Abstract
Background
It is estimated that one-third of delirium cases in hospitals could be prevented with appropriate interventions. In Dutch hospitals a manual instrument (VMS-questions) is used to identify patients at-risk for delirium. Delirium Model (DEMO) is an automated model which could support delirium prevention more efficiently. However, it has not been validated beyond the hospital it was developed in.
Aim
To externally validate the DEMO and compare its performance to the VMS-questions.
Method
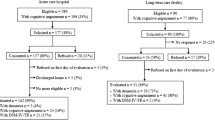
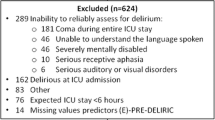
A retrospective cohort study between July and December 2018 was conducted. Delirium cases were identified through a chart review, and the VMS-questions were extracted from the electronic health records. The DEMO was validated in patients ≥ 60 years, and a comparison with the VMS-questions was made in patients ≥ 70 years.
Results
In total 1,345 admissions were included. The DEMO predicted 59 out of 75 delirium cases (sensitivity 0.79, 95% CI = 0.68–0.87; specificity 0.75, 95% CI = 0.72–0.77). Compared to the VMS-questions, the DEMO showed a lower specificity (0.64 vs. 0.72; p < 0.001) and a comparable sensitivity (0.83 vs. 0.80; p = 0.56). The VMS-questions were missing in 20% of admissions, in which the DEMO correctly predicted 10 of 12 delirium cases.
Conclusion
The DEMO showed acceptable performance for delirium prediction. Overall the DEMO predicted more delirium cases because the VMS-questions were missing in 20% of admissions. This study shows that automated instruments such as DEMO could play a key role in the efficient and timely deployment of measures to prevent delirium.

Similar content being viewed by others
References
Davoudi A, Ebadi A, Rashidi P, et al. Delirium prediction using machine learning models on preoperative electronic health records data. Proc IEEE Int Symp Bioinformatics Bioeng. 2017;2017:568–73. https://doi.org/10.1109/BIBE.2017.00014.
Siddiqi N, House AO, Holmes JD. Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing. 2006;35(4):350–64. https://doi.org/10.1093/ageing/afl005.
Hapca S, Guthrie B, Cvoro V, et al. Mortality in people with dementia, delirium, and unspecified cognitive impairment in the general hospital: prospective cohort study of 6,724 patients with 2 years follow-up. Clin Epidemiol. 2018;10:1743–53. https://doi.org/10.2147/CLEP.S174807.
Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911–22. https://doi.org/10.1016/S0140-6736(13)60688-1.
Salluh JI, Wang H, Schneider EB, et al. Outcome of delirium in critically ill patients: systematic review and meta-analysis. BMJ. 2015;350:h2538. https://doi.org/10.1136/bmj.h2538.
Marcantonio ER. Delirium in hospitalized older adults. N Engl J Med. 2017;377(15):1456–66. https://doi.org/10.1056/NEJMcp1605501.
Carrasco MP, Villarroel L, Andrade M, et al. Development and validation of a delirium predictive score in older people. Age Ageing. 2014;43(3):346–51. https://doi.org/10.1093/ageing/aft141.
Strijbos MJ, Steunenberg B, van der Mast RC, et al. Design and methods of the Hospital Elder Life Program (HELP), a multicomponent targeted intervention to prevent delirium in hospitalized older patients: efficacy and cost-effectiveness in Dutch health care. BMC Geriatr. 2013;13:78. https://doi.org/10.1186/1471-2318-13-78.
Setters B, Solberg LM. Delirium. Prim Care. 2017;44(3):541–59. https://doi.org/10.1016/j.pop.2017.04.010.
Lindroth H, Bratzke L, Purvis S, et al. Systematic review of prediction models for delirium in the older adult inpatient. BMJ Open. 2018;8(4):e019223. https://doi.org/10.1136/bmjopen-2017-019223.
Chen Y, Du H, Wei BH, et al. Development and validation of risk-stratification delirium prediction model for critically ill patients: A prospective, observational, single-center study. Medicine (Baltimore). 2017;96(29):e7543. https://doi.org/10.1097/MD.0000000000007543.
de Wit HA, Winkens B, Mestres Gonzalvo C, et al. The development of an automated ward independent delirium risk prediction model. Int J Clin Pharm. 2016;38(4):915–23. https://doi.org/10.1007/s11096-016-0312-7.
Douglas VC, Hessler CS, Dhaliwal G, et al. The AWOL tool: derivation and validation of a delirium prediction rule. J Hosp Med. 2013;8(9):493–9. https://doi.org/10.1002/jhm.2062.
