Abstract
Background
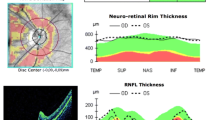
There have been no studies investigating the correlation between structural [thickness of the retinal nerve fiber layer (RNFL) as determined by optical coherence tomography (OCT)] and functional [Humphrey visual field (HVF) or visual evoked potential (VEP) amplitude] measures of optic nerve integrity in patients with pituitary adenomas (PA).
Methods
Patients with PAs were recruited between September 2010 and September 2013. OCT, standard automated perimetry (SAP), and multifical VEP (mfVEP) were performed. Agreement between OCT, SAP, and mfVEP values in classifying eyes/quadrants was determined using AC1 statistics. Pearson’s correlation was used to examine relationships between structural and functional data.
Results
In total, 88.7 % of the eyes tested showed abnormal SAP findings and 93.7 % showed abnormal mfVEP findings. Only 14.8 % of the eyes showed abnormal OCT findings. The agreement between SAP and mfVEP findings was 88.9 % (AC1 = 0.87). The agreement between OCT and mfVEP findings was 24.2 % (AC1 = −0.52), and that between OCT and SAP findings was 21.5 % (AC1 = −0.56). The correlation values between RNFL thickness and the functional measurements were −0.601 for the mfVEP score (P = 0.000) and −0.441 for the SAP score (P = 0.000). The correlation between the mfVEP and SAP scores was −0.617 (P = 0.000).
Conclusions
mfVEP, SAP, and OCT provided complementary information for detecting visual pathway abnormalities in patients with PAs. Good agreement was demonstrated between SAP and mfVEP and quantitative analysis of structure–function measurements revealed a moderate correlation.


Similar content being viewed by others
References
Mete O, Asa SL (2012) Clinicopathological correlations in pituitary adenomas. Brain Pathol 22:443–453
Boonchai W, Vivienne CG, Fabio NK, Tomas MG, Jeffrey ML, Robert R, Donald CH (2009) A method to detect progression of glaucoma using the multifocal visual evoked potential technique. Doc Ophthalmol 118:139–150
Mousa MF, Cubbidge RP, Al-Mansouri F, Bener A (2014) Evaluation of hemifield sector analysis protocol in multifocal visual evoked potential objective perimetry for the diagnosis and early detection of glaucomatous field defects. Korean J Ophthalmol 28(1):49–65
Jayaraman M, Gandhi RA, Ravi P, Sen PL (2014) Multifocal visual evoked potential in optic neuritis, ischemic optic neuropathy and compressive optic neuropathy. Indian J Ophthalmol 62(3):299–304
Brecelj J (2014) Visual electrophysiology in the clinical evaluation of optic neuritis, chiasmal tumours, achiasmia, and ocular albinism: an overview. Doc Ophthalmol 129(2):71–84
Ml Jacob, Raverot G, Jouanneau E, Borson-Chazot F, Perrin G, Rabilloud M, Tilikete C, Bernard M, Vighetto A (2009) Predicting visual outcome after treatment of pituitary adenomas with optical coherence tomography. Am J Ophthalmol 147(1):64–70
Klistorner A, Arvind H, Garrick R, Graham SL, Paine M, Yiannikas C (2010) Interrelationship of optical coherence tomography and multifocal visual-evoked potentials after optic neuritis. Invest Ophthalmol Vis Sci 51(5):2770–2777
Laron M, Cheng H, Zhang B, Schiffman JS, Tang RA, Frishman LJ (2012) Comparison of multifocal visual evoked potential, standard automated perimetry and optical coherence tomography in assessing visual pathway in multiple sclerosis patients. Mult Scler. 16(4):412–426
Garway-Heath DF, Poinoosawny D, Fitzke FW (2000) Mapping the visual field to the optic disc in normal tension glaucoma eyes. Ophthalmology 107(10):1809–1815
Psaras T, Milian M, Hattermann V, Gerlach C, Honegger J (2011) Executive functions recover earlier than episodic memory after microsurgical transsphenoidal resection of pituitary tumors in adult patients: a longitudinal study. J Clin Neurosci. 18(10):1340–1345
Brummelman P, Elderson MF, Dullaart RP, van den Bergh AC, Timmer CA, van den Berg G, Koerts J, Tucha O, Wolffenbuttel BH, van Beek AP (2011) Cognitive functioning in patients treated for nonfunctioning pituitary macroadenoma and the effects of pituitary radiotherapy. Clin Endocrinol (Oxf). 74(4):481–487
Punjabi OS, Stamper RL, Bostrom AG, Han Y, Lin SC (2008) Topographic comparison of the visual function on multifocal visual evoked potentials with optic nerve structure on heidelberg retinal tomography. Ophthalmology 115(3):440–446
Danesh-Meyer HV, Carroll SC, Gaskin BJ, Gao A, Gamble GD (2006) Correlation of the multifocal visual evoked potential and standard automated perimetry in compressive optic neuropathies. Invest Ophthalmol Vis Sci 47(4):1458–1463
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Nidan Qiao and Yichao Zhang have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Qiao, N., Zhang, Y., Ye, Z. et al. Comparison of multifocal visual evoked potential, static automated perimetry, and optical coherence tomography findings for assessing visual pathways in patients with pituitary adenomas. Pituitary 18, 598–603 (2015). https://doi.org/10.1007/s11102-014-0613-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-014-0613-6