysis of 121 cases with long-term follow-up. Clin Endocrinol (Oxf) 62(4):397–409
Mortini P, Losa M, Pozzobon G, Barzaghi R, Riva M, Acerno S, Angius D, Weber G, Chiumello G, Giovanelli M (2011) Neurosurgical treatment of craniopharyngioma in adults and children: early and long-term results in a large case series. J Neurosurg 114(5):1350–1359
Schoenfeld A, Pekmezci M, Barnes MJ, Tihan T, Gupta N, Lamborn KR, Banerjee A, Mueller S, Chang S, Berger MS, Haas-Kogan D (2012) The superiority of conservative resection and adjuvant radiation for craniopharyngiomas. J Neurooncol 108(1):133–139
Cohen M, Guger S, Hamilton J (2011) Long term sequelae of pediatric craniopharyngioma - literature review and 20 years of experience. Front Endocrinol (Lausanne) 28(2):81
Kalapurakal JA, Goldman S, Hsieh YC, Tomita T, Marymont MH (2003) Clinical outcome in children with craniopharyngioma treated with primary surgery and radiotherapy deferred until relapse. Med Pediatr Oncol 40:214–218
Jacobsen MF, Thomsen ASS, Bach-Holm D, Doroudian G, Nissen KR, Fugleholm K et al (2018) Predictors of visual outcome in patients operated for craniopharyngioma - a Danish national study. Acta Ophthalmol 96(1):39–45
Kim SK, Wang KC, Shin SH, Choe G, Chi JG, Cho BK (2001) Radical excision of pediatric craniopharyngioma: recurrence pattern and prognostic factors. Child’s Nerv Syst 17:531–536
Van Effenterre R, Boch AL (2002) Craniopharyngioma in adults and children: a study of 122 surgical cases. J Neurosurg 97:3–11
Weiner HL, Wisoff JH, Rosenberg ME, Kupersmith MJ, Cohen H, Zagzag D et al (1994) Craniopharyngiomas: a clinicopathological analysis of factors predictive of recurrence and functional outcome. Neurosurgery 35:1001–1011
Yasargil MG, Curcic M, Kis M, Siegenthaler G, Teddy PJ, Roth P (1990) Total removal of craniopharyngiomas. Approaches and long-term results in 144 patients. J Neurosurg 73:3–11
Gupta DK, Ojha BK, Sarkar C, Mahapatra AK, Mehta VS (2006) Recurrence in craniopharyngiomas: analysis of clinical and histological features. J Clin Neurosci 13(4):438–442
Garg K, Chandra PS, Singh PK, Sharma BS (2013) Giant craniopharyngioma: can it grow bigger than this? Pediatr Neurosurg 49(2):124–125
Trejos H, Caceres A, Segura JL (2005) Monstrous craniopharyngioma. Case presentations and term proposal. Child’s Nerv Syst 21:1049–1053
Fahlbusch R, Hoffman BM (2008) Surgical management of giant craniopharyngiomas. Acta Neurochir 150:1213–1226
Han S, Tie X, Qin X, Wang Y, Wu A (2014) Frontobasal interhemispheric approach for large superasellar craniopharyngiomas: do the benefits outweigh the risks? Acta Neurochir (Wien) 156(1):123–130
Yosef L, Ekkehard KM, Shalom M (2016) Giant craniopharyngiomas in children: short- and long-term implications. Childs Nerv Syst 32(1):79–88
Puget S, Garnett M, Wray A, Grill J, Habrand JL, Bodaert N et al (2007) Pediatric craniopharyngiomas: classification and treatment according to the degree of hypothalamic involvement. J Neurosurg 106:3–12
Wen BC, Hussey DH, Staples J, Hitchon PW, Jani SK, Vigliotti AP et al (1989) A comparison of the roles of surgery and radiation therapy in the management of craniopharyngiomas. Int J Radiat Oncol Biol Phys 16:17–24
Bunin GR, Surawicz TS, Witman PA, Preston-Martin S, Davis F, Bruner JM (1997) The descriptive epidemiology of craniopharyngioma. Neurosurg Focus 3(6):e1
Fahlbusch R, Honegger J, Paulus W, Huk W, Buchfelder M (1999) Surgical treatment of craniopharyngiomas: experience with 168 patients. J Neurosurg 90:237–250
