Abstract
Background
Although duloxetine has shown a positive effect on pain relief with hip and knee osteoarthritis, there is no pooled analysis of duloxetine for pain relief and opioid consumption in patients after total hip or knee arthroplasty.
Aim
This systematic review and meta-analysis aimed to analyze pain control, opioid consumption, and associated adverse events of perioperative administration of duloxetine after total hip or knee arthroplasty.
Method
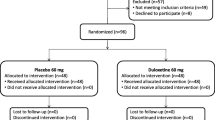
After being registered with PROSPERO (CRD42022323202), the databases of MEDLINE, PubMed, Embase, Web of Science, Cochrane Library, and ClinicalTrials.gov were searched from inception until March 20, 2023, for randomized controlled trials (RCTs). Primary outcomes were the visual Analog Scale (VAS) pain scores at rest (rVAS) and upon ambulation (aVAS). Secondary outcomes were postoperative opioid consumption quantified as oral morphine milligram equivalents (MMEs) and adverse effects of duloxetine.
Results
Nine RCTs with 806 cases were included. Duloxetine was associated with lower VAS scores at different times after surgery (24 h, two weeks, and ≥ 3 months). Compared to placebo, perioperative daily duloxetine use significantly reduced daily opioid MMEs at 24 h (standard mean deviation [SMD] −0.71, 95% confidence interval [95% CI] −1.19 to −0.24, P = 0.003), three days (SMD −1.10, 95% CI −1.70 to −0.50, P = 0.0003), and one week (SMD −1.18, 95% CI −1.99 to −0.38, P = 0.004) after surgery. The duloxetine group had a significantly lower rate of nausea (odds ratio 0.62, 95% CI [0.41 to 0.94], P = 0.02) and a higher rate of drowsiness and somnolence (odds ratio 1.87, 95% CI [1.13 to 3.07], P = 0.01) compared to the placebo group. No significant differences were observed in the rates of other adverse events.
Conclusion
Perioperative duloxetine significantly decreased postoperative pain and opioid consumption with good safety profiles. Further high quality designed and well-controlled randomized trials are warranted.





Similar content being viewed by others
References
Bashinskaya B, Zimmerman RM, Walcott BP, et al. Arthroplasty utilization in the United States is predicted by age-specific population groups. ISRN Orthop. 2012;2012:185938.
Ackerman IN, Bohensky MA, Zomer E, et al. The projected burden of primary total knee and hip replacement for osteoarthritis in Australia to the year 2030. BMC Musculoskelet Disord. 2019;20(1):90.
Karam JA, Schwenk ES, Parvizi J. An update on multimodal pain management after total joint arthroplasty. J Bone Joint Surg Am. 2021;103(17):1652–62.
Beswick AD, Wylde V, Gooberman-Hill R, et al. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open. 2012;2(1):e000435.
Joshi GP, Ogunnaike BO. Consequences of inadequate postoperative pain relief and chronic persistent postoperative pain. Anesthesiol Clin North Am. 2005;23(1):21–36.
Lunn MP, Hughes RA, Wiffen PJ. Duloxetine for treating painful neuropathy, chronic pain or fibromyalgia. Cochrane Database Syst Rev. 2014;2014(1):Cd007115.
Ammitzbøll N, Arendt-Nielsen L, Bertoli D, et al. A mechanism-based proof of concept study on the effects of duloxetine in patients with painful knee osteoarthritis. Trials. 2021;22(1):958.
Braillon A. Efficacy and safety of duloxetine in osteoarthritis or chronic low back pain? The tip of an iceberg! Osteoarthritis Cartilage. 2020;28(9):1298–9.
Brown JP, Boulay LJ. Clinical experience with duloxetine in the management of chronic musculoskeletal pain. A focus on osteoarthritis of the knee. Ther Adv Musculoskelet Dis. 2013;5(6):291–304.
Branton MW, Hopkins TJ, Nemec EC. Duloxetine for the reduction of opioid use in elective orthopedic surgery: a systematic review and meta-analysis. Int J Clin Pharm. 2021;43(2):394–403.
Yuan M, Tang T, Ding Z, et al. Analgesic effect of perioperative duloxetine in patients after total knee arthroplasty: a prospective, randomized, double-blind, placebo-controlled trial. BMC Musculoskelet Disord. 2022;23(1):242.
YaDeau JT, Mayman DJ, Jules-Elysee KM, et al. Effect of duloxetine on opioid use and pain after total knee arthroplasty: a triple-blinded randomized controlled trial. J Arthroplasty. 2022;37(6S):S147–54.
Koh IJ, Kim MS, Sohn S, et al. Duloxetine reduces pain and improves quality of recovery following total knee arthroplasty in centrally sensitized patients: a prospective, randomized controlled study. J Bone Joint Surg Am. 2019;101(1):64–73.