Kukreja D, Gunther U, Popp J. Delirium in the elderly: current problems with increasing geriatric age. Indian J Med Res. 2015;142(6):655–62. https://doi.org/10.4103/0971-5916.174546.
Oh ES, Fong TG, Hshieh TT, et al. Delirium in older persons: advances in diagnosis and treatment. JAMA. 2017;318(12):1161–74. https://doi.org/10.1001/jama.2017.12067.
Yang Y, Zhao X, Dong T, et al. Risk factors for postoperative delirium following hip fracture repair in elderly patients: a systematic review and meta-analysis. Aging Clin Exp Res. 2017;29(2):115–26. https://doi.org/10.1007/s40520-016-0541-6.
Kinchin I, Mitchell E, Agar M, et al. The economic cost of delirium: a systematic review and quality assessment. Alzheimers Dement. 2021;17(6):1026–41. https://doi.org/10.1002/alz.12262.
Nederlandse Vereniging voor Klinische Geriatrie. Delier bij volwassenen en ouderen. 2020. https://richtlijnendatabase.nl/richtlijn/delier_bij_volwassenen_en_ouderen/startpagina_-_delier_bij_volwassenen_en_ouderen.html. Accessed 24 July 2023.
Inouye SK, Bogardus ST, Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340(9):669–76. https://doi.org/10.1056/nejm199903043400901.
Expertgroep Kwetsbare ouderen. VMS Veiligheidsprogramma: Kwetsbare ouderen. Den Haag. 2009. https://www.vmszorg.nl/wp-content/uploads/2017/11/web_2009.0104_praktijkgids_kwetsbare_ouderen.pdf. Accessed 24 July 2023.
VMSzorg. Dutch patient safety programme. 2021. https://www.vmszorg.nl/vms-veiligheidsprogramma/dutch-patient-safety-programme-english/. Accessed 26 July 2023.
Ettema R, Heim N, Hamaker M, et al. Validity of a screening method for delirium risk in older patients admitted to a general hospital in the Netherlands. Gen Hosp Psychiatry. 2018;55:44–50. https://doi.org/10.1016/j.genhosppsych.2018.09.004.
Mestres Gonzalvo C, de Wit H, van Oijen BPC, et al. Validation of an automated delirium prediction model (DElirium MOdel (DEMO)): an observational study. BMJ Open. 2017;7(11):e016654. https://doi.org/10.1136/bmjopen-2017-016654.
Inouye SK, Leo-Summers L, Zhang Y, et al. A chart-based method for identification of delirium: validation compared with interviewer ratings using the confusion assessment method. J Am Geriatr Soc. 2005;53(2):312–8. https://doi.org/10.1111/j.1532-5415.2005.53120.x.
Wassenaar A, Schoonhoven L, Devlin JW, et al. Delirium prediction in the intensive care unit: comparison of two delirium prediction models. Crit Care. 2018;22(1):114. https://doi.org/10.1186/s13054-018-2037-6.
Schulthess-Lisibach AE, Gallucci G, Benelli V, et al. Predicting delirium in older non-intensive care unit inpatients: development and validation of the DELIrium risK Tool (DELIKT). Int J Clin Pharm. 2023. https://doi.org/10.1007/s11096-023-01566-0.
Collins N, Blanchard MR, Tookman A, et al. Detection of delirium in the acute hospital. Age Ageing. 2010;39(1):131–5. https://doi.org/10.1093/ageing/afp201.
Inouye SK. Predisposing and precipitating factors for delirium in hospitalized older patients. Dement Geriatr Cogn Disord. 1999;10(5):393–400. https://doi.org/10.1159/000017177.
Young J, Leentjens AF, George J, et al. Systematic approaches to the prevention and management of patients with delirium. J Psychosom Res. 2008;65(3):267–72. https://doi.org/10.1016/j.jpsychores.2008.05.022.
Young J, Murthy L, Westby M, et al. Diagnosis, prevention, and management of delirium: summary of NICE guidance. BMJ. 2010;341:c3704. https://doi.org/10.1136/bmj.c3704.
Funding
No specific funding was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ali, M.I.M., Kalkman, G.A., Wijers, C.H.W. et al. External validity of an automated delirium prediction model (DEMO) and comparison to the manual VMS-questions: a retrospective cohort study. Int J Clin Pharm 45, 1128–1135 (2023). https://doi.org/10.1007/s11096-023-01641-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-023-01641-6