Stripp DC, Maity A, Janss AJ, Belasco JB, Tochner ZA, Goldwein JW, Moshang T, Rorke LB, Phillips PC, Sutton LN, Shu HK (2004) Surgery with or without radiation therapy in the management of craniopharyngiomas in children and young adults. Int J Radiat Oncol Biol Phys 58:714–720
Morisako H, Goto T, Goto H, Bohoun CA, Tamrakar S, Ohata K (2016) Aggressive surgery based on an anatomical subclassification of craniopharyngiomas. Neurosurg Focus 41(6):E10
Zhang YQ, Ma ZY, Wu ZB, Luo SQ, Wang ZC (2008) Radical resection of 202 pediatric craniopharyngiomas with special reference to the surgical approaches and hypothalamic protection. Pediatr Neurosurg 44:435–443
Zuccaro G (2005) Radical resection of craniopharyngioma. Childs Nerv Syst 21(8–9):679–690
Al-Mefty O, Hassounah M, Weaver P, Sakati N, Jinkins JR, Fox JL (1985) Microsurgery for giant craniopharyngiomas in children. Neurosurgery 17:585–595
Ammirati M, Samii M, Sephernias A (1990) Surgery of large retrochiasmatic craniopharyngiomas in children. Childs Nerv Syst 6:13–17
Yang I, Sughrue ME, Rutkowski MJ, Kaur R, Ivan ME, Aranda D, Barani IJ, Parsa AT (2010) Craniopharyngioma: a comparison of tumor control with various treatment strategies. Neurosurg Focus 28(4):E5
Hetelekidis S, Barnes PD, Tao ML, Fischer EG, Schneider L, Scott RM, Tarbell NJ (1993) 20-year experience in childhood craniopharyngioma. Int J Radiat Oncol Biol Phys 27(2):189–195
Shirane R, Ching-Chan S, Kusaka Y, Jokura H, Yoshimoto T (2002) Surgical outcomes in 31 patients with craniopharyngiomas extending outside the suprasellar cistern: an evaluation of the frontobasal interhemispheric approach. J Neurosurg 96(4):704–712
Chargari C, Bauduceau O, Bauduceau B, Camparo P, Ceccaldi B, Fayolle M et al (2007) Craniopharyngiomas: role of radiotherapy. Bull Cancer 94(11):987–994
Sadashivam S, Menon G, Abraham M, Nair SN (2020) Adult craniopharyngioma: the role of extent of resection in tumor recurrence and long-term functional outcome. Clin Neurol Neurosurg 192:105711
Hasegawa T, Kondziolka D, Hadjipanayis CG, Lunsford LD (2004) Management of cystic craniopharyngiomas with phosphorus-32 intracavitary irradiation. Neurosurgery 54(4):813–820
Maarouf M, El Majdoub F, Fuetsch M, Hoevels M, Lehrke R, Berthold F, Voges J, Sturm V (2016) Stereotactic intracavitary brachytherapy with P-32 for cystic craniopharyngiomas in children. Strahlenther Onkol 92(3):157–165
Funding
This is a non-funded study. No funds received from any source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the Institute Ethical Committee (IEC) of Sree Chitra Tirunal Institute for Medical Science and Technology and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Research involving human and animal rights
This article does not contain any studies with animals performed by any of the authors.
Informed consent
This is a retrospective study and data were collected retrospectively from the case files. Patients’ identity revealing details were not included in the study. For this type of study, consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sadhasivam, S., Menon, G., Abraham, M. et al. The implication of giant tumor size on surgical resection, oncological, and functional outcomes in craniopharyngioma. Pituitary 23, 515–525 (2020). https://doi.org/10.1007/s11102-020-01053-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-020-01053-z