Page MJ, Moher D, Bossuyt PM, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160.
Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American pain society, the American society of regional anesthesia and pain medicine, and the American society of anesthesiologists’ committee on regional anesthesia, executive committee, and administrative council. J Pain. 2016;17(2):131–57.
Dworkin RH, Turk DC, Farrar JT, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113(1–2):9–19.
Centers for Disease Control and Prevention. Analyzing Prescription Data and Morphine Milligram Equivalents (MME). https://www.cdc.gov/opioids/data-resources/index.html. Accessed 28 Mar 2023.
Lossio-Ventura JA, Song W, Sainlaire M, et al. Opioid2MME: standardizing opioid prescriptions to morphine milligram equivalents from electronic health records. Int J Med Inform. 2022;162:104739.
Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Ding ZC, Li H, Huang C, et al. Significant analgesic benefits of perioperative duloxetine in patients who have depressive symptoms undergoing total hip arthroplasty: A randomized controlled trial. J Arthroplasty. 2023;38(3):519–24.
Ho KY, Tay W, Yeo MC, et al. Duloxetine reduces morphine requirements after knee replacement surgery. Br J Anaesth. 2010;105(3):371–6.
Kim MS, Koh IJ, Sung YG, et al. Preemptive duloxetine relieves postoperative pain and lowers wound temperature in centrally sensitized patients undergoing total knee arthroplasty: a randomized, double-blind, placebo-controlled trial. J Clin Med. 2021;10(13):2809.
Li H, Zeng WN, Ding ZC, et al. Duloxetine reduces pain after total hip arthroplasty: a prospective, randomized controlled study. BMC Musculoskelet Disord. 2021;22(1):492.
Rienstra W, Blikman T, Dijkstra B, et al. Effect of preoperative duloxetine treatment on postoperative chronic residual pain after total hip or knee arthroplasty: a randomised controlled trial. BMJ Open. 2021;11(11):e052944.
YaDeau JT, Brummett CM, Mayman DJ, et al. Duloxetine and subacute pain after nnee arthroplasty when added to a multimodal analgesic regimen: a randomized, placebo-controlled, triple-blinded trial. Anesthesiology. 2016;125(3):561–72.
Ljungqvist O, de Boer HD, Balfour A, et al. Opportunities and challenges for the next phase of enhanced recovery after surgery: a review. JAMA Surg. 2021;156(8):775–84.
Kehlet H, Dahl JB. Anaesthesia, surgery, and challenges in postoperative recovery. Lancet. 2003;362(9399):1921–8.
Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. Pain. 2011;152(3 Suppl):S2-s15.
Fillingham YA, Hannon CP, Buvanendran A, et al. Multimodal analgesia for hip and knee arthroplasty: eliminating opioids as the cornerstone of postoperative pain management. J Arthroplasty. 2020;35(10):2695–6.
Brannan SK, Mallinckrodt CH, Detke MJ, et al. Onset of action for duloxetine 60 mg once daily: double-blind, placebo-controlled studies. J Psychiatr Res. 2005;39(2):161–72.
Wang CF, Russell G, Wang SY, et al. R-duloxetine and n-methyl duloxetine as novel analgesics against experimental postincisional pain. Anesth Analg. 2016;122(3):719–29.
Wang CF, Russell G, Strichartz GR, et al. The local and systemic actions of duloxetine in allodynia and hyperalgesia using a rat skin incision pain model. Anesth Analg. 2015;121(2):532–44.
Onuţu AH. Duloxetine, an antidepressant with analgesic properties - a preliminary analysis. Rom J Anaesth Intensive Care. 2015;22(2):123–8.
Miller A, Roth T, Roehrs T, et al. Correlation between sleep disruption on postoperative pain. Otolaryngol Head Neck Surg. 2015;152(5):964–8.
Kluge M, Schüssler P, Steiger A. Duloxetine increases stage 3 sleep and suppresses rapid eye movement (REM) sleep in patients with major depression. Eur Neuropsychopharmacol. 2007;17(8):527–31.
Chellappa SL, Aeschbach D. Sleep and anxiety: From mechanisms to interventions. Sleep Med Rev. 2022;61:101583.
Doghramji K. Sleep extension in sleepy individuals reduces pain sensitivity: new evidence regarding the complex, reciprocal relationship between sleep and pain. Sleep. 2012;35(12):1587–8.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhong, H., Li, J., Chen, Y. et al. Effect of duloxetine on pain and opioid consumption after total knee and hip arthroplasty: a systematic review and meta-analysis of randomized controlled trials. Int J Clin Pharm 46, 14–25 (2024). https://doi.org/10.1007/s11096-023-01593-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-023-01593-x