Abstract
In recent decades, the therapeutic potential of cannabinoids and analogous compounds has been intensively investigated. The endocannabinoid system has already been identified in the skin and, although much remains to be discovered about its contribution and importance for the maintenance of skin homeostasis, it has been increasingly associated as promising for dermatological disorders’ management. Cannabidiol (CBD), the main non-intoxicating phytocannabinoid in cannabis, has been shown to have hydrating, sebostatic, antipruritic, antimicrobial, anti-inflammatory, antioxidant, wound healing, photoprotective, anti-fibrotic and antitumoral, as well as modulating hair growth. Thus, CBD has gained attention concerning its application in cutaneous pathologies such as atopic dermatitis, psoriasis, acne, epidermolysis bullosa, systemic sclerosis, seborrheic dermatitis, androgenetic alopecia and cutaneous melanoma, although its bioactivities still lack scientific evidence and some of its mechanisms of action remain to be elucidated. Given its physicochemical characteristics, its topical administration becomes challenging, and it is necessary to develop new technological strategies to overcome the skin intact barrier. This review describes the latest evidence that exists on the application of CBD to the skin, the problems inherent to its chemical structure and that compromise its cutaneous administration, and the different strategies and formulations that have been studied to improve it, also clarifying some CBD-containing cosmetics products that are already available on the market.
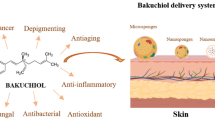
Graphical Abstract

Similar content being viewed by others
Introduction
Cannabis sativa L. plant is a member of the Cannabaceae family (Muscara et al. 2021) that has been used since the beginning of human species evolution (Gallily et al. 2018; Russo 2007). It has several applications, for example, for recreational purposes (Petrocellis et al. 2011), in religious traditions (Pattnaik et al. 2022), as nutrients and other compounds source, and as a natural fiber for textiles (Muscara et al. 2021). Nevertheless, cannabis stands out by its therapeutical applications, mainly for pain relief and in different autoimmune and inflammatory diseases (Gallily et al. 2018). It is also known by its topical uses in skin disorders, such as atopic dermatitis (ATD) (Zeng et al. 2021), psoriasis (Yeroushalmi et al. 2020), eczema, pruritus (Biernacki et al. 2021), skin cancer (Rio et al. 2018a), acne (Olah et al. 2014), skin inflammatory disease (Mugnaini et al. 2019), amongst others. Although delta-9-tetrahydrocannabinol (THC) is the main phytocannabinoid with psychotropic activity (Walsh et al. 2021) cannabidiol (CBD) is the major non-psychoactive one (Blaskovich et al. 2021) found in cannabis. CBD has numerous pharmacological activities and, as it is considered to be safer (Junaid et al. 2022) and to have less potential to induce dependence (Petrocellis et al. 2011), it has been the aim of many pharmaceutical studies for a great number of diseases, including skin-related ones (Blaskovich et al. 2021).
The skin is the largest (Gegotek et al. 2021a) and most external organ of the human body forming the first barrier against chemical, physical and biological agents (Gegotek et al. 2021b). Furthermore, it produces a wide range of molecules like growth factors, neuropeptides, steroids, cytokines, and endocannabinoids (ECs). It also has a complex structure with a developed neuroendocrine (Gegotek et al. 2021a), endocannabinoid (Zakany et al. 2018) and antioxidant systems that contribute to the whole body (Gegotek et al. 2021b) and skin homeostasis (Rio et al. 2018a). The endocannabinoid system (ECS) is a vast signaling system (Bow and Rimoldi 2016) distributed throughout the body, including skin cells and appendages. It comprises the cannabinoid receptor type-1 (CB1R) and cannabinoid receptor type-2 (CB2R), their endogenous ligands (the EC 2-arachidonoylglycerol (2-AG) and N-arachidonoylethanolamine (AEA)) and a variety of enzymes responsible for EC synthesis and degradation (Zakany et al. 2018). It plays an important role in the different cutaneous functions, such as regulation of melanogenesis, immunity responses (Correia-Sa et al. 2020), cell growth and differentiation (Olah et al. 2014), hair growth (Szabo et al. 2020), sebaceous glands production (Zakany et al. 2018), and tissue repair (Ruhl et al. 2021). Hence, any dysregulation or alteration in one or more of its components may trigger a skin condition.
In recent years, CBD has shown excellent results when used in the treatment of several pathologies due to its various biological properties. Additionally, there are already CBD-containing products approved by the Food and Drug Administration (FDA) and European Medicines Agency (EMA) (McGregor et al. 2020). Regarding its application in the skin, several challenges have to be overcome due to its physicochemical characteristics, mainly its high lipophilicity (Momekova et al. 2021).
This review article will describe the different skin biological properties of CBD and the several benefits it has already shown in several emerging skin pathologies. Additionally, different CBD delivery systems and formulation strategies that have been developed, studied, and implemented to improve the delivery of CBD in the skin. Thus, the outcome improvement of its application in different skin diseases will also be discussed.
Cannabidiol
Physicochemical characteristics
CBD is a natural phytocannabinoid whose structure consists of a meroterpenoid of twenty-one carbon atoms (Walsh et al. 2021) with a pentylresorcinol group (Fig. 1). Although its small molecular weight of 3.14 Da is quite favorable, especially for topical administration, its transdermal delivery is compromised and thus poses a challenge due to its extreme lipophilicity characterized by a logP of 5.79 (Junaid et al. 2022). Furthermore, its bioavailability varies not only according to the route of administration, but also to the characteristics of the formulation (Martin et al. 2018). However, it is known that when orally administrated, it exhibits a very low bioavailability since it is highly metabolized by cytochrome P450 (CYP), mostly by CYP3A4 and CYP2C19, in its hydroxylated metabolites (Jiang et al. 2011). Additionally, it shows a high plasma protein binding (> 94%). Altogether, these factors make it a poorly absorbed compound and thus with very low bioavailability (Momekova et al. 2021).
As a cannabinoid, CBD has the ability to not only interact and modulate the ECS in a similar way to EC by binding to its receptors, but it has also been shown that it interacts with several non-CB1R/ non-CB2R (Table 1) (Pattnaik et al. 2022). Generally, but mainly in the skin, CBD shows a negligible binding affinity for both CB1R and CB2R, for which it has proved to be a negative allosteric modulator and an inverse agonist, respectively (Laprairie et al. 2015; Russo et al. 2021). Also, it has been described as a G protein-coupled receptor 55 (GPR55) antagonist (Olah et al. 2014) and an agonist either of both adenosine receptor (ADR) 2A (Liou et al. 2008), and of all members of the transient receptor potential channels (TRP) [except for TRP melastatin subtype (TRPM) 8, for which exhibits antagonization effects] (Petrocellis et al. 2011; Hammell et al. 2016). Additionally, CBD also interacts with Peroxisome Proliferator-Activated Receptor gamma (PPAR-γ) (Gegotek et al. 2019). Finally, CBD is also capable of binding to 5-HT1a receptors and playing a significant role as agonist (Chiocchetti et al. 2022; Almeida and Devi 2020).
Natural sources and chemical synthesis
Phytocannabinoids are non-nitrogen terpenophenols (Russo et al. 2021)) mainly produced and stored within the glandular trichomes of female flowers of C. sativa L. (Gagne et al. 2012). In fact, despite the complexity of cannabinoid synthesis pathways is not yet entirely elucidated (Luo et al. 2019), there is already some knowledge about its main stages. In a first step, to form olivetolic acid (OA), consecutive condensations occur between hexanoyl-CoA and malonyl-CoA followed by a cyclization (Gagne et al. 2012). Subsequently, a Friedel–crafts-like alkylation between the synthesized OA and geranyl phosphate takes place to produce cannabigerolic acid (Happyana et al. 2013). Cannabigerolic acid is later converted into cannabidiolic acid (CBDA) (Gagne et al. 2012), the most abundant cannabinoid in this plant (Hanus et al. 2005). CBDA further undergoes a non-enzymatic decarboxylation to form CBD (Wang et al. 2016).
Nowadays, most of the CBD used for pharmaceutical purposes is extracted from C. sativa. Nevertheless, it requires a lot and rigorous purification to avoid contaminations with heavy metals and pesticides. Additionally, as in nature there are no stereoisomers, CBDs chemical synthesis has been the focus of many studies (Pirrung 2020). Although CBD is commonly synthesized using olivetol or its derivatives, different strategies for its chemical synthesis and to increase their yield had been and are still being investigated. These include Friedel–Crafts alkylation’s, biotechnology-based synthesis, Diels–Alder reactions (Aguillon et al. 2021), cyclohexenyl monoacetate alkenylation (Kobayashi et al. 2006) and enantiospecific synthesis (Shultz et al. 2018).
The demand and consumption of CBD in different sectors, and more impactfully in the pharmaceutical sector, has increased exponentially in the last decades. Hence, it is of utmost importance to develop more effective purification, extraction, and synthesis techniques, and procedures to meet all the necessities of this actual reality.
Dermatological biological activities
Ancient medical patterns in the literature describe that cannabis has been used in different dermatological conditions for centuries. In this way, also studies, pre-clinical and clinical evidence about CBDs applications and benefits have already begun to exist to treat several skin conditions.
One of them is ATD, a chronic inflammatory skin disorder in which skin integrity and immune system are compromised, characterized by skin intense pruritus, itching, skin inflammation (Zeng et al. 2021) and skin dryness. There is not only a dysregulation of sebaceous glands (Zakany et al. 2018) and an overdifferentiation of Th2 cells (Gong et al. 2020; Rundle et al. 2021), but also elevated levels of inflammatory mediators (chemokines, cytokines, growth factors, histamine) (Zeng et al. 2021). Additionally, there is a reduction in the production of keratin, fillagrin, desmossomal cadherins (Gong et al. 2020) and ceramide (Zakany et al. 2018).
Another relevant skin condition is psoriasis, an inflammatory skin pathology, characterized by silvery (Loft et al. 2022) squamous plaques arising from the abnormal differentiation and proliferation of epidermal keratinocytes, hypervascularization of the dermis (Rio et al. 2018a) and inflammatory cell accumulation at dermal and epidermal levels. This disease can be triggered by mechanical trauma, stress or by a microbial infection of the skin (Young et al. 2008).
Acne has also been associated with having benefits from CBD application, being a multifactorial skin disease in which there is an overproduction of sebum largely driven by abnormally high hormonal levels. Infection by Propionibacterium acnes and disturbances of sebum composition are of particular importance for the exacerbation of this disease (Shi et al. 2015).
Epidermolysis bullosa has also shown relevance, consisting of a group of hereditary bullous diseases manifesting debile skin integrity as a result of abnormal skin layers junctions (Meyer-Mueller et al. 2022) that develop significant blisters or ulcerations with a minimal trauma (Loh et al. 2014), both in internal or external organs/ tissues (Meyer-Mueller et al. 2022).
Another relevant disease in systemic sclerosis, a chronic connective tissue disease whose mechanism of fibrosis is thought to be a combination of an abnormal immune system and alterations in blood vessels. Together with collagen deposition and the proposed fibroblasts oxidative stress (Bourji et al. 2015), this leads to a variety of pathological conditions comprising chronic structural and functional deteriorations (Mei et al. 2020).
Seborrheic dermatitis and scalp psoriasis have also been mentioned, being multifactorial inflammatory dermatoses (Vincenzi and Tosti 2020), characterized by red, greasy, and squamous patches mainly in areas with a high density of sebaceous glands, such as scalp, face, upper trunk and inguinal region. These characteristics are associated with hormonal variations, distinct sebum composition, Malassezia colonization and a subsequent exacerbated immune reaction (Ghodsi et al. 2015).
Androgenetic alopecia has also been linked to benefiting from CBD properties, being a common skin disease characterized by an excessive and progressive hair loss. This hair loss results from an anagen phase shortening and a telogen phase lengthening at each hair cycle, leading to a hair thinning and shortening at a first stage, and to a reduction of the hair number at an advanced phase (Tampucci et al. 2022).
Melanoma, the most severe and with the worst prognosis skin cancer (Gruber et al. 2021; Pereira et al. 2023), that arises from the abnormal and malignant differentiation and proliferation of melanocytes (Rio et al. 2018a), has also been known to benefit from CBDs action.
Hence, the multiple CBD's biological properties discovered and researched to date are enough to already make this phytocannabinoid a potential candidate for these and other skin-related conditions (Fig. 2).
Hydrating and moisturizing
CBD has different ways of reducing excessive skin water loss and, thus, increasing its water content. On one hand, CBD stimulates sphingomyelinase and consequently, by enhancing sphingomyelin (SGM) cleavage, rises ceramides levels, reinforcing the structure of the epidermis and preserving skin moisture (Luczaj et al. 2020a). On the other hand, CBD has been shown to increase the expression of aquaporin-3 (AQP3) which, as it improves glycerol transport in different skin cells, improves skin water retention (Fig. 3). Using hairless mice and by measuring their skin dermal water content (DWC), it was shown that, compared to the control group, CBD increased DWC at the same time that the skin barrier integrity was maintained intact. Additionally, as CBD has not affected neither transcription nor expression of skin moisturizing factor-related genes, the observed results were due to AQP3 modulation, probably by activation of PPAR-γ. As it is an important glycerol and water transporter involved in cutaneous water retention, CBD may improve skin water content also by increasing AQP3 expression in skin keratinocytes (Ikarashi et al. 2021). Furthermore, in a different study, carried out on keratinocytes of psoriatic patients ultraviolet (UV)-irradiated, it was observed that 4 μM of CBD led to a significant reduction in the SGM concentration (Luczaj et al. 2020b), as it was shown in the skin of nude rats. There was also a simultaneously an increase of sphingomyelinase activity and consequently of ceramides levels. Ceramides play a key role in the transepidermal barrier function, contributing to the prevention of extreme water loss. Hence, CBD, through modulation of SGM metabolism, may promote skin water retention and, thus, improve DWC (Luczaj et al. 2020a).
a Schematic representation of the method used to analyze the skin moisturizing effect of CBD after 14 days of application of an aqueous solution of 1% CBD; b Comparison of skin aquaporin (Aqp) mRNA expression levels assessed by real-time RT-PCR between the control group and the CBD-treated group; c Measurement results of the DWC (A) and transepidermal water loss (B); d Analysis of the removed skin sample of the control group (A) and the treated group (B) by hematoxylin and eosin staining; e and f Evaluation of the mRNA expression levels of the pro-inflammatory proteins tumor necrosis factor-alpha (Tnfa) and cyclooxygenase-2 (Cox2) (Adapted from: (Ikarashi et al. 2021))
Hair growth modulation
Hair is a complex skin appendage essential for the survival and reproduction of some species. It has an important role in a variety of biological functions just as physical and mechanical protection, thermoregulation, sensorial experiences, and sexual attraction (Azuma et al. 2019). It is made up of dead keratinocytes and generated in the hair follicles (HFLs), which in turn undergo continuous turnover cycles, where new cells are produced and the old ones are forced to fall down (Bhinge et al. 2021). This hair growth cycle can be divided into different stages: anagen (proliferation and growth phase), catagen (involution phase), and telogen (resting phase) (Azuma et al. 2019). These stages are influenced by different cells and mediators like human dermal papilla cells, basal HFL matrix cells, keratinocytes, growth factors, EC and androgen hormones (Serruya and Maor 2021). Thus, it is understandable that any condition or disorder that affects one or more of these elements, including some diseases, nutritional or hormonal imbalance, aging, and stress may affect hair growth and/or lead to excessive hair loss (Azuma et al. 2019). It will do so by disturbing, in most cases and via neuroendocrine pathways, the HFL cycle, leading to an early end and an early start of anagen and catagen, respectively (Szabo et al. 2020).
Similar to the skin, the ECS is also present in HFLs and EC has been shown to influence the different stages of their cycle and, thus, control the HFL cell growth (Biro et al. 2006). Of the various receptors that constitute the ECS, it is known that in HFLs exists: CB1R, expressed in the outer root sheath (ORS) and whose expression seems to vary throughout the HFL cycle (Telek et al. 2007); several TRP Vanilloid Subtype (TRPV) 1, TRPV4 and TRPV3, expressed in an HFL cycle-dependent way mainly in the ORS, which inhibit matrix proliferation and hair shaft elongation and stimulate HFLs cell apoptosis and early initiation of catagenesis (Bodó et al. 2005; Szabó et al. 2019; Borbíró et al. 2011); ADR, of which ADR2A and ADR2B are on ORS and on some dermal papilla cells, and ADR3 on matrix keratinocytes, all stimulating anagenesis and inhibiting catagenesis (Iino et al. 2007).
CBD showed that when applied in different doses it presents different effects, probably mediated by two distinct receptors. On the one hand, at low concentrations (0.1–1 μM), CBD promoted hair shaft elongation without any influence on anagenesis/catagenesis nor the number of proliferating cells in human HFLs and downregulated pro-inflammatory cytokine levels, probably via ADR stimulation. On the other hand, at higher concentrations (10 μM) it exhibited procatagenic activity, inhibited hair shaft growth and stimulated an increase in the number of cells in apoptosis, which seems to be associated with TRPV4 (Szabó et al. 2017). Also, adults diagnosed with androgenetic alopecia applied 3-4 mg of CBD in all their bald areas once a day for 6 months. At the end of this period, all together showed a 93.5% increase in hair count, supporting the idea that CBD has hair growth benefits (Smith and Satino 2021). Despite all the data obtained, further studies are needed to establish the most advantageous topical dose of CBD for hair growth and the mechanism of action by which it exerts this activity.
Sebostatic
Sebaceous gland dysfunctions leading to both hypo- and hyperproduction of sebum are present in various pathologies. An example is acne, whose pathology includes hyperproduction and hyperexcretion of sebum by sebaceous glands as a result of their overstimulation by the higher levels of hormones typical of the puberty (Shi et al. 2015). Seborrheic dermatitis is also relevant in this context, and here dysfunctions are mainly related to hormonal variations and abnormal sebum composition (Ghodsi et al. 2015).
Although what is known about the sebostatic properties of CBD is still scarce, the existing studies show promising results. The suppression of cellular proliferation is another CBD biological property that makes it a promising compound for the treatment of different dermatological conditions. In a study using SZ95 sebocytes, CBD not only has suppressed their proliferation in vitro without diminishing cellular viability nor inducing apoptosis or necrosis, but it has also decreased MK167 expression, a proliferation marker (Olah et al. 2014). Moreover, a shampoo containing 0.075% broad-spectrum CBD applied for 14 days, has shown to have sebostatic activity in subjects diagnosed with mild to moderate scalp psoriasis or seborrheic dermatitis (Vincenzi and Tosti 2020). Furthermore, a study to assess CBD effects on the sebaceous glands showed that CBD exerts sebostatic actions through ECS and non-ECS mechanisms, by having reversed the induction of lipogenesis by arachidonic acid and by a combination of linoleic acid and testosterone. CBD blocks the AEA TRP-stimulation of sebum production and activates TRPV4, the main TRP channel expressed in SZ95 sebocytes, which is responsible for its CBDs lipostatic action (Olah et al. 2014).
Antipruritic
Pruritus is characterized by an unpleasant sensation that leads to a desire to scratch and represents a defense mechanism against external agents. When it becomes chronic or is exacerbated over a long period it can not only lead to the onset of skin lesions but also triggers the release of several pro-inflammatory molecules that eventually lead to an increased urge to scratch (Steinhoff et al. 2006). A large part of the diseases that affect the integrity of the skin and which have inflammatory components and/or adjacent alterations of the sebaceous glands, develop pruritus as one of their main symptoms. On one hand, epidermolysis bullosa is characterized by an extremely fragile skin along with pain and itching (Loh et al. 2014). On the other hand, eczema, ATD, psoriasis, and scalp psoriasis are inflammatory skin disorders associated with intense itching and burning, mainly when exacerbated or at a more advanced stage (Loft et al. 2022; Vincenzi and Tosti 2020; Thyssen et al. 2013).
The anti-pruritic potential of CBD has been studied and is increasingly gaining attention given the successful, though limited, results that have been obtained. A survey study was carried out to evaluate, in part, the types of cannabinoid-based medicines (CBM) used and the evolution of symptoms in patients with epidermolysis bullosa. It was observed that the topical formulations were the most commonly adopted route of administration and that the most frequently used CBMs were those combining THC with CBD (34.7%) and those containing only CBD (20.33%). The antipruritic action of CBD was felt by the majority of patients (90.9%), who admitted to having had a significant improvement in pruritus and with more than half of them no longer have needed or have reduced anti-itch therapy doses (Schräder et al. 2021). Also, a case report of a sublingual CBM containing CBD administrated to three patients suffering from epidermolysis bullosa has shown that together they experienced an effective improvement in the severity, intensity, and frequency of itching and a decrease in the urge to scratch (Schrader et al. 2019). Supporting these observations regarding epidermolysis bullosa, a 10% CBD containing broad spectrum hemp oil, without THC, applied for a minimum of eight weeks in dogs diagnosed with ATD has been shown to decrease the intensity and recurrence of itching after just two weeks (Mogi et al. 2022).
Although there are still no mechanistic or molecular studies reporting the effect of CBD on pruritus and the case reports that have been conducted lack scientific strength and statistical significance, this phytocannabinoid has the potential for further studies in this area.
Antimicrobial
Given the rapid growth in nosocomial infections largely due to the overwhelming increase in the occurrence of multi-drug resistant bacteria and of ESKAPE (Enterococcus faecium, Staphylococcus aureus; Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter spp.), developing new strategies and alternatives is becoming urgent (Abichabki et al. 2022). Besides all skin infections, there are several diseases associated with the colonization of the skin by different microorganisms whose treatments are often associated with various side effects or for which there is often no molecule that can simultaneously combat more than one of the pathological factors associated with the disease. An example of this is acne, in which colonization by Propionibacterium acnes contributes for its severity (Ghodsi et al. 2015). Additionally, seborrheic dermatitis and scalp pruritus are also relevant in this context, since they are common dermatoses characterized by an inflammation of the skin associated with Malassezia spp overgrowth and whose skin saturated fatty acids metabolization into skin irritating free unsaturated fatty acids trigger the immune system by penetrating the cutaneous layers (Shi et al. 2015).
The discovery of new natural antimicrobials can represent a potential solution for the treatment of numerous infections, including topical ones (Muscara et al. 2021). Although the antimicrobial activity of CBD has been described for some decades, it was only in 2008 that it began to be given proper attention, giving rise to further studies on account of its promising results (Abichabki et al. 2022). Gram-positive (Gram +) bacteria are more susceptible to the different factors and compounds due to their structural characteristics than Gram-negative (Gram-) strains which have a solid and distinct outer membrane and an important structural and virulent factor, the lipopolysaccharide (LPS) (Martinenghi et al. 2020). In different studies, CBD demonstrated a constant antibacterial activity against different Gram + bacteria, including multi-drug resistant strains and Propionibacterium acnes. The minimum inhibitory concentrations were fairly consistent among them, ranging from 2 to 4 μg/ml for Abichabki et al. (Abichabki et al. 2022) to 1–4 μg/ml and 0.5 – 1 μg/ml in previous studies (Blaskovich et al. 2021; Appendino et al. 2008). Also Gram- bacteria CBD showed consistent results among different studies, showing no antibacterial activity in at least 20 species, including Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, and Acinetobacter baumannii, except against Neisseria gonorrhoeae, N. Meningitidis, Moraxella catarrhalis and Legionella pneumophila, for which it appears to be a potent antibacterial compound (Abichabki et al. 2022; Martinenghi et al. 2020). The mechanism of action by which CBD exerts its antibacterial activity is far from being fully understood. Notwithstanding, it has been described as a bactericidal agent with a low propensity to develop resistance that decreases membrane potential (Wassmann et al. 2020). It has also shown to act by inhibiting the synthesis of nucleic acids, lipids, and peptidoglycans, disrupting the cytoplasmic membrane and consequently leading to bacterial death, as observed in a study in which Staphylococcus aureus was exposed to CBD concentrations of 6 to 14 μM (Blaskovich et al. 2021). Moreover, it has been shown to inhibit the release and alter the morphology and size of membrane vesicles in E. coli and S. aureus, important structures for biofilm formation, survival, and pathogenicity of Gram- (Kosgodage et al. 2019).
One of the strategies that allows reducing the amount of a determined required antibiotic and the probability of emergence of new drug resistance is the combination of the antibiotic with other drugs, antibiotics or not. For Martinenghi et al. CBD did not show any synergistic effects with the most commonly used antibiotics (Martinenghi et al. 2020). But for Kosgodage et al. CBD in combination with antibiotics has been shown to improve its antibacterial effects compared to using them alone (Kosgodage et al. 2019). When tested in combination with low concentrations of Polymyxin B (PMB) (< 2 μg/ml), it showed to exponentially decrease the number of colony units formed per milliliter compared to the same concentrations of PMB alone. Additionally, it also proved that CBD at concentrations ≤ 4 μg/ml holds antibacterial activity against Gram- bacteria, including K. pneumoniae, E.coli and A. baumanni (Abichabki et al. 2022). Moreover, when Gram + were exposed to bacitracin associated with CBD, it was observed that besides the minimum inhibitory concentration of bacitracin was dozens of times lower (from eightfold to more than 64-fold). Furthermore, together they led to morphological and cell division disturbances, which was not observed when both were used alone (Wassmann et al. 2020). Given the consistent results reported to date and bearing in mind that therapeutic efficacy may be highly formulation-dependent (Appendino et al. 2008), CBD could eventually be repurposed as an antibacterial agent.
Anti-inflammatory
Several skin diseases have an associated inflammatory component, which is either related to their pathological mechanisms or their symptoms, as observed in ATD and psoriasis (Luczaj et al. 2020a). On one hand, ATD is an example of a complex and multi-factorial chronic inflammatory skin disease largely related to dysfunctions in the skin barrier and immune system (Zeng et al. 2021), where there is a typical secretion of different inflammatory mediators (Zeng et al. 2021; Gong et al. 2020; Rundle et al. 2021). On the other hand, psoriasis is a chronic inflammatory skin disease mediated by the immune system and characterized by inflammatory infiltrates at different skin layers (Young et al. 2008). In turn, there are also other diseases such as acne, seborrheic dermatitis, and scalp pruritus that, although they have other preponderant factors underlying their pathology, have a strong inflammatory burden.
The mechanisms by which CBD exerts its anti-inflammatory actions are not yet fully elucidated. It is known that one of its main mechanisms is the downregulation of the Nuclear factor-kappa B (NF-κB) signaling and there are several pathways by which CBD decreases NF-κB levels. These include, apart from others, the inhibition of the epidermal growth factor—epidermal growth factor receptor interaction (Elbaz et al. 2015), and consequently, inhibition of NF-κB pathway activation (Biswas et al. 2000). Additionally, they also include inhibition of the expression of several NF-κB-stimulating proteins, such as heat shock proteins, and induction of NF-κB translocation to the nucleus (Gegotek et al. 2021c). However, by interacting with different receptors, CBD contributes to the decrease of general inflammatory conditions by reducing levels of numerous interleukines (ILs), such as IL-6, IL-1, IL-4, IL-5, IL-13, IL-8, and IL-1β (Olah et al. 2014; Szabo et al. 2020; Gui et al. 2014; Vuolo et al. 2019), tumor necrosis factor-α (TNF-α) and cyclooxygenase-2 (Castillo et al. 2010). It also leads to decreasing inducible nitric oxide synthase activity (Vincenzi and Tosti 2020) and NF-κB-mediated transcription of pro-inflammatory genes (Hou et al. 2012).
Several animal studies have demonstrated the anti-inflammatory potential of CBD on the skin. At the molecular level, the application of CBD to the skin in nude rats, after UV irradiation, significantly attenuated the increase of NF-κB and TNF-α levels (Gegotek et al. 2021a), which is in agreement with the study of Olah et al. in SZ95 sebocytes. Is this study, the elevation of TNF-α, as well as IL-6 and IL-1β induced by inflammatory stimuli, was highly prevented (Olah et al. 2014). These results were also observed in human ORS keratinocytes by Szabo et al. and in HaCaT and human dermal fibroblasts by Sangiovanni et al.. Is these studies, CBD, after treatment of the cells with pro-inflammatory molecules, toll-like receptor 3-activator polyinosinic-polycytidylic acid and TNF-α, respectively, effectively inhibited the release of several IL, TNF-α and even limited the transcription of pro-inflammatory factors by NF-κB (Szabo et al. 2020; Sangiovanni et al. 2019). However, in animal models in which inflammation of the skin was induced, while CBD was shown to reduce the edema formed at doses of 1 mm and 100 mg, higher doses had no effect (Lodzki et al. 2003; Miltner et al. 2018).
Antioxidant
CBD antioxidant properties, just like anti-inflammatory ones, represent one of its main biological activities. In addition to the inflammatory environment present in numerous diseases, oxidative stress and its cellular, molecular, and metabolic implications also represent pathological mechanisms of ATD and psoriasis, as well as alterations inherent to UV irradiation (Luczaj et al. 2020a). Different in vivo and in vitro studies conducted on different keratinocyte cell lines and models, have demonstrated that CBD exerts its antioxidant actions through different mechanisms, all contributing to the decrease of the oxidative environment and the regulation of the redox balance (Luczaj et al. 2020b). In this way, CBD has proven to have the ability to decrease the levels and activity of reactive oxygen species (ROS) generating enzymes, such as NADPH oxidase and xanthine oxidase (Atalay et al. 2020b; Wojcik et al. 2020). Additionally, it also showed to be capable of upregulating the activity of glutathione reductase and thioredoxin reductase, with a consequent increase in the levels of glutathione and thioredoxin, both compounds with important antioxidant activity (Biernacki et al. 2021; Jastrzab et al. 2021). Complementing this mechanism of decreasing ROS levels, Hamelink et al. demonstrated that CBD also has the ability to reduce these reactive molecules by chelating transition metals required for their synthesis reaction (Hamelink et al. 2005). Furthermore, Jastrzab et al. and Biernacki et al. observed that when CBD was applied to nude rats for four weeks, this phytocannabinoid, by modulating the ECS, led to increased levels of EC and to changes in the expression of the receptors of which they are agonists: CB1R, CB2R, and TRPV1. With PPAR-γ being linked to antioxidant actions when activated by CBD and 2-AG (Biernacki et al. 2021; Jastrzab et al. 2021), CB2R is associated with anti-inflammatory responses and CB1R with increased ROS and TNF-α production and their consequent inflammatory responses (Han et al. 2009), the upregulation of PPAR-γ and CB2R and downregulation of CB1R may account for yet another mechanism for the decrease in ROS levels (Biernacki et al. 2021). CBD has also been shown to induce the expression of nuclear factor erythroid-2 related factor (NRF2), which is associated with the production of antioxidant and cytoprotective proteins and for which CBD has shown to be an activator (Jastrząb 2019; Casares et al. 2020). Thus, by decreasing the production and levels of ROS and pro-oxidant factors and by increasing molecules, receptors, and enzymes that contribute to a general anti-oxidant action in keratinocytes, CBD prevents oxidative stimuli-induced alterations in membrane phospholipids, such as the production of lipid peroxidation products (Atalay et al. 2020b). In this way, CBD contributes to preventing the formation of adducts with proteins (Gegotek et al. 2021c), which allows for keeping intact and functional different proteins that are important for the maintenance of cellular homeostasis, such as chaperones (Atalay et al. 2021a, 2021b).
Wound healing
Wound healing is an innate process that allows a prompt and efficient tissue damage and rehabilitation (Brownhill et al. 2021). It results from an interaction between different cells, growth factors, and various mediator substances and it occurs in a sequential way that includes three main phases (Correia-Sa et al. 2020; Mascarenhas-Melo et al. 2022). After an initial inflammation, a proliferation period follows, which comprises granulation, tissue synthesis, re-epithelization, and angiogenesis, with fibroblast deposition in the extracellular matrix and keratinocyte proliferation and migration towards the wound. Lastly, dermal remodeling occurs, in which a reorganization of the extracellular matrix happens to restore skin integrity (Sangiovanni et al. 2019; Wilkinson and Hardman 2020). It is thought that the ECS also play an important role in wound healing processes. Endocannabinoids are present during the wound healing process in higher concentrations than in normal skin, where they influence skin cells proliferation and inhibit their apoptosis (Gegotek et al. 2021b). Additionally, CB2R is overexpressed in skin fibroblasts and macrophages and are highly involved in re-epithelization, cell proliferation, fibrinogenesis and in reducing the inflammatory environment. Furthermore, as it involves continuous interactions between immune and non-immune cells, both releasing signaling cytokines for inflammatory and regenerative responses, it may have a strong influence during tissue repair periods (Ruhl et al. 2021).
In this context, CBD is being study as a potential new therapy molecule to accelerate wound healing. The activity of a C. sativa L. ethanolic extract and pure CBD on the expression of wound healing relevant genes was evaluated. Treating HaCaT cells and human dermal fibroblasts with TNF-α it was found that TNF-α upregulated several genes including extracellular matrix enzymes, pro-inflammatory molecules and growth factors. Of the 26 genes raised in HaCaT cells, whereas the ethanolic extract down-regulated all of them, CBD only did it for 15. The same was observed in human dermal fibroblasts, where of the 16 upregulated genes, CBD was only able to reverse 11. It can be concluded that CBD has the ability to act against pro-inflammatory mediators associated with wound healing, favoring this process, but there are other compounds in cannabis that act synergistically to obtain better results (Sangiovanni et al. 2019). However, the activity of CBD in wound healing was also observed by Zheng et al. who developed a hydrogel containing CBD and studied its healing ability in SD rats subjected to a surgical wound creation. Over 10 days of treatment, and compared to the non-CBD hydrogel, faster healing was observed with a lower percentage of the area remaining. Furthermore, the rats’ skins were evaluated on the seventh and fourteenth day and it was found that CBD hydrogel led to a higher epidermis regeneration, collagen deposition, granulation tissue development, and number of new HFLs, while decreasing the levels of inflammatory cells. This proved the acceleration of wound healing in vivo and what is in agreement with the anti-inflammatory, anti-oxidant and anti-bacterial activities of CBD (Zheng et al. 2022). Moreover, CBD applied continuously to different children diagnosed with epidermolysis bullosa led to a marked reduction in blistering and its healing time, and often allowed the suspension of analgesic medication (Chelliah et al. 2018).
Photoprotection
UV radiation comprises, not only but also, UVA and UVB radiation, the major radiation types causing damage to skin cells. UVA radiation, comprised between 320 and 400 nm (Luczaj et al. 2020a), penetrates into deep dermis causing vascular damage and modulating fibroblasts, dendritic cells, and immune cells metabolism (Biernacki et al. 2021). On the other way, UVB radiation, whose radiation is comprised between 280 and 320 nm (Luczaj et al. 2020a), reaches predominantly the epidermis affecting its keratinocytes metabolism and molecular physiology (Gegotek et al. 2021a) and promoting its cells to release a variety of signaling molecules into the bloodstream. Skin cells exposure to both radiation types leads to an induction of an inflammatory response by stimulating the generation of pro-inflammatory signaling molecules, including ROS and reactive nitrogen species (Biernacki et al. 2021). It also leads to the hyperproduction of lipid peroxidation products (molecular aldehydes and isoprostanes), labeled as one of the fastest and most reactive signals transducers (Gegotek et al. 2021b), and the enhanced secretion of skin neuroendocrine system products, such β-endorphin, adrenocorticotropic hormone, corticosterone, and corticotropin-releasing hormone. Consequently, skin structure and function are compromised, immune system becomes fragile and has not the same immunological response efficiency. Skin cells membranes, signaling and metabolism are also highly affected (Gegotek et al. 2021a), and macromolecules such as nucleic acids, lipids and proteins undergo oxidative reactions losing their functional structure and activity and contributing to the whole set of dysfunctional changes (Biernacki et al. 2021). Included in this whole set of targets and disturbances is the ECS: not only endocannabinoids production is diminished but also its receptors are overexpressed (CB1R, CB2R and TRPV1). This can be explained by the fact that CB1-CB2 heterodimers activation leads to the activation and translocation to the nucleus of transcription factor NRF2. In turn this will promote different proteins expression important to skin cells UV radiation defense. Nevertheless, this activation and transduction process can lead to malignant transformations when NRF2 is continuously and deregulatory activated (Gegotek et al. 2021b).
CBD has multiple properties that make it a potential molecule to counteract radiation damage in skin cells. These include the capacity to reduce ROS levels, regulate antioxidants and oxidative molecules to optimum levels, modulate the immune system and avoid exacerbated inflammatory responses. Its capacity of reducing the oxidative stress state stems from its regulation of ROS not only by trapping them, chelating essential metal ions or by stimulating antioxidant enzymes involved in their metabolization (Luczaj et al. 2020a), but also by regulating cannabinoid receptors activity (Biernacki et al. 2021). CRL-1474 human skin fibroblasts treated with CBD after irradiation with UVA and UVB underwent significant changes in certain protein expression. CBD decreased the levels of protein-lipid peroxidation products, mainly 4-Hydroxy-2-nonenal (4-HNE) and malondialdehyde (MDA), resulting from cell irradiation, and consequently the levels of transporters modified by them. It also lowered the expression of metalloproteinases, catabolic enzymes of the intracellular matrix. CBD has also shown to decrease the expression of NF-κB, breaking its pro-inflammatory pathway. Additionally, it has proven to upregulate the expression of antioxidant enzymes involved in glutathione metabolism, and of enzymes important in cell metabolism, survival and growth, fundamental for cell protection against UV radiation damage (Gegotek et al. 2019). The photoprotective effect of CBD was further supported by Luczaj et al. who studied the changes in lipid profile of keratinocytes after exposure to UVA and UVB radiation. If these radiations led to an increase in phosphatidylcholines, lysophosphatidylcholines, and phosphatidylethanolamines and a decrease in SGM, concomitant treatment with CBD resulted in significant differences in the levels of these compounds. It caused an increase in phosphatidylserines levels, demonstrating CBD's prevention of phospholipid oxidation, and phosphatidylethanolamines levels, leading to a decrease in the effects of oxidative stress via increased autophagy. It also induced down-regulation of lysophosphatidylcholines, decreasing the inflammatory environment resulting from radiation. In addition, it decreased SGM levels, accompanied by increased ceramide concentration, important for maintaining an integral epidermal barrier (Luczaj et al. 2020a). Though these effects of CBD had already been described in skin cells, similar and interesting results were also observed in the blood. When applied to the skin, CBD had been absorbed into the bloodstream, but its levels were low, due to its lipophilic nature and tendency to accumulate in lipid membranes, and were even reduced following UV exposure. Similarly to its activity in fibroblasts, CBD has been shown to increase the levels of enzymes and antioxidant compounds and decrease the synthesis of lipid peroxidation products. These effects have mainly been seen on 4-HNE and MDA, and ROS, both by activation of membrane receptors, including TRPVs and PPAR-γ, and indirectly by stimulating 2-AG synthesis, decreasing CBIR activation and increasing CB2R levels (Biernacki et al. 2021). Similarly, the same results were obtained by Gegotek et al., having further observed that CBD is able to prevent the release of keratin into the blood, induced by radiation, and which, by stimulating T cells, leads to widespread inflammation (Gegotek et al. 2021a).
Antifibrotic
The fibrotic process is not a fully understood physiologic but essential part of the repairing response (Wernig et al. 2017a). Fibrotic disorders often occur associated with autoimmune diseases, such as scleroderma, when there is a pathological imbalance that leads to the abnormal accumulation of components of the extracellular matrix in different organs and/or tissues that are inflamed or damaged (Wynn and Ramalingam 2012). Each fibrotic disease is thought to have different pathophysiological mechanisms (Wernig et al. 2017b) and it is known that there are several molecular and cellular mechanisms inherent to these diseases. These mechanisms involve various growth factors, cytokines, pro- and anti-inflammatory proteins, and various immune cells (Tager et al. 2008; Liu et al. 2015; Kitani et al. 2003).
Although the antifibrotic activity of CBD has not yet been sufficiently investigated, there are already some studies that corroborate its effects on the fibrosis process. The administration of 20 mg/kg of CBD in diabetic mice over 4 weeks, limited the diabetes-induced increase in fibrosis of the myocardium. A decrease in the expression of pro-fibrotic genes and collagen deposition in the myocardium was also observed (Rajesh et al. 2010). These results are in agreement with Lee et al. who observed a significant attenuation of the fibrosis process in the myocardium at the time of myocardial infarction in mice. It was also shown that this attenuation is due to a decrease of profibrotic factors, such as IL-6 and IL-1, and to a reduction in the transformation rate of the macrophages into myofibroblasts (Lee et al. 2016). Not only in the heart but also in the lungs CBD has been shown to reduce collagen deposition while decreasing levels of IL-4 and IL-13 (Vuolo et al. 2019), pro-inflammatory and pro-fibrotic cytokines that have been shown to stimulate collagen fiber and fibrous connective tissue formation (Bellini et al. 2012).
One of the fibrotic diseases that most affect the skin is systemic sclerosis, a chronic connective tissue disease (Bourji et al. 2015). Although CBD effects have not been directly studied for this disease, in addition to the fact that its antifibrotic properties may prove to be effective in systemic sclerosis, VCE-004.3 (CBD-aminoquinone), a CBD derivative and selective agonist of PPAR-γ has shown promising results. PPAR-γ has already been shown to be associated with antifibrotic activity, both by activating signaling pathways that lead to decreased pro-inflammatory cytokines (Odegaard et al. 2007) and by limiting fibroblast activation by transforming growth factor β (TGF-β1) (Kulkarni et al. 2011), which has profibrotic properties (Kitani et al. 2003). In this context, it was observed that VCE-004.3 not only led to a decrease in TGF-β1-induced collagen synthesis in vitro, but like in the CBD studies, attenuated the increase in the cytokines IL-4 and IL-6 and the fibrosis in established-skin fibrosis mice (Rio et al. 2018b). More recently, a study showed that CBD was able to reduce BLM-induced dermal fibrosis (Rio et al. 2022). Thus, studies on the antifibrotic activity of CBD in systemic sclerosis and other fibrotic diseases affecting the skin should be carried out to directly understand the potential of this molecule in these chronic diseases.
Antitumoral
Given the increasing prevalence of various types of cancer throughout the world, there is an urgent demand to find more specific, more effective, and safer anticancer therapies. CBD has already shown promising antitumoral activity in different types of cancer cells via several mechanisms of action, although not all have been fully detailed or are well understood to date. In several in vitro and in vivo studies of various types of cancer such as glioma (Vaccani et al. 2005; Nabissi et al. 2015; Aparicio-Blanco et al. 2019), breast cancer (Elbaz et al. 2015), lung cancer (Hamad and Olsen 2021), colorectal cancer (Yun et al. 2019), leukaemia (Olivas-Aguirre et al. 2019; Lee et al. 2008), gastric cancer (Jeong et al. 2019) and melanoma (Junaid et al. 2022), CBD has been shown to successfully inhibit the migration of cancer cells (Vaccani et al. 2005; Olivas-Aguirre et al. 2019) and the progression of metastases and tumor growth (Elbaz et al. 2015; Jeong et al. 2019). It has also shown to induce cell death, mostly by apoptosis, through different mechanisms, such as stimulation of ROS production (Hamad and Olsen 2021; Lee et al. 2008) and induction of endoplasmic reticulum stress (Yun et al. 2019), resulting in mitochondrial damage and consequent organelle and cell dysfunction. It has also been proven to induce cell death by suppression of apoptosis inhibitory proteins, such as X-linked inhibitor apoptosis (Jeong et al. 2019; Burch et al. 2021), ATP depletion (Lukhele and Motadi 2016), and activation of autophagic processes (Olivas-Aguirre et al. 2019).
The most frequent human tumoral disorder is skin cancer (Xu et al. 2020) and melanoma is the malignant, most aggressive, and most lethal form (Gruber et al. 2021). Several studies have been conducted to establish the activity of CBD on melanoma cells. In a study using different types of human melanoma cell lines, CBD in a concentration range of 2–10 μg/ml was shown to reduce both cell viability and proliferation in a concentration-dependent manner, only exhibiting toxicity to normal keratinocytes at concentrations much higher than required to exert the described effects (Marzęda et al. 2022). These results are consistent with another study in B16 mice melanoma cells, in which CBD, although used at much higher concentrations of 200 μg/ml, decreased melanoma cell counts by more than 50% compared to the positive control (from 75,000 to 30,000 cells). It also suppressed cell growth in a concentration-dependent way: higher concentrations (200 and 40 μg/ml) showed inhibition percentages of 60% and 20%, respectively, which was much higher than the lower concentrations (8 and 16 μg/ml), whose results were not relevant (Burch et al. 2021). Following these results, Choi et. al also demonstrated that CBD exhibits a concentration-dependent cytotoxicity in A549 melanoma cells, when applied at concentrations ranging from 5 to 80 μM, in a time course ranging from 6 to 36 h. This lead to a decrease in the number of viable cells from 100 to 20%, from the lowest to the highest concentration (Choi et al. 2008). Furthermore, CBD and THC, when co-administered in a 1:1 ratio of 1 μM THC and 1 μM CBD, showed a much higher reduction in the cell viability of different melanoma cell lines than that obtained with an equivalent concentration of THC. Additionally, they were also shown to inhibit the growth of CHL-1 xenografts tumors in a higher way. Compared to the in vitro results of THC, CBD administered with relatively low doses of THC boosts its anti-tumoral activity (Armstrong et al. 2015). To support CBD's antitumoral activity, in human skin keratinocytes transformed with HPV-16 E6/E7, CBD led to keratinocyte proliferation inhibition with an IC50 value lower than any of the IC50 presented by the other phytocannabinoids tested (Wilkinson and Williamson 2007).
Dermopharmaceutical delivery systems of cannabidiol
Topical formulations offer numerous advantages, such as the possibility of exerting a local drug effect, frequently associated with low toxicity and no or few systemic side effects. They also allow the use of lower drug dosages and longer administration intervals, enabling the immediate interruption of administration when necessary. Moreover, topical administration is a non-invasive and more comfortable route, potentially increasing patient compliance and ramp up the probability of a higher therapeutic success rate (Lodzki et al. 2003; Radwan-Pragłowska et al. 2021). However, topical administration of CBD presents some challenges, not only due to its physicochemical characteristics, but also on account of the efficient barrier function of human skin (Lodzki et al. 2003). On the one hand, if CBD delivery has the problem of being high lipophilic and having a poor solubility (Momekova et al. 2021). Additionally, dermatological application has its own formulation challenges, mainly if the intention of the preparation is its delivery into the dermis or deeper epidermis (or even for systemic delivery). The stratum corneum forms a strong barrier and just a few molecules can pass through it, mainly those whose logP is between 1 and 3, have a low molecular weight, below 500 Da, a solubility that supports a high membrane concentration gradient, and a low melting point (less than 200 °C) (Vanti et al. 2021; Kim et al. 2020). Considering these requirements, CBD presents many challenges when it comes to use in topical formulations, especially with regard to CBD’s extreme lipophilicity (LogP = 5.79), that may lead to its accumulation in the sebaceous glands, forming depots in the stratum corneum, as it tends to penetrate through the transfollicular route.
In the past years, efforts are being made to develop CBD dermopharmaceutical delivery systems and strategies to improve its skin biological properties and therapeutic potentials. These strategies have included the use of polyssacharides (Momekova et al. 2021) permeation enhancers (Paudel et al. 2010), different nanoparticles (NPs) formulations (Momekova et al. 2021), nanometric emulsions (Vanti et al. 2021; Park et al. 2021) and cryogels (Momekova et al. 2020, 2021; Heussler et al. 2019).
Conventional semi-solid formulations
Despite all the technological and biomedical advances that have been achieved in recent decades, many of the formulations used today are conventional, only improved and adjusted to enhance certain organoleptic, pharmacokinetic, pharmacological or toxicological characteristics. Of the various semi-solid formulations suitable for skin application, different forms of gels have undergone particular attention with regard to the cutaneous delivery of CBD (Table 2). Hydrogels have been studied and developed as topical drug delivery systems (Wang et al. 2020), many of which with the aim of prolonging drug release and thereby extending drug action over time (Namazi and Heydari 2014). Several advantages are highlighted, such as having a structure similar to the extracellular matrix (Li et al. 2018; Qu et al. 2018), low toxicity, little effect on drug biological properties, and a straightforward preparation method (Wang et al. 2020). However, some technological challenges are ascribed to these systems, such as their weakly functional mechanical properties (Li et al. 2018; Qu et al. 2018), and the impairment to control the release of hydrophobic molecules with low molecular weight, as CBD (Koshy et al. 2018; Pacelli et al. 2021).
A CBD gel in ethanol 72.5% w/w has exhibited excellent results in Sprague–Dawley rats, since plasma CBD concentrations showed linear pharmacokinetic profiles for the lowest CBD doses studied, as high as 6.2 mg/day. Additionally, it also showed promise in terms of its ability to decrease induced inflammation, both regarding swelling, immune cell infiltration and reduction in the levels of pro-inflammatory molecules, such as calcitonin gene-related protein and TNF-α (Hammell et al. 2016). Thus, this CBD gel shows potential application in several inflammatory diseases or with a strong inflammatory component, such as seborrheic dermatitis, scalp pruritus, common dermatoses, psoriasis, and ATD.
Satisfactory results were also obtained with an alginate-based CBD hydrogel containing zinc. This formulation showed good rheological properties, ensuring its integrity during the application, and a CBD release rate proportional to its concentration, reaching the plateau after 24 h (Fig. 4). The hydrogel also proved to have excellent antioxidant, antibacterial, anti-inflammatory and angiogenic activities. Compared to an alginate and zinc hydrogel without CBD, it showed higher ROS scavenging and a lower E. coli colony count than the other groups. It also led to a significant decrease of TNF-α, IL-6 and IL-1β levels, with the levels of IL-6 and IL-1β dropping below those of the control group. With regard to the expression of vascular endothelial growth factor and epidermal growth factor like domain multiple 6 (biomarkers of angiogenesis), both alginate and zinc hydrogels, with and without CBD, were shown to increase their expression, but little or no significant difference was observed between them. The truth is that zinc is a cofactor ion of multiple enzymes and has, by itself, antibacterial activity, besides promoting angiogenesis, which explains the excellent results obtained. Hence, these results arose from the synergistic activity of CBD with zinc, and the fact that the presence of CBD did not influence the values of angiogenic markers expression. The CBD hydrogel also showed a higher amount of granulation tissue and collagen deposition, together with a decrease in the amount of inflammatory cells, which makes it a promising candidate for wound treatment. Thus, this hydrogel presents wound-healing potential, as was later observed in in vivo in SD rats. In these studies, the reduction of the wound area previously created by surgery was much faster with CBD hydrogel, having, on the 10th day presented a remaining wound area of 13.72% (unlike the alginate and zinc hydrogel, the positive control and the negative control, which exhibited, respectively, areas of 17.08%, 25.84% and 34.33%) (Zheng et al. 2022). Furthermore, due to the excellent results presented with regard to this hydrogel's antibacterial, antioxidant and anti-inflammatory activities, its application for the treatment of epidermolysis bullosa, where chronic wounds are an impacting factor (Chelliah et al. 2018), may be effective. It may also be effective for the treatment of acne, which, being a multifactorial disease, encompasses inflammatory, oxidative and bacterial factors (Shi et al. 2015),.
a Schematic representation of a CBD alginate and zinc based hydrogel formulated for wound healing owing to its antioxidant, antibacterial, anti-inflammatory and angiogenic properties; b Release profile curves of cannabidiol from the different formulated hydrogels; c Macroscopic photographs of skin wounds of the control group and of the groups treated with the 3 M wound dressing, the pure hydrogel and the CBD containing hydrogel; d Wound healing rate analyzed in terms of percentage of remaining wound area over a 14-day period (Adapted from (Zheng et al. 2022))
Another study evaluated the influence of different vehicles in semi-solid formulations on CBD permeation through the skin (Table 3). In this study CBD-enriched Cannabis sativa seed oil was added to one hydrophobic ointment, G1, and three hydrophilic gels with different compositions, G2, G3 and G4. Using human epidermis as a membrane in Franz diffusion cells, it was observed that G4, to which glycerin was additionally incorporated, demonstrated the best results regarding the amount of CBD retained and accumulated, 53.64 ± 8.37 and 90.81 ± 29.20 μg/cm2, respectively. This happened mainly in the upper layers of the skin, given the high value of Qr24/J. Thus, G4 is suitable for future in vivo studies in patients with a wide range of skin pathologies, as it shows an excellent CBD permeation and retention profile, such as it is desired for the treatment of so many skin disorders (Curcio et al. 2021).
Conventional semi-solid formulations containing penetration enhancers
Penetration enhancers, by interacting with different skin structure components and by modifying skin arrangement, may enhance CBD’s absorption and diffusion through the different skin cells and layers (Vanti et al. 2021) (Table 4). Chemical enhancers alter skin resistance either by reversible stratum corneum lipid disposition or by increasing its lipid solubility. Transcutol, isopropyl myristate, and oleic acid were chosen to study their effectiveness in enhancing the permeation of 5% CBD in propylene glycol (PPG) in an in vitro study using human skin. In a 24 h period 40% w/w Transcutol in PPG did not lead to a considerable increase difference in the amount of CBD’s delivered compared to the control group (26.29 and 29.03 μg/cm2, respectively), probably due to the PPG similar permeation enhancing property. Additionally, 10% CBD in 10% w/w isopropyl myristate in PPG only resulted in a delivery of 5.92 μg/cm2. Nevertheless, a 5% CBD in 5% w/w oleic acid in PPG led to a considerable increase of CBD’s permeation with a delivery of 67.54 μg/cm2, at a faster rate and with a lower lag time. Furthermore, oleic acid showed to deliver a higher amount of CBD in both epidermis and dermis, 155.95 and 31.05 μg/cm2 respectively, compared to both the Transcutol and isopropyl myristate groups. Hence, oleic acid seems to be the most efficient penetration enhancer of 5% CBD w/w in PPG, apart from delivering the best results in terms of CBD delivery to the epidermis, the desired location for the treatment of various dermatological conditions, such as ATD and psoriasis (Junaid et al. 2022).
However, other transdermal studies have shown different and satisfactory results with other penetration enhancers. A study in hairless guinea pigs (the most appropriate alternative to the human skin in in vitro studies due to similar cannabinoids permeability results) has demonstrated that, by using Transcutol as a penetration enhancer at 6% (v/v) in a CBD transdermal gel formulation, pharmacokinetic parameters had a noteworthy improvement and an enhancement factor of 3.7. A flux increase was also observed, compared to the same formulation without the penetration enhancer, 14.81 nmol/cm2/h and 6.13 nmol/cm2/h, respectively (Paudel et al. 2010). The truth is that N-methyl-2-pyrrolidone (NMP), lactic acid (LA), and dimethyl sulfoxide (DMSO) also achieved highly satisfactory results with regard to the improvement of transdermal permeation of CBD gels. All of them led to a consistent increase in average CBD flux, up to values of 13.26 μg/cm2/h, and to a higher cumulative CBD permeation, having even reached 610.86 μg/cm2. Besides having improved the abovementioned parameters, the anti-inflammatory property of the corresponding gels has been further investigated. In Sprague Dawley rats in which a carrageenan paw edema was induced, it was reported that the edema rate of the CBD gel, compared to the control group where no treatment was provided, was 3.92 times lower after one day of CBD application. The proven anti-inflammatory potential of these CBD gels makes them promising study targets for CBD treatments in several skin diseases, such as ATD. It also shows potential in UV-irradiated skins, in which several inflammatory signaling cascades are triggered. Nevertheless, although chemical penetration enhancer shows promising results regarding the optimization of dermatological formulations and are worthy of further study in the future, some concerns stand out with regard to the high incidence of adverse effects (Salau et al. 2022).
Cannabidiol-loaded nanosized delivery systems
Nanotechnology has revolutionized various fields of science and has had a considerable impact on medicine and the pharmaceutical industry in the past years. By working with compounds at the nanoscale, it can develop and manipulate NPs with a considerably larger surface area, lower binding energy, and much higher reactivity than the traditional materials. NPs have been studied as an effective formulation strategy to deliver lipophilic drugs, such as CBD, to the skin. This is mainly due to the fact that they tend to concentrate in HFLs and follow the intercellular route, and thus they may be developed to have a controlled and prolonged release of the drug at the targets sites (Josiah et al. 2021) (Table 5). Thus, a strategy that has already shown excellent results with regard to administration by other administration routes, such as oral (Wang et al. 2022), intravenous (Liu et al. 2022), nasal (Matarazzo et al. 2021), ocular (Sosnik et al. 2021) and intraperitoneal (Fraguas-Sanchez et al. 2020) is CBD encapsulation.
Modification of hydrogels becomes necessary in these situations to achieve a controlled release of CBD. In line with this, Momekova et al. developed a hydrogel based on 2-hydroxyethyl cellulose (HEC) and beta-cyclodextrin (β-CD) into which CBD was subsequently incorporated (Fig. 5). By forming a macroporous structure these polysaccharides allow a higher CBD loading, which is partly adsorbed in the cavities of the β-CD, and the other part remains embedded in the inner surface. Thus, the CBD release occurs in a biphasic way, with a burst release of 50% of the loaded CBD in the first 3 h and, afterwards, a sustained release of the remaining amount. The opposite happens with the equivalent pure HEC hydrogel, unmodified by β-CD, which leads to a burst release of 96% of the CBD in the first 6 h. Although this gel led to a decrease of the antiproliferative effect of CBD compared to an ethanolic CBD solution, this delivery system does not counteract the biological activities of CBD. Moreover, by presenting a good biocompatibility, enabling the incorporation of a large amount of CBD and leading to its biphasic release, this modified hydrogel may be beneficial for melanoma treatment. It will expose malignant cells to a large and rapid initial amount of CBD, and allow them to remain subject to its antitumoral activity for a longer period of time (Momekova et al. 2021).
a Schematic representation of HEC/β-CD polymeric network and CBD-βCD complex; b Scanning electron microscopy analysis of CBD-loaded and pure HEC/βCD cryogels showing the surface difference of each sample as a consequence of the CBD particles absorption on the inner cryogel surface c Influence of HEC/βCD mass on the swelling degree of cryogels d In vitro CBD release profile of CBD-loaded HEC and HEC/βCD cryogels in acetate buffer (pH 5. 5); e Antitumoral activity of CBD in pure HEC and HEC/βCD cryogels on human tumor cell line Cutaneous T-cell lymphoma, CTCL-Cesary syndrome (HUT-78) (Adapted from (Momekova et al. 2021))
Polymeric NPs have been showing great and interesting results as skin delivery systems to improve the bioavailability of the different compounds, either by enhancing drug absorption/penetration and preventing early drug degradation, or as a method to control drug release (Abdel-Hafez et al. 2018; Pires et al. 2023). This has been observed in studies including vitamin A and octyl methoxycinnamate. Depending on the physical–chemical properties and structural characteristics, the different Polymeric NPs are capable of both achieving controlled drug release and allowing and prolonging the permanence of the formulation on the skin surface. This is done without compromising drug diffusion and delivery to the deeper layers (Alvarez-Roman et al. 2001, 2004; Mao et al. 2017), at the same time that they may reduce active ingredients toxicity. In this way, the application of encapsulated CBD to the skin was also subject of some studies. Polymeric NPs made of ethyl cellulose were developed using a non-surfactant compound. The main purposes were to, while preventing NPs aggregation, avoid the solubilization of CBD and thus the encapsulation efficiency (EE) decrease, and reduce the NPs’ size by decreasing the polymeric surface tension. Compared to solutions of different CBD concentrations, CBD ethyl cellulose NPs showed less toxicity up to CBD concentrations of 500 μg/1012 NPs. Furthermore, they have demonstrated an efficient CBD cellular uptake in HaCaT cells, proportional to the amount of CBD incorporated into the NPs added to the culture medium. It was further observed that the application of high concentrations of CBD, as high as 859 μg CBD/1012 NPs, despite leading to a lower viability of HaCaT cells, show good anti-proliferative effects. This could be beneficial in the treatment of both melanoma, by preventing the proliferation of malignant cells, and psoriasis, by attenuating the excessive proliferation of epidermal keratinocytes (Zamansky et al. 2021). Likewise, when CBD was encapsulated in polymeric micelles and incorporated into a HEC-based cryogel, it showed a more constant and slower release over 24 h. A pure HEC cryogel, used for comparison purposes, after a burst release of approximately 50% of the CBD, completed the release of CBD in 8 h. Such observations arise from the fact that in pure cryogel the CBD is embedded in the numerous macro-pores, and thus susceptible to a rapid dissolution when it is incorporated in polymeric micelles. As these remain within the cryogel matrix, CBD, to be dissolved, must first be released from the micelles and then diffuse into the medium, making the process slower and more progressive. The preservation of CBD antitumoral activity in an in vitro study on MJ cells (cutaneous T-cell lymphoma, Mycosis fungoides) has also been observed. Hence, together with the fact that it is provided its sustainable release, this cryogel might be a potential topical delivery system for the treatment of melanoma (Momekova et al. 2020).
Otherwise, one of the polymers showing a promising bright future for the development of novel and functional transdermal delivery systems is chitosan. It leads to no toxicity for skin cells, has intrinsic biological properties and the capacity of mucoadhesion, and leads to interaction with cellular membranes. This will lead to increased permeability and thus improved delivery of different compounds (Abdel-Hafez et al. 2018). Additionally, chitosan tends to form dense structured transdermal delivery systems capable of not only enhancing the effective incorporation of active substances, but also of controlling their release performance (Radwan-Pragłowska et al. 2021). A study involving the use of chitosan and collagen (CH/CL) NPs to stabilize pickering emulsions, formulated with olive oil and liquid paraffin, has shown that CH/CL NPs have the ability to improve CBD stability, EE, and skin penetration (Fig. 6). The percentage of CBD proved to be 99.45% after 5 months, whereas what was expected according to several CBD products on the market is a relatively fast degradation. Additionally, due to the formation of consistent oil droplets wall by the CH/CL NPs, the efficiency of CBD encapsulation has presented excellent values, all above 99%, thus allowing to effectively protect and encapsulate CBD. Moreover, pickering emulsions formulated with these NPs have been shown to improve the topical administration of this compound (Sharkawy et al. 2021), compared to solutions of 1% (w/w) CBD in liquid paraffin and olive oil, in a study performed to investigate the impact of the vehicle characteristics in the whole process of skin permeation. While the application of the solutions in the skin has led to an amount of CBD retained in the skin of 15.15 μg/cm2 for liquid paraffin and 6.45 μg/cm2 for olive oil after 24 h (Casiraghi et al. 2020), the new pickering emulsions have been shown to significantly increase the amount of CBD delivered to the skin, with results of 143.98 and 158 μg/cm2 for olive oil and 97.26 and 80.16 μg/cm2 for liquid paraffin. This can be justified through the ability of these PEs to change the order of the stratum corneum lipid components, and, thus, increase its fluidity with the consequent improvement of CBD penetration (Sharkawy et al. 2021). Sharkawy et al. corroborated the results obtained for pickering emulsions stabilized with chitosan NPs. They attempted to understand the influence of the degree of deacetylation (DOD) of the chitosan used in chitosan and gum arabic NPs on the stabilization of these formulations. They noticed that high DOD NPs not only showed higher hydrophobicity, but also better emulsification properties. Moreover, regarding the formulation of pickering emulsions, these NPs, by leading to the formation of a larger number of particles and, consequently, with a lower average droplet size, allowed a higher EE of CBD. They also allowed a higher emulsion stability, presenting a less pronounced increase in droplet size and showing no phase separation after a 60-day storage. The presence of these NPs in pickering emulsions was shown to promote the accumulation of 3.07% and 1.23% of the applied CBD in the stratum corneum and in the viable epidermis and dermis, respectively (Sharkawy et al. 2022), which are optimal concentrations for its use in cosmetics (Casiraghi et al. 2020). This absorption of CBD in the stratum corneum allows it to act as a reservoir, promoting subsequent prolonged release into the deeper layers of the skin (Sharkawy et al. 2022).
a Schematic representation of the preparation process of CH/CL NPs and the subsequent CBD-loaded pickering emulsion; b Photographs of all the different pickering emulsions at the moment of preparation and after a 30 days storage, whose creaming indexes (CI%) are respectively registered, and visual appearance of pickering emulsion 1 stored for 5 months; c Obtained optical microscopy images of fresh pickering emulsion 1 and after a storage of 5 months; d Comparison of the pickering emulsion droplet size distribution of fresh and stored formulations; e Amount of CBD that penetrated through each of the skin layers and into the receptor fluid after 24 h for all the formulated pickering emulsions (Adapted from (Sharkawy et al. 2021))
Another study showed that the modification of a hydrogel with chitosan and zinc oxide (ZnO) NPs significantly improved its characteristics to allow a controlled and prolonged release of CBD (Fig. 7). Furthermore, the functionalized hydrogel was porous, had a rougher surface, and improved the tensile strength. This allowed good water absorption, as desired for transdermal patches, but also better adhesion to the skin and higher durability. NPs has a large and specific surface area that allows them to have excellent sorption properties. In this way, the modified hydrogels were able to incorporate a higher amount of drug, about 90 mg/g vs 200 mg/g, pure and modified gel, respectively. Additionally, they released, and for a longer period, a minimum of 80% CBD, having even reached 100%, unlike the hydrogel which exhibited a maximum release of merely 60% and at a much higher rate (Radwan-Pragłowska et al. 2021).
a Pathway of preparation of chitosan/zinc oxide (ZnO) NPs transdermal delivery system and delivery of CBD to the skin; b Morphology of swollen pure hydrogel and swollen CBD-loaded hydrogel modified with ZnO NPs; c Swelling degree and percent porosity of pure hydrogels and chitosan-modified hydrogels formulated with different amounts of ZnO NPs; d Drug loading capacity of the various formulated samples; e CBD release profile for the various hydrogels modified with chitosan and different concentrations of ZnO NPs, under sink conditions, for 6 days (Adapted from (Radwan-Pragłowska et al. 2021))
Also, ethosomes, nanosized malleable vesicles made up of water, phospholipids, and ethanol, have also proved to be potential skin delivery systems. Ethanol fluidizes the lipids of the stratum corneum, reducing the integrity of the barrier that it represents, and improves the malleability of the vesicles (Bodade et al. 2013), contributing to an increase in the percutaneous delivery of hydro- or lipophilic molecules (Niu et al. 2019). In nude mice, a transdermal 3% w/w CBD ethosomal system led to the accumulation of CBD in the skin, crucial for the local treatment of several skin diseases. It also led to its identification in some internal organs, such as muscle, the liver, and the pancreas, after 24 h of application, as well as in plasma during a 72 h of application. Moreover, it has also shown to efficiently prevent the localized acute inflammatory reaction induced by carrageenan, which suggests that its use for treating several inflammatory diseases, particularly seborrheic dermatitis, acne, ATD and psoriasis, can be particularly beneficial (Lodzki et al. 2003).
Likewise, also nanometric emulsions have gained significant recognition owing to their physicochemical, thermodynamic, and organoleptic characteristics. They can be defined as a thermodynamically stable, transparent, single-phase oil–water mixture with nanosized particles. By having a lipid domain, they are able to interact with and penetrate the stratum corneum and maintain lipophilic compounds solubilized, contributing to its permeation and bioavailability. Also, by offering a huge surface area, they add to a large area of absorption of the active compounds (Vanti et al. 2021). The combination and concentrations of surfactant, cosurfactant and oil phase must be studied and adjusted to each compound to obtain the most appropriate results in terms of physicochemical properties, particle size, pH, stability, and skin permeation (Park et al. 2021). This must be done in order to optimize nanometric emulsions’ advantages, such as the possibility of little cutaneous irritation, great thermodynamic stability and the facility and reproducibility of its production (Vanti et al. 2021). Cannabinoid-loaded nanometric emulsions have been studied as delivery systems capable of improving cannabinoids’ stability and their delivery through the skin. NPs size in nanometric emulsions is one of the major factors influencing the flux through the skin. Additionally, the weight ratio of surfactant-cosurfactant and the nanometric emulsions pH, have a brutal impact on their diffusion through the skin, suitability for skin application and on their stability (Park et al. 2021). Lewińska and its colleagues developed a nanometric oil-in-water (O/W) emulsion stabilized with polyethylene glycol (PEG) sorbitan monooleate and surfactin. The use of PEG enables an improvement in the solubility of CBD and to obtain a smaller particle size. Nevertheless, when used alone, it turned out the pH was too low and not compatible for application on the skin. In turn, surfactin shifts the formulations pH to neutral, making it more compatible and safer for the skin. Furthermore, as it has polar compounds, it increases the zeta potential in the interfacial film, which, by acting as a stabilizing barrier, prevents the aggregation of particles and thus improves stability. It is the combination of both surface active agents in equal amounts, but at specific concentrations, that presents the most satisfactory results, in terms of polydispersity index, with optimum values of 0.3 and toxicity, showing no cytotoxicity in in vitro studies in human normal dermal fibroblasts and HaCaT cells. It also gave origin to optimum stability, with no phase separation, creaming or particle size change being observed during the 30 observation days. When studying the in vivo human skin response to the developed CBD nanometric emulsion, they observed an improved hydration status, mainly in zone U, but also in zone T. This makes it not only an interesting formulation for cosmetic application, but also a delivery system that should be studied in the treatment of various skin diseases, including ATD and acne (Lewińska 2021). Also in a different study, and compared to a cannabis ethanol extract (positive control), the lowest mean droplet size of cannabinoid-loaded nanometric emulsions of THCA and CBDA (89.62 nm for THCA and 84.72 nm for CBDA) showed a flux increase of approximately 17- and 12-fold, respectively. Also, pH-adjusted nanometric emulsions enhanced CBDs formulation stability, as they have been shown to decompose more slowly than the positive control (Park et al. 2021).
Despite all the mentioned CBD-nanometric emulsions advantages, among their disadvantages for skin delivery is its low viscosity, not being the most suitable for application in the skin since it is advantageous an to have an adequate retention of the product in the skin (Benigni et al. 2018). For this reason, the development of a nanoemulgel (NEG) was carried out in order to improve the physical–chemical, sensory, dermatological, and organoleptic characteristics (Fig. 8). In terms of viscosity, NEG has demonstrated to have a similar viscosity to that of a CBD-gel, 439,000 vs 518,500 mPa.s, respectively. Nevertheless, it proved to be a more stable formulation by presenting a decrease of viscosity at high rotational speed slower than the gel, and similar viscosity values in the up and down ramp (392,000 and 390,000 mPa.s), unlike the gel (628,000 and 595,000 mPa.s). Furthermore, CBD-NEG has also shown a prolonged and controlled release and absorption, with a consequent smaller amount of active ingredient diffusion to the acceptor compartment, in a 24 h in vitro release test (89.96 μg/cm2), compared to the conventional CBD-gel (128.13 μg/cm2). It also showed much slower CBD release, showed by the 3 h extra necessary to detect CBD in the acceptor compartment, by the 67% lower amount of CBD that permeated the skin after 24 h, and by the half amount of drug absorbed and accumulated in the skin at the end of the study. These results demonstrated that the NEG has characteristics that make it possible to associate the retention of CBD in the skin, while avoiding its transdermal delivery, like is desired for the local treatment of various skin conditions (Vanti et al. 2021). Although nanometric emulsions studies were conducted with cannabis ethanolic extracts rich in tetrahydrocannabinolic acid and CBDA, some conclusions possibly may be drawn for CBD-loaded nanometric emulsions based on the obtained results. This is due to the fact that CBD is a compound structurally similar to CBDA, even though further studies may be carried out in order to conclude about the formulation of CBD-loaded nanometric emulsions. Accordingly, formulation of CBD in nanometric emulsions or NEG, depending on the intended objectives of the formulation and the condition to be treated, may represent a bright future for CBD delivery systems, not only by improving several properties but also by increasing safety and reproducibility.
a The process steps for formulating a nanoemulsion and a nanoemulgel and the subsequent loading with CBD; b Scanning Electron Microscope images of CBD-nanoemulsion (A) and CBD-nanoemulgel (B); c CBD release profile from the CBD-nanoemulgel (CBD-MEgel) and CBD-gel over 24 h; d Variation of average droplet size and polydispersity index (PdI) of CBD-nanoemulgel over a 3-month period (Adapted from (Vanti et al. 2021))
Marketed cannabidiol-containing dermatological formulations
In recent years, CBD has been one of the main trends in the world of cosmetics. According to Future Market Insights' report "CBD Skin Care Market Overview (2022–2028)", it is estimated that by 2022 the global sales of CBD-based skin care products will reach US$ 2,359.5 Mn and it is predicted that by 2028 this market will experience a 28% growth (Insights and Overview 2022). Among the several commercialized cosmetic products containing CBD in their composition, the most notable are creams, lotions, balms oils and serums (Table 6). Although the CBD strength may be below the therapeutic window in some cases, or even not disclosed in other cases, there have been an increasing number of new products coming out with the most diverse and innovative formulations. These include claims as potential adjuvants in skin hydration, anti-ageing, photoprotection, acne and modulation of hair growth on account of their anti-inflammatory, moisturizing, antioxidant, sebostatic and healing properties (Jhawar et al. 2019).
The ongoing formulation development containing CBD and other compounds with attractive and synergetic biological activities aims to bring to fruition promising products for different skin conditions and skin types. Of the different ingredients used, essential oils such as jojoba, lavender, bergamot and jasmine oils stand out. Other non-CBD ingredients have also shown relevance, such as coconut oil, olive oil, sunflower oil, shea butter and Aloe vera gel. One company that is worth mentioning is Lula™, which combined CBD with Butyrospermum parkii (shea butter) and different essential oils, including, among others, lavender, bitter orange, bergamot, lemon, jasmine and rosemary in one of its lotions, the hand and body lotion, and which has yet developed potion serum by using a wide range of essential oils (Gleason-Allured et al. 2022). Another company is Saint Jane®, which formulated luxury beauty serum allying CBD to sunflower seeds oil (Helianthus annuus), shea butter and yet several essential oils, such as rosehip, jojoba, rose and rosemary (Xue 2022). On the other had, the company Chantecaille® bet on Aloe barbadensis leaf juice, olive oil, shea butter and sunflower oil properties to optimize CBD 300 face and body cream (Behrens 2022). Moreover, a different company, Deawy®, added, in addition to CBD and shea butter, coconut oil to becalm burn balm (Elitou 2020).
Furthermore, there are several products containing different vitamins that have already been launched on the market, such as: the C-drops, by Saint Jane®, and vitamin C and CBD skin elixir, by Botanika Life™, with vitamin C (Xue 2022; Schlabach 2022); and CBD body lotion, by Lazarus Naturals™, beyond balm, by Lula™, and calm, by Calm by Wellness Hemp®, with vitamin E (Gleason-Allured et al. 2022; Davenport 2022). In turn, Envy CBD® has not bet on the application of only one type of vitamin, but on the combination of vitamins E, C and B5 to develop CBD Face Cream. The truth is that other common and highly sought-after ingredients in the dermocosmetic industry, such as hyaluronic acid, retinol, resveratrol and squalene have been added to CBD-based products. The proof of this are: acid mantle repair and line refine by Lord Jones™; CBD face crème, by Green Gorilla™, which has in its composition the coenzyme Q10 (ubiquinone), resveratrol and vitamin E (Davenport 2022); and the unblemished + salicylic acid acne treatment, which Botanika Life™ formulated containing, in addition to salicylic acid, hyaluronic acid, allantoin, squalene and vitamins E and C (Schlabach 2022).
Given the CBD's potential to modulate hair growth, CBD shampoos and serums and other hair and scalp products are now available and gaining popularity. Of particular interest is Vagemour's GRO + advanced hair serum which, by microencapsulating CBD and using mung bean, red clover, curcumin and Nicotiana benthamiana extracts, claims to strengthen hair roots and increase hair volume, density, and thickness (Latimer 2022). Another interesting product is Cannabae soothing shampoo, developed by Sexyhair® containing 99% pure CBD and cold-pressed avocado and macadamia oil, as a revitalizing and repairing shampoo for damaged hair and as a scalp moisturizer (Scianna 2022).
Despite the huge growth that the CBD market has undergone and the popularity that these products have achieved in recent decades, it should be borne in mind that there are also CBD products that remain on the market and whose efficacy, safety and quality have not been subjected to any kind of control, potentially carrying significant consumer safety risks. Nevertheless, considering the most recent developments observed in this industry, some efforts have been made to clarify the regulatory framework for cannabis and its products. In this way, and with the CBD price decline that has been observed, it is expected that the amount of products commercialized will continue to increase and that new formulations will keep being developed so that the benefits of this phytocannabinoid can be better exploited and, thus, valorized (Lessard 2022).
Safety of cannabidiol-containing dermopharmaceutical applications: regulatory and toxicological aspects
In recent years, cannabis products have been experiencing monumental growth across the world (Leas et al. 2019; EMCDDA, Low-THC 2020). These products, which come in many different forms and compositions (Hughes et al. 2022) include different topical formulations such as gels, balms, and lotions (McGregor et al. 2020). However, regulatory and legislative discrepancies exist and have been observed to increase in different countries and continents regarding the use of cannabis for medicinal, non-medicinal, and recreational purposes (Cross and Cock 2020). On one hand, in the European Union and most of the other European countries, Australia, Canada, and New Zealand, the use of medical cannabis is legal with a medical prescription and, in some countries, subject to country-specific inclusion criteria (McGregor et al. 2020). On the other hand, in the United States of America there are plenty of questions and doubts that emerge regarding the legal status of these products as a result of the differences that exist at the state and federal level (Mead 2017). In the US, CBD-containing products, in state terms, are legal in all states if the CBD is derived from hemp (which has scant amounts of THC), or in states where marijuana is legal for recreational and medicinal purposes (Lucas et al. 2018). In federal terms, if the Drug Enforcement Administration had previously classified CBD products as Schedule I (not accepted for any medical use and propensity for abuse), in 2018 it alleviated the classification criteria for products containing less than 0.3% THC and which are FDA approved, making them Schedule V (very low potential for abuse and with limited amounts of specific narcotics) (McGregor et al. 2020; Mead 2017). However, if within the US there are frequently doubts about the legal status of CBD products, also in the European Union there are some discrepancies resulting from the differences inherent to each country and from the adaptation of European laws to each one of them (Hughes et al. 2022). That is the case of the maximum THC limit in each CBD product: if for European Union countries there can be no more than 0.2% THC (EMCDDA 2017), in Switzerland the limit is extended to 1% (Ordonnance 2011). However, according to EEC Regulation (EU) 2022/1393 of August 11, 2022, the threshold levels for hemp seeds and derived products are set in terms of the sum of THCA and THC, expressed in THC equivalents, to 3.0 and to 7.5 mg/kg in hemp seed oil (EUR-LEX. Regulamento (UE) 2022). In turn, there are still countries where cannabis for non-medical purposes remains illegal and others where the use of any cannabis product is prohibited for any purpose, such as Japan (McGregor et al. 2020). Nevertheless, there are already approved medical CBD-containing products. One of them is Epidiolex®, containing only CBD, approved by the FDA and EMA, for the treatment of the rare forms of pediatric epilepsy, Dravet syndrome or Lennox-Gastaut syndrome (Devinsky et al. 2017). Studies with healthy volunteers showed increases in ALT, AST, ALP and GGT at doses of Epidiolex® of 20 mg/kg b.w. per day. However, increases in ALT and AST were also seen in a study with 4.3 mg/kg b.w. per day. In patients with epilepsy that were concomitantly treated also with other antiepileptic medication, increased liver enzymes were reported in the same dose range (Turck et al. 2022). The other is Sativex®, an orobuccal spray containing equimolar concentrations of THC and CBD, approved in the European Union, for multiple sclerosis spasticity (McGregor et al. 2020).
Most of the doubts and uncertainties that remain regarding the regulation of CBD in different countries are largely due to the lack of control in the production, distribution, quality control, and effectiveness of most products containing CBD, but also to the scarcity of scientific evidence on the effects of chronic CBDs use (Hazekamp 2018) and owing to frequent incorrect labeling (Li et al. 2021). In part, there is insufficient quality control from production to manufacturing that results in the presence of contaminants, both intentionally added (such as pesticides and metals) (Busse et al. 2008) and unintentionally present bacteria, fungi (McKernan et al. 2016) and heavy metals (Linger et al. 2002). On the other hand, it is observed that most products contain doses of CBD much lower than those that are clinically effective (Millar et al. 2019). Additionally, the claimed amounts of CBD can be higher or lower than what actually exists and the labeled THC concentration might be underestimated (Liebling et al. 2022). Thus, the safety and toxicity associated with these products are, in addition to being related to the CBD’s biological activities, also related to the flaws inherent to the lack of control and harmonized regulation.
CBD has relatively high safety and tolerability concerning its administration by different routes. However, although new delivery systems and administration routes are increasingly being studied, most of the known data and information about this phytocannabinoid is based on studies concerning its oral administration, for which many questions remain to be answered. This happens mainly because the existing toxicological studies, both in vivo and in vitro, vary in terms of preparations or extract type and concentration of CBD and other compounds naturally present in the plant or resulting from the extraction process (Turck et al. 2022; Taylor et al. 2018). Nevertheless, it has been observed that the doses at which CBD safely exerts therapeutic activity are between 300 and 1,500 mg (Millar et al. 2019), although doses up to 6,000 mg showed relatively good tolerability (Taylor et al. 2018). Despite all its benefits, some concerns have also been raised in terms of its toxicity and potential side effects in cellular and animal studies and clinical trials. CBD has demonstrated toxicity to the reproductive system in a 34-day study in rats where doses of 15 and 30 mg/kg/day of CBD altered testosterone levels, different stages of spermatogenesis, and daily sperm conformation and production (Carvalho et al. 2018). Additionally, it has also exhibited liver toxicity, through liver hypertrophy, significant changes in lipid metabolism and through an increase of hepatic enzymes and total bilirubin levels in mouse models and human studies (Turck et al. 2022; Ewing et al. 2019). Nevertheless, hepatic toxicity is not yet fully disclosed since it is mostly used in association with anticonvulsants, which may exhibit drug-drug interactions in vivo. In addition, there are several adverse effects arising from the oral administration of CBD among which stand out as the most common, such as somnolence (Izgelov et al. 2020), diarrhea, vomiting, and upper respiratory tract infections (Devinsky et al. 2017). Thereby, even though cutaneous administration may induce local adverse effects, like skin dryness and pain (Scheffer et al. 2021) and rash, as observed for two different CBD gels, it has been demonstrated that topical CBD may reduce gastrointestinal AEs compared to the oral route (Scheffer et al. 2021). It has also been proven that other three topical formulations (gel, balm and cream) have not induced skin irritation, sensitization and phototoxicity (Maghfour et al. 2021), demonstrating that transdermal and topical route might be a great alternative for a safe, effective and well tolerated CBD administration.
Whereas much of the available information stems from studies concerning oral administration, it is worth noting that the safety and toxicity of CBD depend on its dose, frequency of administration, route of administration, and the amount of other compounds present in the formulations, and that there are significant data gaps that have to be clarified in the future with more research in humans and experimental animals (Turck et al. 2022).
Conclusions and future perspectives
Nowadays there is an urgent need to find or improve therapeutic solutions for new emerging diseases. The endocannabinoid system, present throughout the body, is involved in homeostasis maintenance and in the development of several diseases. There is already an important amount of scientific evidence which prove the benefits and therapeutic applications of CBD. CBD has several skin biological properties that make it a compound that can simultaneously act on different targets of multifactorial diseases such as ATD, psoriasis, acne, epidermolysis bullosa, systemic sclerosis, seborrheic dermatitis, scalp psoriasis, androgenetic alopecia and melanoma leading to better outcomes and improved patient quality of life.
Nevertheless, the physicochemical characteristics of CBD, mainly its extreme hydrophobic nature, make it a challenging molecule for topical administration. Therefore, to improve the delivery of CBD into the skin and maximize its properties, several strategies and delivery systems have been developed. These strategies have included improved conventional semi-solid formulations, such as cryogels, hydrogels and ethanolic gels, and formulations containing penetration enhancers, comprising Transcutol®, isopropyl myristate, oleic acid, LA, DMSO, NMP or PEG-400. CBD has also been incorporated in nanosized delivery systems, such NPs, ethosomes, polymeric mycelles, pickering emulsions, nanometric emulsions and NEGs, with varying composition.
Nevertheless, despite current state of knowledge on the dermatological value of CBD, many gaps exist regarding therapeutic mechanisms of action, minimum effective doses, clinical studies, and most importantly safety and regulation. Hence, many studies have yet to be carried out to elucidate these issues. But given the growth of cannabis-based medicines observed in the past years, it is expected that phytocannabinoids and their analogs will continue to be a preferred focus of scientific research.
Abbreviations
- 2-AG:
-
2-Arachidonoylglycerol
- 4-HNE:
-
4-Hydroxy-2-nonenal
- ADR:
-
Adenosine receptor
- AEA:
-
Arachidonoylethanolamine
- AQP3:
-
Aquaporin-3
- ATD:
-
Atopic dermatitis
- βCD:
-
Beta-cyclodextrin
- CB1R:
-
Cannabidiol receptor type-1
- CB2R:
-
Cannabidiol receptor type-2
- CBD:
-
Cannabidiol
- CBDA:
-
Cannabidiolic acid
- CH/CL:
-
Chitosan and collagen
- CI:
-
Creaming index
- CYP:
-
Cytochrome P450
- DL:
-
Drug loading
- DMSO:
-
Dimethyl sulfoxide
- DOD:
-
Degree of deacetylation
- DWC:
-
Dermal water content
- ECS:
-
Endocannabinoid system
- EC:
-
Endocannabinoid
- EE:
-
Encapsulation efficiency
- EMA:
-
European medicines agency
- ESKAPE:
-
Enterococcus faecium, Staphylococcus aureus; Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter Spp
- FDA:
-
Food and drug administration
- GPR55:
-
G protein-coupled receptor 55
- Gram-:
-
Gram-negative
- Gram + :
-
Gram-positive
- HEC:
-
2-Hydroxyethyl cellulose
- HFL:
-
Hair follicle
- IL:
-
Interleukine
- LA:
-
Lactic acid
- MDA:
-
Malondialdehyde
- N/A:
-
Not available
- NEG:
-
Nanoemulgel
- NF-κB:
-
Nuclear factor-kappa B
- NMP:
-
N-Methyl-2-pyrrolidone
- NP:
-
Nanoparticle
- NRF2:
-
Nuclear factor erythroid-2 related factor
- O/W:
-
Oil-in-water
- ORS:
-
Outer root sheath
- OA:
-
Olivetolic acid
- PEG:
-
Polyethylene glycol
- PMB:
-
Polymyxin B
- PPAR-γ:
-
Peroxisome proliferator-activated receptor gamma
- PPG:
-
Propylene glycol
- ROS:
-
Reactive oxygen species
- SGM:
-
Sphingomyelin
- TGF-β1:
-
Transforming growth factor beta1
- THC:
-
Delta-9-Tetrahydrocannabinol
- TNF-α:
-
Tumor necrosis factor-alpha
- TRP:
-
Transient receptor potential channel
- TRPAI:
-
Transient receptor potential channel ankyrin 1 subtype
- TRPM:
-
Transient receptor potential channel melastatin subtype
- TRPM8:
-
Transient receptor potential channel subfamily melastin member 8
- TRPV:
-
Transient receptor potential channel, vanilloid subtype
- UV:
-
Ultraviolet
- ZnO:
-
Zinc oxide
References
Elitou, E. This "Becalm" Balm Uses CBD to Soothe Everything from Burns to Stressed-out Skin. 2020 [cited 2022 20 de agosto ]; Available from: https://www.byrdie.com/deawy-cbd-burn-balm-launch-5085906.
Xue F, Exclusive: Saint Jane Debuts New "C-Drops" Serum. 2022 [cited 2022 20 de agosto ]; Available from: https://www.byrdie.com/saint-jane-c-drops-serum-4800703.
Abdel-Hafez SM, Hathout RM, Sammour OA (2018) Tracking the transdermal penetration pathways of optimized curcumin-loaded chitosan nanoparticles via confocal laser scanning microscopy. Int J Biol Macromol 108:753–764. https://doi.org/10.1016/j.ijbiomac.2017.10.170
Abichabki N, Zacharias LV, Moreira NC, Bellissimo-Rodrigues F, Moreira FL, Benzi JRL, Ogasawara TMC, Ferreira JC, Ribeiro CM, Pavan FR, Pereira LRL, Brancini GTP, Braga GUL, Zuardi AW, Hallak JEC, Crippa JAS, Lanchote VL, Canton R, Darini ALC, Andrade LN (2022) Potential cannabidiol (CBD) repurposing as antibacterial and promising therapy of CBD plus polymyxin B (PB) against PB-resistant gram-negative bacilli. Sci Reports. https://doi.org/10.1038/s41598-022-10393-8
Aguillon AR, Leao RAC, Miranda LSM, de Souza R (2021) Cannabidiol discovery and synthesis-a target-oriented analysis in drug production processes. Chem-a Eur J 27(18):5577–5600. https://doi.org/10.1002/chem.202002887
Alvarez-Roman R, Barre G, Guy RH, Fessi H (2001) Biodegradable polymer nanocapsules containing a sunscreen agent: preparation and photoprotection. Eur J Pharm Biopharm 52(2):191–195. https://doi.org/10.1016/s0939-6411(01)00188-6
Alvarez-Roman R, Naik A, Kalia YN, Guy RH, Fessi H (2004) Enhancement of topical delivery from biodegradable nanoparticles. Pharm Res 21(10):1818–1825. https://doi.org/10.1023/B:PHAM.0000045235.86197.ef
Aparicio-Blanco J, Sebastián V, Benoit JP, Torres-Suárez AI (2019) Lipid nanocapsules decorated and loaded with cannabidiol as targeted prolonged release carriers for glioma therapy: In vitro screening of critical parameters. Eur J Pharm Biopharm 134:126–137. https://doi.org/10.1016/j.ejpb.2018.11.020
Appendino G, Gibbons S, Giana A, Pagani A, Grassi G, Stavri M, Smith E, Rahman M (2008) Antibacterial cannabinoids from cannabis sativa: a structure-activity study. J Nat Prod 71(8):1427–1430. https://doi.org/10.1021/np8002673
Armstrong JL, Hill DS, McKee CS, Hernandez-Tiedra S, Lorente M, Lopez-Valero I, Anagnostou ME, Babatunde F, Corazzari M, Redfern CPF, Velasco G, Lovat PE (2015) Exploiting cannabinoid-induced cytotoxic autophagy to drive melanoma cell death. J Investig Dermatol 135(6):1629–1637. https://doi.org/10.1038/jid.2015.45
Atalay S, Jarocka-Karpowicz I, Skrzydlewska E (2020a) Antioxidative and anti-inflammatory properties of cannabidiol. ANTIOXIDANTS. https://doi.org/10.3390/antiox9010021
Atalay S, Dobrzynska I, Gegotek A, Skrzydlewska E (2020b) Cannabidiol protects keratinocyte cell membranes following exposure to UVB and hydrogen peroxide. Redox Biol. https://doi.org/10.1016/j.redox.2020.101613
Atalay S, Gegotek A, Skrzydlewska E (2021a) Protective effects of cannabidiol on the membrane proteome of uvb-irradiated keratinocytes. Antioxidants. https://doi.org/10.3390/antiox10030402
Atalay S, Gegotek A, Domingues P, Skrzydlewska E (2021b) Protective effects of cannabidiol on the membrane proteins of skin keratinocytes exposed to hydrogen peroxide via participation in the proteostasis network. Redox Biol. https://doi.org/10.1016/j.redox.2021.102074
Azuma K, Koizumi R, Izawa H, Morimoto M, Saimoto H, Osaki T, Ito N, Yamashita M, Tsuka T, Imagawa T, Okamoto Y, Inoue T, Ifuku S (2019) Hair growth-promoting activities of chitosan and surface-deacetylated chitin nanofibers. Int J Biol Macromol 126:11–17. https://doi.org/10.1016/j.ijbiomac.2018.12.135
Baswan SM, Klosner AE, Glynn K, Rajgopal A, Malik K, Yim S, Stern N (2020) Therapeutic potential of cannabidiol (cbd) for skin health and disorders. Clin Cosmet Investig Dermatol 13:927–942. https://doi.org/10.2147/CCID.S286411
Behrens, M. Chantecaille packs cbd and cannabis into redness reducing moisturizer. [cited 2022 20 de agosto ]; Available from: https://www.cosmeticsandtoiletries.com/cosmetic-ingredients/moisturizing/news/21843898/chantecaille-packs-cbd-and-cannabis-into-redness-reducing-moisturizer.
Bellini A, Marini MA, Bianchetti L, Barczyk M, Schmidt M, Mattoli S (2012) Interleukin (IL)-4, IL-13, and IL-17A differentially affect the profibrotic and proinflammatory functions of fibrocytes from asthmatic patients. Mucosal Immunol 5(2):140–149. https://doi.org/10.1038/mi.2011.60
Benigni M, Pescina S, Grimaudo MA, Padula C, Santi P, Nicoli S (2018) Development of microemulsions of suitable viscosity for cyclosporine skin delivery. Int J Pharm 545(1–2):197–205. https://doi.org/10.1016/j.ijpharm.2018.04.049
Berhrens, M. Vital You CBD Mists Tone, Hydrate Skin with Aromatherapy. [cited 2022 20 de agosto ]; Available from: https://www.cosmeticsandtoiletries.com/formulas-products/skin-care/news/21844105/vital-you-cbd-mists-tone-hydrate-skin-with-aromatherapy.
Bhinge SD, Bhutkar MA, Randive DS, Wadkar GH, Todkar SS, Savali AS, Chittapurkar HR (2021) Screening of hair growth promoting activity of Punica granatum L. (pomegranate) leaves extracts and its potential to exhibit antidandruff and anti-lice effect. Heliyon. https://doi.org/10.1016/j.heliyon.2021.e06903
Biernacki M, Brzoska MM, Markowska A, Galazyn-Sidorczuk M, Cylwik B, Gegotek A, Skrzydlewska E (2021) Oxidative stress and its consequences in the blood of rats irradiated with UV: protective effect of cannabidiol. Antioxidants. https://doi.org/10.3390/antiox10060821
Biro T, Bodo E, Telek A, Geczy T, Tychsen B, Kovacs L, Paus R (2006) Hair cycle control by vanilloid receptor-1 (TRPV1): Evidence from TRPV1 knockout mice. J Investig Dermatol 126(8):1909–1912. https://doi.org/10.1038/sj.jid.5700321
Biswas DK, Cruz AP, Gansberger E, Pardee AB (2000) Epidermal growth factor-induced nuclear factor κB activation: a major pathway of cell-cycle progression in estrogen-receptor negative breast cancer cells. Proc Natl Acad Sci 97(15):8542–8547. https://doi.org/10.1073/pnas.97.15.8542
Blaskovich MAT, Kavanagh AM, Elliott AG, Zhang B, Ramu S, Amado M, Lowe GJ, Hinton AO, Pham DMT, Zuegg J, Beare N, Quach D, Sharp MD, Pogliano J, Rogers AP, Lyras D, Tan L, West NP, Crawford DW, Peterson ML, Callahan M, Thurn M (2021) The antimicrobial potential of cannabidiol. Commun Biol. https://doi.org/10.1038/s42003-020-01530-y
Bodade SS, Shaikh KS, Kamble MS, Chaudhari PD (2013) A study on ethosomes as mode for transdermal delivery of an antidiabetic drug. Drug Delivery 20(1):40–46. https://doi.org/10.3109/10717544.2012.752420
Bodó E, Bíró T, Telek A, Czifra G, Griger Z, Tóth BI, Mescalchin A, Ito T, Bettermann A, Kovács L, Paus R (2005) A hot new twist to hair biology. Am J Pathol 166(4):985–998. https://doi.org/10.1016/s0002-9440(10)62320-6
Borbíró I, Lisztes E, Tóth BI, Czifra G, Oláh A, Szöllősi AG, Szentandrássy N, Nánási PP, Péter Z, Paus R, Kovács L, Bíró T (2011) Activation of transient receptor potential vanilloid-3 inhibits human hair growth. J Investig Dermatol 131(8):1605–1614. https://doi.org/10.1038/jid.2011.122
Bourji K, Meyer A, Chatelus E, Pincemail J, Pigatto E, Defraigne JO, Singh F, Charlier C, Geny B, Gottenberg JE, Punzi L, Cozzi F, Sibilia J (2015) High reactive oxygen species in fibrotic and nonfibrotic skin of patients with diffuse cutaneous systemic sclerosis. Free Radical Biol Med 87:282–289. https://doi.org/10.1016/j.freeradbiomed.2015.07.002
Bow EW, Rimoldi JM (2016) The structure-function relationships of classical cannabinoids: CB1/CB2 modulation. Perspect Med Chem. https://doi.org/10.4137/pmc.s32171
Brownhill VR, Huddleston E, Bell A, Hart J, Webster I, Hardman MJ, Wilkinson HN (2021) Pre-clinical assessment of single-use negative pressure wound therapy during in vivo porcine wound healing. Adv Wound Care 10(7):345–356. https://doi.org/10.1089/wound.2020.1218
Burch R, Mortuza A, Blumenthal E, Mustafa A (2021) Effects of cannabidiol (CBD) on the inhibition of melanoma cells <i>in vitro</i>. J Immunoassay Immunochem 42(3):285–291. https://doi.org/10.1080/15321819.2020.1862863
Busse FP, Fiedler GM, Leichtle A, Hentschel H, Stumvoll M (2008) Lead poisoning due to adulterated marijuana in leipzig. Dtsch Arztebl Int. https://doi.org/10.3238/arztebl.2008.0757
Carvalho RK, Santos ML, Souza MR, Rocha TL, Guimaraes FS, Anselmo-Franci JA, Mazaro-Costa R (2018) Chronic exposure to cannabidiol induces reproductive toxicity in male Swiss mice (vol 38, pg 1215, 2018). J Appl Toxicol 38(12):1545–1545. https://doi.org/10.1002/jat.3731
Casares L, Garcia V, Garrido-Rodriguez M, Millan E, Collado JA, Garcia-Martin A, Penarando J, Calzado MA, de la Vega L, Munoz E (2020) Cannabidiol induces antioxidant pathways in keratinocytes by targeting BACH1. Redox Biol. https://doi.org/10.1016/j.redox.2019.101321
Casiraghi A, Musazzi UM, Centin G, Franze S, Minghetti P (2020) Topical administration of cannabidiol: influence of vehicle-related aspects on skin permeation process. Pharmaceuticals. https://doi.org/10.3390/ph13110337
Castillo A, Tolon MR, Fernandez-Ruiz J, Romero J, Martinez-Orgado J (2010) The neuroprotective effect of cannabidiol in an in vitro model of newborn hypoxic-ischemic brain damage in mice is mediated by CB2 and adenosine receptors. Neurobiol Dis 37(2):434–440. https://doi.org/10.1016/j.nbd.2009.10.023
Chadwick, M.R. 11 Legit CBD oils to use from head-to-toe. 2022 [cited 2022 20 de agosto ]; Available from: https://www.byrdie.com/best-cbd-oils-4796948.
Chelliah MP, Zinn Z, Khuu P, Teng JMC (2018) Self-initiated use of topical cannabidiol oil for epidermolysis bullosa. Pediatr Dermatol 35(4):E224–E227. https://doi.org/10.1111/pde.13545
Chiocchetti R, De Silva M, Aspidi F, Cunha RZ, Gobbo F, Tagliavia C, Sarli G, Morini M (2022) Distribution of cannabinoid receptors in keratinocytes of healthy dogs and dogs with atopic dermatitis. Front Vet Sci. https://doi.org/10.3389/fvets.2022.915896
Choi WH, Do Park H, Baek SH, Chu JP, Kang MH, Mi YJ (2008) Cannabidiol induces cytotoxicity and cell death via apoptotic pathway in cancer cell lines. Biomol Ther. https://doi.org/10.4062/biomolther.2008.16.2.087
Correia-Sa IB, Carvalho CM, Serrao PV, Loureiro AI, Fernandes-Lopes C, Marques M, Vieira-Coelho MA (2020) A new role for anandamide: defective link between the systemic and skin endocannabinoid systems in hypertrophic human wound healing. Sci Reports. https://doi.org/10.1038/s41598-020-68058-3
Cross JH, Cock H (2020) A perspective on cannabinoids for treating epilepsy: do they really change the landscape? Neuropharmacology. https://doi.org/10.1016/j.neuropharm.2019.107861
Curcio, A., F. Nano, M. Pironti, N. Marchitto, A. Pannozzi, L. Bilo, A. Romano, and R. G. (2021) In vitro study evaluating the influence of vehicle in the permeability process of a topical composition containing cannabis sativa oil, escin, bromelain, glucosamine sulphate, methylsulfonylmethane, methylsalicylate and boswellia extract, designed for local treatment of musculoskeletal painful and inflammatory conditions. Journal of Clinical Chemistry and Laboratory Medicine https://doi.org/10.35248/jcclm.21.4.189.
Davenport, S. CBD skin cream: How to use and best options. [cited 2022 20 de agosto ]; Available from: https://www.medicalnewstoday.com/articles/cbd-skin-cream#product-list.
de Almeida DL, Devi LA (2020) Diversity of molecular targets and signaling pathways for CBD. Pharmacol Res Perspect 8(6):e00682. https://doi.org/10.1002/prp2.682
del Rio C, Millan E, Garcia V, Appendino G, DeMesa J, Munoz E (2018a) The endocannabinoid system of the skin. Biochemical Pharmacology, A potential approach for the treatment of skin disorders. https://doi.org/10.1016/j.bcp.2018.08.022
del Rio C, Cantarero I, Palomares B, Gomez-Canas M, Fernandez-Ruiz J, Pavicic C, Garcia-Martin A, Bellido ML, Ortega-Castro R, Perez-Sanchez C, Lopez-Pedrera C, Appendino G, Calzado MA, Munoz E (2018b) VCE-004.3, a cannabidiol aminoquinone derivative, prevents bleomycin-induced skin fibrosis and inflammation through PPAR gamma- and CB2 receptor-dependent pathways. British J Pharmacol 175(19):3813–3831. https://doi.org/10.1111/bph.14450
Del Rio C, Ruiz-Pino F, Prados ME, Fiebich BL, Tena-Sempere M, Munoz E (2022) Cannabidiol markedly alleviates skin and liver fibrosis. Front Pharmacol 13:981817. https://doi.org/10.3389/fphar.2022.981817
De Petrocellis L, Ligresti A, Moriello AS, Allara M, Bisogno T, Petrosino S, Stott CG, Di Marzo V (2011) Effects of cannabinoids and cannabinoid-enriched cannabis extracts on TRP channels and endocannabinoid metabolic enzymes. Br J Pharmacol 163(7):1479–1494. https://doi.org/10.1111/j.1476-5381.2010.01166.x
Devinsky O, Cross JH, Laux L, Marsh E, Miller I, Nabbout R, Scheffer IE, Thiele EA, Wright S (2017) Trial of cannabidiol for drug-resistant seizures in the dravet syndrome. N Engl J Med 376(21):2011–2020. https://doi.org/10.1056/nejmoa1611618
Elbaz M, Nasser MW, Ravi J, Wani NA, Ahirwar DK, Zhao H, Oghumu S, Satoskar R, Abhay K, Shilo WEC, Ganju K, Ramesh, (2015) Modulation of the tumor microenvironment and inhibition of EGF/EGFR pathway: novel anti-tumor mechanisms of cannabidiol in breast cancer. Mol Oncol. https://doi.org/10.1016/j.molonc.2014.12.010
EMCDDA (2017) Cannabis legislation in Europe - an overview p 32.
EMCDDA (2020) Low-THC cannabis products in Europe
Ewing LE, Skinner CM, Quick CM, Kennon-McGill S, McGill MR, Walker LA, ElSohly MA, Gurley BJ, Koturbash I (2019) Hepatotoxicity of a cannabidiol-rich cannabis extract in the mouse model. Molecules. https://doi.org/10.3390/molecules24091694
Fink, H. Beekman 1802 Launches CBD Goat Milk Body Soap. [cited 2022 20 de agosto ]; Available from: https://www.cosmeticsandtoiletries.com/formulas-products/bath-shower/news/21861939/beekman-1802-launches-cbd-goat-milk-body-soap.
Fraguas-Sanchez AI, Torres-Suarez AI, Cohen M, Delie F, Bastida-Ruiz D, Yart L, Martin-Sabroso C, Fernandez-Carballido A (2020) PLGA nanoparticles for the intraperitoneal administration of cbd in the treatment of ovarian cancer. Pharmaceutics, In Vitro and In Ovo Assessment. https://doi.org/10.3390/pharmaceutics12050439
Gagne SJ, Stout JM, Liu EW, Boubakir Z, Clark SM, Page JE (2012) Identification of olivetolic acid cyclase from cannabis sativa reveals a unique catalytic route to plant polyketides. Proc Natl Acad Sci USA 109(31):12811–12816. https://doi.org/10.1073/pnas.1200330109
Gallily R, Yekhtin Z, Hanus LO (2018) The anti-inflammatory properties of terpenoids from cannabis. Cannabis Cannabinoid Res 3(1):282–290. https://doi.org/10.1089/can.2018.0014
Gegotek A, Atalay S, Domingues P, Skrzydlewska E (2019) The differences in the proteome profile of cannabidiol-treated skin fibroblasts following UVA or UVB irradiation in 2D and 3D cell cultures. Cells. https://doi.org/10.3390/cells8090995
Gegotek A, Atalay S, Skrzydlewska E (2021a) UV induced changes in proteome of rats plasma are reversed by dermally applied cannabidiol. Sci Reports. https://doi.org/10.1038/s41598-021-00134-8
Gegotek A, Jastrzab A, Dobrzynska M, Biernacki M, Skrzydlewska E (2021b) Exogenous antioxidants impact on UV-induced changes in membrane phospholipids and the effectiveness of the endocannabinoid system in human skin cells. Antioxidants. https://doi.org/10.3390/antiox10081260
Gegotek A, Atalay S, Rogowska-Wrzesinska A, Skrzydlewska E (2021c) The effect of cannabidiol on UV-Induced changes in intracellular signaling of 3D-cultured skin keratinocytes. Int J Mol Sci. https://doi.org/10.3390/ijms22031501
Ghodsi SZ, Abbas Z, Abedeni R (2015) Efficacy of oral itraconazole in the treatment and relapse prevention of moderate to severe seborrheic dermatitis: a randomized, placebo-controlled trial. Am J Clin Dermatol 16(5):431–437. https://doi.org/10.1007/s40257-015-0133-9
Gleason-Allured, J. SuperOrdinary launches lula CBD beauty. [cited 2022 20 de agosto ]; Available from: https://www.cosmeticsandtoiletries.com/cosmetic-ingredients/natural-sustainable/news/21863408/superordinary-launches-lula-cbd-beauty.
Gong XD, Sun CL, Abame MA, Shi WQ, Xie YC, Xu WB, Zhu FQ, Zhang Y, Shen JS, Aisa HA (2020) Synthesis of CBD and Its derivatives bearing various C4 ’-side chains with a late-stage diversification method. J Org Chem 85(4):2704–2715. https://doi.org/10.1021/acs.joc.9b02880
Gruber T, Robatel S, Kremenovic M, Bariswyl L, Gertsch J, Schenk M (2021) Cannabinoid receptor type-2 in B cells is associated with tumor immunity in melanoma. Cancers. https://doi.org/10.3390/cancers13081934
Gui H, Liu X, Wang ZW, He DY, Su DF, Dai SM (2014) Expression of cannabinoid receptor 2 and its inhibitory effects on synovial fibroblasts in rheumatoid arthritis. Rheumatology 53(5):802–809. https://doi.org/10.1093/rheumatology/ket447
Hamad H, Olsen BB (2021) Cannabidiol induces cell death in human lung cancer cells and cancer stem cells. Pharmaceuticals 14(11):1169. https://doi.org/10.3390/ph14111169
Hamelink C, Hampson A, Wink DA, Eiden LE, Eskay RL (2005) Comparison of cannabidiol, antioxidants, and diuretics in reversing binge ethanol-induced neurotoxicity. J Pharmacol Exp Ther 314(2):780–788. https://doi.org/10.1124/jpet.105.085779
Hammell DC, Zhang LP, Ma F, Abshire SM, McIlwrath SL, Stinchcomb AL, Westlund KN (2016) Transdermal cannabidiol reduces inflammation and pain-related behaviours in a rat model of arthritis. Eur J Pain 20(6):936–948. https://doi.org/10.1002/ejp.818
Hanus LO, Tchilibon S, Ponde DE, Breuer A, Fride E, Mechoulam R (2005) Enantiomeric cannabidiol derivatives: synthesis and binding to cannabinoid receptors. Org Biomol Chem 3(6):1116–1123. https://doi.org/10.1039/b416943c
Han KH, Lim S, Ryu J, Lee CW, Kim Y, Kang JH, Kang SS, Ahn YK, Park CS, Kim JJ (2009) CB1 and CB2 cannabinoid receptors differentially regulate the production of reactive oxygen species by macrophages. Cardiovasc Res 84(3):378–386. https://doi.org/10.1093/cvr/cvp240
Happyana N, Agnolet S, Muntendam R, Van Dam A, Schneider B, Kayser O (2013) Analysis of cannabinoids in laser-microdissected trichomes of medicinal cannabis sativa using LCMS and cryogenic NMR. Phytochemistry 87:51–59. https://doi.org/10.1016/j.phytochem.2012.11.001
Hazekamp A (2018) The trouble with CBD oil. Med Cannabis Cannabinoids 1(1):65–72. https://doi.org/10.1159/000489287
Heussler H, Cohen J, Silove N, Tich N, Bonn-Miller MO, Du W, O’Neill C, Sebree T (2019) A phase 1/2, open-label assessment of the safety, tolerability, and efficacy of transdermal cannabidiol (ZYN002) for the treatment of pediatric fragile X syndrome. J Neurodev Disord. https://doi.org/10.1186/s11689-019-9277-x
Hou YZ, Moreau F, Chadee K (2012) PPAR gamma is an E3 ligase that induces the degradation of NF kappa B/p65. Nat Commun. https://doi.org/10.1038/ncomms2270
Hughes B, Vandam L, Mounteney J, Griffiths P (2022) Regulatory approaches to cannabidiol in the European union: are market developments sowing the seeds of confusion? Addiction 117(1):3–4. https://doi.org/10.1111/add.15587
Iino M, Ehama R, Nakazawa Y, Iwabuchi T, Ogo M, Tajima M, Arase S (2007) Adenosine stimulates fibroblast growth factor-7 gene expression via adenosine A2b receptor signaling in dermal papilla cells. J Investig Dermatol 127(6):1318–1325. https://doi.org/10.1038/sj.jid.5700728
Ikarashi N, Shiseki M, Yoshida R, Tabata K, Kimura R, Watanabe T, Kon R, Sakai H, Kamei J (2021) Cannabidiol application increases cutaneous aquaporin-3 and exerts a skin moisturizing effect. Pharmaceuticals. https://doi.org/10.3390/ph14090879
Insights, F.M. CBD Skin Care Market Overview (2022–2028). [cited 2022 24 de agosto]; Available from: https://www.futuremarketinsights.com/reports/cbd-skin-care-market.
Izgelov D, Davidson E, Barasch D, Regev A, Domb AJ, Hoffman A (2020) Pharmacokinetic investigation of synthetic cannabidiol oral formulations in healthy volunteers. Eur J Pharm Biopharm 154:108–115. https://doi.org/10.1016/j.ejpb.2020.06.021
Jastrząb G, Skrzydlewska, (2019) Cannabidiol regulates the expression of keratinocyte proteins involved in the inflammation process through transcriptional regulation. Cells. https://doi.org/10.3390/cells8080827
Jastrzab A, Jarocka-Karpowicz I, Markowska A, Wronski A, Gegotek A, Skrzydlewska E (2021) Antioxidant and anti-inflammatory effect of cannabidiol contributes to the decreased lipid peroxidation of keratinocytes of rat skin exposed to UV radiation. Oxidative Med Cell Longev. https://doi.org/10.1155/2021/6647222
Jeong S, Jo MJ, Yun HK, Kim DY, Kim BR, Kim JL, Park SH, Na YJ, Jeong YA, Kim BG, Ashktorab H, Smoot DT, Heo JY, Han J, Lee SI, Kim HD, Kim DH, Oh SC, Lee DH (2019) Cannabidiol promotes apoptosis via regulation of XIAP/Smac in gastric cancer. Cell Death Disease. https://doi.org/10.1038/s41419-019-2001-7
Jhawar N, Schoenberg E, Wang JV, Saedi N (2019) The growing trend of cannabidiol in skincare products. Clin Dermatol 37(3):279–281. https://doi.org/10.1016/j.clindermatol.2018.11.002
Jiang RR, Yamaori S, Takeda S, Yamamoto I, Watanabe K (2011) Identification of cytochrome P450 enzymes responsible for metabolism of cannabidiol by human liver microsomes. Life Sci 89(5–6):165–170. https://doi.org/10.1016/j.lfs.2011.05.018
Josiah AJ, Pillai SK, Cordier W, Nell M, Twilley D, Lall N, Ray SS (2021) Cannabidiol-mediated green synthesis, characterization, and cytotoxicity of metal nanoparticles in human keratinocyte cells. ACS Omega 6(43):29078–29090. https://doi.org/10.1021/acsomega.1c04303
Junaid M, Tijani AO, Puri A, Banga AK (2022) In vitro percutaneous absorption studies of cannabidiol using human skin: exploring the effect of drug concentration, chemical enhancers, and essential oils. Int J Pharm. https://doi.org/10.1016/j.ijpharm.2022.121540
Kim B, Cho H-E, Moon SH, Ahn H-J, Bae S, Cho H-D, An S (2020) Transdermal delivery systems in cosmetics. Biomed Dermatol. https://doi.org/10.1186/s41702-020-0058-7
Kitani A, Fuss I, Nakamura K, Kumaki F, Usui T, Strober W (2003) Transforming growth factor (TGF)-β1–producing regulatory T cells induce smad-mediated interleukin 10 secretion that facilitates coordinated immunoregulatory activity and amelioration of TGF-β1–mediated fibrosis. J Exp Med 198(8):1179–1188. https://doi.org/10.1084/jem.20030917
Kobayashi Y, Takeuchi A, Wang Y-G (2006) Synthesis of cannabidiols via alkenylation of cyclohexenyl monoacetate. Org Lett 8(13):2699–2702. https://doi.org/10.1021/ol060692h
Kosgodage US, Matewele P, Awamaria B, Kraev I, Warde P, Mastroianni G, Nunn AV, Guy GW, Bell JD, Inal JM, Lange S (2019) Cannabidiol is a novel modulator of bacterial membrane vesicles. Front Cell Infect Microbiol. https://doi.org/10.3389/fcimb.2019.00324
Koshy ST, Zhang DKY, Grolman JM, Stafford AG, Mooney DJ (2018) Injectable nanocomposite cryogels for versatile protein drug delivery. Acta Biomater 65:36–43. https://doi.org/10.1016/j.actbio.2017.11.024
Kulkarni AA, Thatcher TH, Olsen KC, Maggirwar SB, Phipps RP, Sime PJ (2011) PPAR-γ ligands repress TGFβ-induced myofibroblast differentiation by targeting the PI3K/Akt pathway: implications for therapy of fibrosis. PLoS ONE. https://doi.org/10.1371/journal.pone.0015909
Laprairie RB, Bagher AM, Kelly MEM, Denovan-Wright EM (2015) Cannabidiol is a negative allosteric modulator of the cannabinoid CB1 receptor. Br J Pharmacol 172(20):4790–4805. https://doi.org/10.1111/bph.13250
Latimer, A. Vegamour Launches CBD Products for Hair Growth. [cited 2022 20 de agosto ]; Available from: https://www.cosmeticsandtoiletries.com/formulas-products/hair-care/news/21871226/vegamour-launches-cbd-products-for-hair-growth.
Leas EC, Nobles AL, Caputi TL, Dredze M, Smith DM, Ayers JW (2019) Trends in internet searches for cannabidiol (CBD) in the United States. JAMA Netw Open. https://doi.org/10.1001/jamanetworkopen.2019.13853
Lee CY, Wey SP, Liao MH, Hsu WL, Wu HY, Jan TR (2008) A comparative study on cannabidiol-induced apoptosis in murine thymocytes and EL-4 thymoma cells. Int Immunopharmacol 8(5):732–740. https://doi.org/10.1016/j.intimp.2008.01.018
Lee WS, Erdelyi K, Matyas C, Mukhopadhyay P, Varga ZV, Liaudet L, Hasko G, Cihakova D, Mechoulam R, Pacher P (2016) Cannabidiol limits t cell-mediated chronic autoimmune myocarditis: implications to autoimmune disorders and organ transplantation. Mol Med 22:136–146. https://doi.org/10.2119/molmed.2016.00007
Lessard, P.C. CBD in cosmetics: a practical primer. [cited 2022 26 de agosto ]; Available from: https://www.cosmeticsandtoiletries.com/research/methods-tools/article/21835839/cbd-in-cosmetics-a-practical-primer.
Lewińska A (2021) Optimizing the process design of oil-in-water nanoemulsion for delivering poorly soluble cannabidiol oil. Processes. https://doi.org/10.3390/pr9071180
Liebling JP, Clarkson NJ, Gibbs BW, Yates AS, O’Sullivan SE (2022) An analysis of over-the-counter cannabidiol products in the united kingdom. Cannabis Cannabinoid Res 7(2):207–213. https://doi.org/10.1089/can.2019.0078
Linger P, Mussig J, Fischer H, Kobert J (2002) Industrial hemp (Cannabis sativa L.) growing on heavy metal contaminated soil: fibre quality and phytoremediation potential. Ind Crops Prod. https://doi.org/10.1016/s0926-6690(02)00005-5
Liou GI, Auchampach JA, Hillard CJ, Zhu G, Yousufzai B, Mian S, Khan S, Khalifa Y (2008) Mediation of cannabidiol anti-inflammation in the retina by equilibrative nucleoside transporter and A(2A) adenosine receptor. Invest Ophthalmol vis Sci 49(12):5526–5531. https://doi.org/10.1167/iovs.08-2196
Liu F, Lagares D, Choi KM, Stopfer L, Marinkovic A, Vrbanac V, Probst CK, Hiemer SE, Sisson TH, Horowitz JC, Rosas IO, Fredenburgh LE, Feghali-Bostwick C, Varelas X, Tager AM, Tschumperlin DJ (2015) Mechanosignaling through YAP and TAZ drives fibroblast activation and fibrosis. Am J Physiol-Lung Cell Mol0 Physiol 308(4):L344–L357. https://doi.org/10.1152/ajplung.00300.2014
Liu YK, Qi XY, Wang YS, Li M, Yuan Q, Zhao ZH (2022) Inflammation-targeted cannabidiol-loaded nanomicelles for enhanced oral mucositis treatment. Drug Delivery 29(1):1272–1281. https://doi.org/10.1080/10717544.2022.2027572
Li S, Dong S, Xu W, Tu S, Yan L, Zhao C, Ding J, Chen X (2018) Antibacterial hydrogels. advanced. Science 5(5):1700527. https://doi.org/10.1002/advs.201700527
Li JP, Carvajal R, Bruner L, Kaminski NE (2021) The current understanding of the benefits, safety, and regulation of cannabidiol in consumer products. Food Chem Toxicol. https://doi.org/10.1016/j.fct.2021.112600
Lodzki M, Godin B, Rakou L, Mechoulam R, Gallily R, Touitou E (2003) Cannabidiol-transdermal delivery and anti-inflammatory effect in a murine model. J Control Release 93(3):377–387. https://doi.org/10.1016/j.jconrel.2003.09.001
Loft N, Nguyen TT, Kristensen LE, Thyssen JP, Egeberg A (2022) Disease burden, symptoms, and use of analgesics in patients with psoriasis with or without psoriatic arthritis: a cross-sectional study. J Am Acad Dermatol 86(3):590–597. https://doi.org/10.1016/j.jaad.2021.07.028
Loh CCH, Kim J, Su JC, Daniel BS, Venugopal SS, Rhodes LM, Intong LRA, Law MG, Murrell DF (2014) Development, reliability, and validity of a novel epidermolysis bullosa disease activity and scarring index (EBDASI). J Am Acad Dermatol. https://doi.org/10.1016/j.jaad.2013.09.041
Lucas CJ, Galettis P, Schneider J (2018) The pharmacokinetics and the pharmacodynamics of cannabinoids. Br J Clin Pharmacol 84(11):2477–2482. https://doi.org/10.1111/bcp.13710
Luczaj W, Domingues MD, Domingues P, Skrzydlewska E (2020a) Changes in lipid profile of keratinocytes from rat skin exposed to chronic UVA or UVB radiation and topical application of cannabidiol. Antioxidants. https://doi.org/10.3390/antiox9121178
Luczaj W, Dobrzynska I, Wronski A, Domingues MR, Domingues P, Skrzydlewska E (2020b) Cannabidiol-mediated changes to the phospholipid profile of UVB-irradiated keratinocytes from psoriatic patients. Int J Mol Sci. https://doi.org/10.3390/ijms21186592
Lukhele ST, Motadi LR (2016) Cannabidiol rather than Cannabis sativa extracts inhibit cell growth and induce apoptosis in cervical cancer cells. BMC Complement Altern Med. https://doi.org/10.1186/s12906-016-1280-0
Luo XZ, Reiter MA, d’Espaux L, Wong J, Denby CM, Lechner A, Zhang YF, Grzybowski AT, Harth S, Lin WY, Lee H, Yu CH, Shin J, Deng K, Benites VT, Wang G, Baidoo EEK, Chen Y, Dev I, Petzold CJ, Keasling JD (2019) Complete biosynthesis of cannabinoids and their unnatural analogues in yeast. Nature. https://doi.org/10.1038/s41586-019-0978-9
Maghfour J, Rietcheck H, Szeto MD, Rundle CW, Sivesind TE, Dellavalle RP, Lio P, Dunnick CA, Fernandez J, Yardley H (2021) Tolerability profile of topical cannabidiol and palmitoylethanolamide: a compilation of single-centre randomized evaluator-blinded clinical and in vitro studies in normal skin. Clin Exp Dermatol 46(8):1518–1529. https://doi.org/10.1111/ced.14749
Mahmoudinoodezh H, Telukutla SR, Bhangu SK, Bachari A, Cavalieri F, Mantri N (2022) The transdermal delivery of therapeutic cannabinoids. PHARMACEUTICS. https://doi.org/10.3390/pharmaceutics14020438
Mao KL, Fan ZL, Yuan JD, Chen P, Yang JJ, Xu J, ZhuGe DL, Jin BH, Zhu QY, Shen BX, Sohawon Y, Zhao YZ, Xu HL (2017) Skin-penetrating polymeric nanoparticles incorporated in silk fibroin hydrogel for topical delivery of curcumin to improve its therapeutic effect on psoriasis mouse model. Coll Surf B-Biointerfaces 160:704–714. https://doi.org/10.1016/j.colsurfb.2017.10.029
Martinenghi LD, Jønsson R, Lund T, Jenssen H (2020) Isolation, purification, and antimicrobial characterization of cannabidiolic acid and cannabidiol from cannabis sativa L. Biomolecules 10(6):900. https://doi.org/10.3390/biom10060900
Martin JH, Schneider J, Lucas CJ, Galettis P (2018) Exogenous cannabinoid efficacy: merely a pharmacokinetic interaction? Clin Pharmacokinet 57(5):539–545. https://doi.org/10.1007/s40262-017-0599-0
Marzęda P, Wróblewska-Łuczka P, Drozd M, Florek-Łuszczki M, Załuska-Ogryzek K, Łuszczki JJ (2022) Cannabidiol interacts antagonistically with cisplatin and additively with mitoxantrone in various melanoma cell lines—an isobolographic analysis. Int J Mol Sci 23(12):6752. https://doi.org/10.3390/ijms23126752
Mascarenhas-Melo F, Gonçalves MBS, Peixoto D, Pawar KD, Bell V, Chavda VP, Zafar H, Raza F, Paiva-Santos AC (2022) Application of nanotechnology in management and treatment of diabetic wounds. J Drug Target 30(10):1034–1054. https://doi.org/10.1080/1061186X.2022.2092624
Matarazzo AP, Elisei LMS, Carvalho FC, Bonfilio R, Ruela ALM, Galdino G, Pereira GR (2021) Mucoadhesive nanostructured lipid carriers as a cannabidiol nasal delivery system for the treatment of neuropathic pain. Eur J Pharm Sci. https://doi.org/10.1016/j.ejps.2020.105698
McGregor IS, Cairns EA, Abelev S, Cohen R, Henderson M, Couch D, Arnold JC, Gauld N (2020) Access to cannabidiol without a prescription: a cross-country comparison and analysis. Int J Drug Policy. https://doi.org/10.1016/j.drugpo.2020.102935
McKernan, K., J. Spangler, Y. Helbert, R.C. Lynch, A. Devitt-Lee, L. Zhang, W. Orphe, J. Warner, T. Foss, C.J. Hudalla, M. Silva, and D.R. Smith (2016) Metagenomic analysis of medicinal Cannabis samples; pathogenic bacteria, toxigenic fungi, and beneficial microbes grow in culture-based yeast and mold tests. F1000Research https://doi.org/10.12688/f1000research.9662.1.
Mead A (2017) The legal status of cannabis (marijuana) and cannabidiol (CBD) under US law. Epilepsy Behav 70:288–291. https://doi.org/10.1016/j.yebeh.2016.11.021
Mei XQ, Zhao H, Huang Y, Tang YL, Shi XG, Pu WL, Jiang S, Ma YY, Zhang YT, Bai L, Tu WZ, Zhao YH, Jin L, Wu WY, Wang JC, Liu QM (2020) Involvement of disabled-2 on skin fibrosis in systemic sclerosis. J Dermatol Sci 99(1):44–52. https://doi.org/10.1016/j.jdermsci.2020.05.009
Meyer-Mueller C, Osborn MJ, Tolar J, Boull C, Ebens CL (2022) Revertant mosaicism in epidermolysis bullosa. Biomedicines. https://doi.org/10.3390/biomedicines10010114
Milando R, Friedman A (2019) Cannabinoids: potential role in inflammatory and neoplastic skin diseases. Am J Clin Dermatol 20(2):167–180. https://doi.org/10.1007/s40257-018-0410-5
Millar SA, Stone NL, Bellman ZD, Yates AS, England TJ, O’Sullivan SE (2019) A systematic review of cannabidiol dosing in clinical populations. Br J Clin Pharmacol 85(9):1888–1900. https://doi.org/10.1111/bcp.14038
Miltner N, Beke G, Angyal K, Pinter E, Helyes Z, Biro T, Mihaly J (2018) Assessment of the anti-inflammatory effects of cannabidiol and its fluorinated derivative in in vitro and in vivo models of atopic dermatitis. J Investig Dermatol 138(5):S173–S173. https://doi.org/10.1016/j.jid.2018.03.1032
Mogi C, Yoshida M, Kawano K, Fukuyama T, Arai T (2022) Effects of cannabidiol without delta-9-tetrahydrocannabinol on canine atopic dermatitis: a retrospective assessment of 8 cases. Can Vet J 63(4):423–426
Momekova D, Ivanov E, Konstantinov S, Ublekov F, Petrov PD (2020) Nanocomposite cryogel carriers from 2-hydroxyethyl cellulose network and cannabidiol-loaded polymeric micelles for sustained topical delivery. Polymers. https://doi.org/10.3390/polym12051172
Momekova D, Danov Y, Momekov G, Ivanov E, Petrov P (2021) Polysaccharide cryogels containing β-cyclodextrin for the delivery of cannabidiol. Pharmaceutics 13(11):1774. https://doi.org/10.3390/pharmaceutics13111774
Mugnaini C, Rabbito A, Brizzi A, Palombi N, Petrosino S, Verde R, Di Marzo V, Ligresti A, Corelli F (2019) Synthesis of novel 2-(1-adamantanylcarboxamido)thiophene derivatives. selective cannabinoid type 2 (CB2) receptor agonists as potential agents for the treatment of skin inflammatory disease. Eur J Med Chem 161:239–251. https://doi.org/10.1016/j.ejmech.2018.09.070
Muscara C, Smeriglio A, Trombetta D, Mandalari G, La Camera E, Grassi G, Circosta C (2021) Phytochemical characterization and biological properties of two standardized extracts from a non-psychotropic Cannabis sativa L. cannabidiol (CBD)-chemotype. Phytother Res 35(9):5269–5281. https://doi.org/10.1002/ptr.7201
Nabissi M, Morelli MB, Amantini C, Liberati S, Santoni M, Ricci-Vitiani L, Pallini R, Santoni G (2015) Cannabidiol stimulates Aml-1a-dependent glial differentiation and inhibits glioma stem-like cells proliferation by inducing autophagy in a TRPV2-dependent manner. Int J Cancer 137(8):1855–1869. https://doi.org/10.1002/ijc.29573
Namazi H, Heydari A (2014) Synthesis of beta-cyclodextrin-based dendrimer as a novel encapsulation agent. Polym Int 63(8):1447–1455. https://doi.org/10.1002/pi.4637
Niu XQ, Zhang DP, Bian Q, Feng XF, Li H, Rao YF, Shen YM, Geng FN, Yuan AR, Ying XY, Gao JQ (2019) Mechanism investigation of ethosomes transdermal permeation. Int J Pharm-X. https://doi.org/10.1016/j.ijpx.2019.100027
Odegaard JI, Ricardo-Gonzalez RR, Goforth MH, Morel CR, Subramanian V, Mukundan L, Eagle AR, Vats D, Brombacher F, Ferrante AW, Chawla A (2007) Macrophage-specific PPARγ controls alternative activation and improves insulin resistance. Nature 447(7148):1116–1120. https://doi.org/10.1038/nature05894
Olah A, Toth BI, Borbiro I, Sugawara K, Szollosi AG, Czifra G, Pal B, Ambrus L, Kloepper J, Camera E, Ludovici M, Picardo M, Voets T, Zouboulis CC, Paus R, Biro T (2014) Cannabidiol exerts sebostatic and antiinflammatory effects on human sebocytes. J Clin Investig 124(9):3713–3724. https://doi.org/10.1172/jci64628
Olivas-Aguirre M, Torres-López L, Valle-Reyes JS, Hernández-Cruz A, Pottosin I, Dobrovinskaya O (2019) Cannabidiol directly targets mitochondria and disturbs calcium homeostasis in acute lymphoblastic leukemia. Cell Death Disease. https://doi.org/10.1038/s41419-019-2024-0
Ordonnance du DFI sur les tableaux des stupéfiants, des substances psychotropes, des précurseurs et des adjuvants chimiques. 2011 8/8/2022]; Available from: https://www.fedlex.admin.ch/eli/oc/2011/363/fr.
Pacelli S, Di Muzio L, Paolicelli P, Fortunati V, Petralito S, Trilli J, Casadei MA (2021) Dextran-polyethylene glycol cryogels as spongy scaffolds for drug delivery. Int J Biol Macromol 166:1292–1300. https://doi.org/10.1016/j.ijbiomac.2020.10.273
Park C, Zuo J, Somayaji V, Lee BJ, Lobenberg R (2021) Development of a novel cannabinoid-loaded microemulsion towards an improved stability and transdermal delivery. Int J Pharm. https://doi.org/10.1016/j.ijpharm.2021.120766
Pattnaik F, Nanda S, Mohanty S, Dalai AK, Kumar V, Ponnusamy SK, Naik S (2022) Cannabis: chemistry, extraction and therapeutic applications. Chemosphere. https://doi.org/10.1016/j.chemosphere.2021.133012
Paudel KS, Hammell DC, Agu RU, Valiveti S, Stinchcomb AL (2010) Cannabidiol bioavailability after nasal and transdermal application: effect of permeation enhancers. Drug Dev Ind Pharm 36(9):1088–1097. https://doi.org/10.3109/03639041003657295
Pereira I, Monteiro C, Pereira-Silva M, Peixoto D, Nunes C, Reis S, Veiga F, Hamblin MR, Paiva-Santos AC (2023) Nanodelivery systems for cutaneous melanoma treatment. Eur J Pharm Biopharm 184:214–247. https://doi.org/10.1016/j.ejpb.2023.02.002
Pires PC, Mascarenhas-Melo F, Pedrosa K, Lopes D, Lopes J, Macário-Soares A, Peixoto D, Giram PS, Veiga F, Paiva-Santos AC (2023) Polymer-based biomaterials for pharmaceutical and biomedical applications: a focus on topical drug administration. Eur Poly J. https://doi.org/10.1016/j.eurpolymj.2023.111868
Pirrung MC (2020) Synthetic access to cannabidiol and analogs as active pharmaceutical ingredients. J Med Chem 63(21):12131–12136. https://doi.org/10.1021/acs.jmedchem.0c00095
Qu J, Zhao X, Liang YP, Zhang TL, Ma PX, Guo BL (2018) Antibacterial adhesive injectable hydrogels with rapid self-healing, extensibility and compressibility as wound dressing for joints skin wound healing. Biomaterials 183:185–199. https://doi.org/10.1016/j.biomaterials.2018.08.044
Radwan-Pragłowska J, Janus Ł, Piątkowski M, Sierakowska A, Szajna E, Matýsek D, Bogdał D (2021) Development of stimuli-responsive chitosan/ZnO nps transdermal systems for controlled cannabidiol delivery. Polymers 13(2):211. https://doi.org/10.3390/polym13020211
Rajesh M, Mukhopadhyay P, Batkai S, Patel V, Saito K, Matsumoto S, Kashiwaya Y, Horvath B, Mukhopadhyay B, Becker L, Hasko G, Liaudet L, Wink DA, Veves A, Mechoulam R, Pacher P (2010) Cannabidiol attenuates cardiac dysfunction, oxidative stress, fibrosis, and inflammatory and cell death signaling pathways in diabetic cardiomyopathy. J Am Coll Cardiol 56(25):2115–2125. https://doi.org/10.1016/j.jacc.2010.07.033
EUR-LEX. Regulamento (UE) 2022/1393 da Comissão de 11 de agosto de 2022 que altera o Regulamento (CE) n.o 1881/2006 no que diz respeito aos teores máximos de delta-9-tetra-hidrocanabinol (Δ9-THC) nas sementes de cânhamo e seus produtos derivados. [cited 2022 3 de setembro ]; Available from: https://eur-lex.europa.eu/legal-content/PT/TXT/?uri=uriserv%3AOJ.L_.2022.211.01.0083.01.POR&toc=OJ%3AL%3A2022%3A211%3ATOC.
Ruhl T, Lippold EF, Christer T, Schaefer B, Kim BS, Beier JP (2021) Genetic deletion of the cannabinoid receptors CB1 and CB2 enhances inflammation with diverging effects on skin wound healing in mice. Life Sci. https://doi.org/10.1016/j.lfs.2021.120018
Rundle CW, Rietcheck H, Maghfour J, Dercon S, Fernandez J, Lio P, Dellavalle RP, Fujita M, Yardley H (2021) Anti-inflammatory effect of cannabidiol and palmitoylethanolamide containing topical formulation on skin in a 12-O-tetradecanoylphorbol-13-acetate-induced dermatitis model in mice. Dermatitis 33(4):277–281. https://doi.org/10.1097/DER.0000000000000722
Russo EB (2007) History of cannabis and its preparations in saga, science, and sobriquet. Chem Biodivers 4(8):1614–1648. https://doi.org/10.1002/cbdv.200790144
Russo C, Lavorgna M, Nugnes R, Orlo E, Isidori M (2021) Comparative assessment of antimicrobial, antiradical and cytotoxic activities of cannabidiol and its propyl analogue cannabidivarin. Sci Reports. https://doi.org/10.1038/s41598-021-01975-z
Salau O, Bagde A, Kalvala A, Singh M (2022) Enhancement of transdermal permeation of cannabinoids and their pharmacodynamic evaluation in rats. Int J Pharm 624:122016. https://doi.org/10.1016/j.ijpharm.2022.122016
Sangiovanni E, Fumagalli M, Pacchetti B, Piazza S, Magnavacca A, Khalilpour S, Melzi G, Martinelli G, Dell’Agli M (2019) Cannabis sativa L extract and cannabidiol inhibit in vitro mediators of skin inflammation and wound injury. Phytother Res 33(8):2083–2093. https://doi.org/10.1002/ptr.6400
Scheffer IE, Hulihan J, Messenheimer J, Ali S, Keenan N, Griesser J, Gutterman DL, Sebree T, Sadleir LG (2021) Safety and tolerability of transdermal cannabidiol gel in children with developmental and epileptic encephalopathies a nonrandomized controlled trial. JAMA Netw Open. https://doi.org/10.1001/jamanetworkopen.2021.23930
Schlabach, J. Botanika life CBD skin care launches. [cited 2022 24 de agosto]; Available from: https://www.cosmeticsandtoiletries.com/formulas-products/skin-care/news/21862348/botanika-life-cbd-skin-care-launches.
Schrader NHB, Duipmans JC, Molenbuur B, Wolff AP, Jonkman MF (2019) Combined tetrahydrocannabinol and cannabidiol to treat pain in epidermolysis bullosa: a report of three cases. Br J Dermatol 180(4):922–924. https://doi.org/10.1111/bjd.17341
Schräder NHB, Gorell ES, Stewart RE, Duipmans JC, Harris N, Perez VA, Tang JY, Wolff AP, Bolling MC (2021) Cannabinoid use and effects in patients with epidermolysis bullosa: an international cross-sectional survey study. Orphanet J Rare Diseases. https://doi.org/10.1186/s13023-021-02010-0
Scianna, T. Sexy Hair Adds to CBD-based Calm Collection. [cited 2022 20 de agosto ]; Available from: https://www.cosmeticsandtoiletries.com/formulas-products/hair-care/news/21863088/sexy-hair-concepts-sexy-hair-adds-to-cbd-based-calm-collection.
Serruya R, Maor Y (2021) Hair growth-promotion effects at the cellular level and antioxidant activity of the plant-based extract Phyllotex (TM). Heliyon. https://doi.org/10.1016/j.heliyon.2021.e07888
Sharkawy A, Silva AM, Rodrigues F, Barreiro F, Rodrigues A (2021) Pickering emulsions stabilized with chitosan/collagen peptides nanoparticles as green topical delivery vehicles for cannabidiol (CBD). Coll Surf-Physicochem Eng Aspects. https://doi.org/10.1016/j.colsurfa.2021.127677
Sharkawy A, Barreiro F, Rodrigues A (2022) Pickering emulsions stabilized with chitosan/gum Arabic particles: effect of chitosan degree of deacetylation on the physicochemical properties and cannabidiol (CBD) topical delivery. J Mol Liquids 355:118993. https://doi.org/10.1016/j.molliq.2022.118993
Shi VY, Leo M, Hassoun L, Chahal DS, Maibach HI, Sivamani RK (2015) Role of sebaceous glands in inflammatory dermatoses. J Am Acad Dermatol 73(5):856–863. https://doi.org/10.1016/j.jaad.2015.08.015
Shultz ZP, Lawrence GA, Jacobson JM, Cruz EJ, Leahy JW (2018) Enantioselective total synthesis of cannabinoids—a route for analogue development. Org Lett 20(2):381–384. https://doi.org/10.1021/acs.orglett.7b03668
Smith G, Satino J (2021) Hair regrowth with cannabidiol (CBD)-rich hemp extract. Cannabis. https://doi.org/10.26828/cannabis/2021.01.003
Sosnik A, Shabo RB, Halamish HM (2021) Cannabidiol-loaded mixed polymeric micelles of chitosan/poly(vinyl alcohol) and poly(methyl methacrylate) for trans-corneal delivery. Pharmaceutics. https://doi.org/10.3390/pharmaceutics13122142
Steinhoff M, Bienenstock J, Schmelz M, Maurer M, Wei E, Bíró T (2006) Neurophysiological, neuroimmunological, and neuroendocrine basis of pruritus. J Investig Dermatol 126(8):1705–1718. https://doi.org/10.1038/sj.jid.5700231
Szabó IL, Herczeg-Lisztes E, Szollosi AG, Szegedi A, Bíró T, Oláh A (2017) 263 (-)-cannabidiol differentially influences hair growth. J Investig Dermatol 137(10):S238. https://doi.org/10.1016/j.jid.2017.07.261
Szabó IL, Herczeg-Lisztes E, Szegedi A, Nemes B, Paus R, Bíró T, Szöllősi AG (2019) TRPV4 Is expressed in human hair follicles and inhibits hair growth in vitro. J Investig Dermatol 139(6):1385–1388. https://doi.org/10.1016/j.jid.2018.11.020
Szabo IL, E Lisztes, G Beke, KF Toth, R Paus, A Olah, and T Biro (2020) The Phytocannabinoid (-)-Cannabidiol Operates as a Complex, Differential Modulator of Human Hair Growth: Anti-Inflammatory Submicromolar versus Hair Growth Inhibitory Micromolar Effects. Journal of Investigative Dermatology DOI: https://doi.org/10.1016/j.jid.2019.07.690.
Tager AM, LaCamera P, Shea BS, Campanella GS, Selman M, Zhao Z, Polosukhin V, Wain J, Karimi-Shah BA, Kim ND, Hart WK, Pardo A, Blackwell TS, Xu Y, Chun J, Luster AD (2008) The lysophosphatidic acid receptor LPA(1) links pulmonary fibrosis to lung injury by mediating fibroblast recruitment and vascular leak. Nat Med 14(1):45–54. https://doi.org/10.1038/nm1685
Tampucci S, Paganini V, Burgalassi S, Chetoni P, Monti D (2022) Nanostructured drug delivery systems for targeting 5-α-reductase inhibitors to the hair follicle. Pharmaceutics 14(2):286. https://doi.org/10.3390/pharmaceutics14020286
Taylor L, Gidal B, Blakey G, Tayo B, Morrison G (2018) A phase I, randomized, double-blind, placebo-controlled, single ascending dose, multiple dose, and food effect trial of the safety, tolerability and pharmacokinetics of highly purified cannabidiol in healthy subjects. CNS Drugs 32(11):1053–1067. https://doi.org/10.1007/s40263-018-0578-5
Telek A, Bíró T, Bodó E, Tóth BI, Borbíró I, Kunos G, Paus R (2007) Inhibition of human hair follicle growth by endo-and exocannabinoids. FASEB J 21(13):3534–3541. https://doi.org/10.1096/fj.06-7689com
Tham M, Yilmaz O, Alaverdashvili M, Kelly MEM, Denovan-Wright EM, Laprairie RB (2019) Allosteric and orthosteric pharmacology of cannabidiol and cannabidiol-dimethylheptyl at the type 1 and type 2 cannabinoid receptors. Br J Pharmacol 176(10):1455–1469. https://doi.org/10.1111/bph.14440
Thyssen JP, Johansen JD, Zachariae C, Menne T, Linneberg A (2013) Xerosis is associated with atopic dermatitis, hand eczema and contact sensitization independent of filaggrin gene mutations. Acta Derm Venereol 93(4):406–410. https://doi.org/10.2340/00015555-1539
Turck D, Bohn T, Castenmiller J, De Henauw S, Hirsch-Ernst KI, Maciuk A, Mangelsdorf I, McArdle HJ, Naska A, Pelaez C, Pentieva K, Siani A, Thies F, Tsabouri S, Vinceti M, Cubadda F, Frenzel T, Heinonen M, Marchelli R, Neuhäuser-Berthold M, Poulsen M, Prieto Maradona M, Schlatter JR, Trezza V, Van Loveren H, Albert O, Dumas C, Germini A, Gelbmann W, Kass G, Kouloura E, Noriega Fernandez E, Rossi A, Knutsen HK (2022) Statement on safety of cannabidiol as a novel food: data gaps and uncertainties. EFSA J. https://doi.org/10.2903/j.efsa.2022.7322
Vaccani A, Massi P, Colombo A, Rubino T, Parolaro D (2005) Cannabidiol inhibits human glioma cell migration through a cannabinoid receptor-independent mechanism. Br J Pharmacol 144(8):1032–1036. https://doi.org/10.1038/sj.bjp.0706134
Vanti G, Grifoni L, Bergonzi MC, Antiga E, Montefusco F, Caproni M, Bilia AR (2021) Development and optimisation of biopharmaceutical properties of a new microemulgel of cannabidiol for locally-acting dermatological delivery. Int J Pharm. https://doi.org/10.1016/j.ijpharm.2021.121036
Vincenzi C, Tosti A (2020) Efficacy and tolerability of a shampoo containing broad-spectrum cannabidiol in the treatment of scalp inflammation in patients with mild to moderate scalp psoriasis or seborrheic dermatitis. Skin Appendage Disorders 6(6):355–361. https://doi.org/10.1159/000510896
Vuolo F, Abreu SC, Michels M, Xisto DG, Blanco NG, Hallak JEC, Zuardi AW, Crippa JA, Reis C, Bahl M, Pizzichinni E, Maurici R, Pizzichinni MMM, Rocco PRM, Dal-Pizzol F (2019) Cannabidiol reduces airway inflammation and fibrosis in experimental allergic asthma. Eur J Pharmacol 843:251–259. https://doi.org/10.1016/j.ejphar.2018.11.029
Walsh KB, McKinney AE, Holmes AE (2021) Minor cannabinoids: biosynthesis, molecular pharmacology and potential therapeutic uses. Front Pharmacol 12:777804. https://doi.org/10.3389/fphar.2021.777804
Wang M, Wang Y-H, Avula B, Radwan MM, Wanas AS, Van Antwerp J, Parcher JF, Elsohly MA, Khan IA (2016) Decarboxylation study of acidic cannabinoids: a novel approach using ultra-high-performance supercritical fluid chromatography/photodiode array-mass spectrometry. Cannabis Cannabinoid Res 1(1):262–271. https://doi.org/10.1089/can.2016.0020
Wang X-H, Su T, Zhao J, Wu Z, Wang D, Zhang W-N, Wu Q-X, Chen Y (2020) Fabrication of polysaccharides-based hydrogel films for transdermal sustained delivery of Ibuprofen. Cellulose 27(17):10277–10292. https://doi.org/10.1007/s10570-020-03503-0
Wang C, Wang J, Sun YH, Freeman K, McHenry MA, Wang CN, Guo MR (2022) Enhanced stability and oral bioavailability of cannabidiol in zein and whey protein composite nanoparticles by a modified anti-solvent approach. Foods. https://doi.org/10.3390/foods11030376
Wassmann CS, Hojrup P, Klitgaard JK (2020) Cannabidiol is an effective helper compound in combination with bacitracin to kill Gram-positive bacteria. Sci Reports. https://doi.org/10.1038/s41598-020-60952-0
Wernig G, Chen SY, Cui L, Van Neste C, Tsai JM, Kambham N, Vogel H, Natkunam Y, Gilliland DG, Nolan G, Weissman IL (2017a) Unifying mechanism for different fibrotic diseases. Proc Natl Acad Sci USA 114(18):4757–4762. https://doi.org/10.1073/pnas.1621375114
Wernig G, Chen S-Y, Cui L, Van Neste C, Tsai JM, Kambham N, Vogel H, Natkunam Y, Gilliland DG, Nolan G, Weissman IL (2017b) Unifying mechanism for different fibrotic diseases. Proc Natl Acad Sci 114(18):4757–4762. https://doi.org/10.1073/pnas.1621375114
Wilkinson HN, Hardman MJ (2020) Wound healing: cellular mechanisms and pathological outcomes. Open Biol. https://doi.org/10.1098/rsob.200223
Wilkinson JD, Williamson EM (2007) Cannabinoids inhibit human keratinocyte proliferation through a non-CB1/CB2 mechanism and have a potential therapeutic value in the treatment of psoriasis. J Dermatol Sci 45(2):87–92. https://doi.org/10.1016/j.jdermsci.2006.10.009
Wojcik P, Garley M, Wronski A, Jablonska E, Skrzydlewska E (2020) Cannabidiol modifies the formation of NETs in neutrophils of psoriatic patients. Int J Mol Sci. https://doi.org/10.3390/ijms21186795
Wynn TA, Ramalingam TR (2012) Mechanisms of fibrosis: therapeutic translation for fibrotic disease. Nat Med 18(7):1028–1040. https://doi.org/10.1038/nm.2807
Xu HM, Wen Y, Chen SY, Zhu L, Feng RL, Song ZM (2020) Paclitaxel skin delivery by micelles-embedded Carbopol 940 hydrogel for local therapy of melanoma. Int J Pharm. https://doi.org/10.1016/j.ijpharm.2020.119626
Yeroushalmi S, Nelson K, Sparks A, Friedman A (2020) Perceptions and recommendation behaviors of dermatologists for medical cannabis: a pilot survey. Complement Therapies Med. https://doi.org/10.1016/j.ctim.2020.102552
Young CN, Koepke JI, Terlecky LJ, Borkin MS, Boyd SL, Terlecky SR (2008) Reactive oxygen species in tumor necrosis factor-alpha-activated primary human keratinocytes: implications for psoriasis and inflammatory skin disease. J Investig Dermatol 128(11):2606–2614. https://doi.org/10.1038/jid.2008.122
Yun HK, Jeong S, Jeong YA, Jo MJ, Kim JH, Park SH, Kim BR, Na YJ, Kim DY, Kim BG, Lee DH, Oh SC (2019) Cannabidiol-induced apoptosis is mediated by activation of Noxa in human colorectal cancer cells. Can Res. https://doi.org/10.1158/1538-7445.am2019-714
Zakany N, Olah A, Markovics A, Takacs E, Aranyasz A, Nicolussi S, Piscitelli F, Allara M, Por A, Kovacs I, Zouboulis CC, Gertsch J, Di Marzo V, Biro T, Szabo T (2018) Endocannabinoid tone regulates human sebocyte biology. J Investig Dermatol 138(8):1699–1706. https://doi.org/10.1016/j.jid.2018.02.022
Zamansky M, Zehavi N, Ben-Shabat S, Sintov AC (2021) Characterization of nanoparticles made of ethyl cellulose and stabilizing lipids: mode of manufacturing, size modulation, and study of their effect on keratinocytes. Int J Pharm. https://doi.org/10.1016/j.ijpharm.2021.121003
Zeng D, Chen C, Zhou W, Ma XS, Pu X, Zeng Y, Zhou WK, Lv FL (2021) TRPA1 deficiency alleviates inflammation of atopic dermatitis by reducing macrophage infiltration. Life Sci. https://doi.org/10.1016/j.lfs.2020.118906
Zheng Z, Qi JC, Hu LQ, Ouyang DF, Wang HZ, Sun QL, Lin LJ, You LD, Tang B (2022) A cannabidiol-containing alginate based hydrogel as novel multifunctional wound dressing for promoting wound healing. Biomater Adv. https://doi.org/10.1016/j.msec.2021.112560
Funding
Open access funding provided by FCT|FCCN (b-on).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ferreira, B.P., Costa, G., Mascarenhas-Melo, F. et al. Skin applications of cannabidiol: sources, effects, delivery systems, marketed formulations and safety. Phytochem Rev 22, 781–828 (2023). https://doi.org/10.1007/s11101-023-09860-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11101-023-09860-5