Abstract
Background
Within the quality use of medicines (QUM)—which entails timely access to, and the rational use of, medicines—medicine safety is a global health priority. In multicultural countries, such as Australia, national medicines policies are focused on achieving QUM, although this is more challenging among their Culturally and Linguistically Diverse (CALD) patients (i.e., those from ethnic minority groups).
Aim
This review aimed to identify and explore the specific challenges to achieving QUM, as experienced by CALD patients living in Australia.
Method
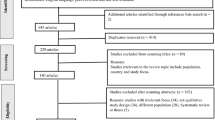
A systematic literature search was conducted using Web of Science, Scopus, Academic search complete, CINHAL, PubMed and Medline. Qualitative studies describing any aspects of QUM among CALD patients in Australia were included.
Results
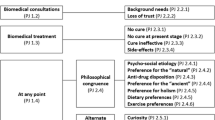
Major challenges in facilitating QUM among CALD patients in Australia were identified, particularly in relation to the following medicines management pathway steps: difficulties around participation in treatment decision-making alongside deficiencies in information provision about medicines. Furthermore, medication non-adherence was commonly observed and reported. When mapped against the bio-psycho-socio-systems model, the main contributors to the medicine management challenges identified related to “social” and “system” factors, reflecting the current health-system’s lack of capacity and resourcing to respond to patients’ low health literacy levels, communication and language barriers, and cultural and religious perceptions about medicines.
Conclusion
QUM challenges were different among different ethnic groups. This review suggests a need to engage with CALD patients in co-designing culturally appropriate resources and/or interventions to enable the health-system to address the identified barriers to QUM.


Similar content being viewed by others
References
Pharmaceutical Society of Australia. 2019. https://www.psa.org.au/medicine-safety-to-be-the-10th-national-health-priority-area/. Accessed 21 Jan 2023.
McLachlan AJ, Aslani P. National Medicines Policy 2.0: a vision for the future. Aust Prescr. 2020;43(1):24–6. https://doi.org/10.18773/austprescr.2020.007.
Nørgaard L, Cantarero-Arévalo L, Håkonsen H. The meeting between ethnic minorities, medicine use and the Nordic countries: an overview of theory-based intervention studies and lessons learned. Res Social Adm Pharm. 2017;13:e5. https://doi.org/10.1016/j.sapharm.2017.02.073.
Pearson SA, Pratt N, de Oliveira Costa J, et al. Generating real-world evidence on the quality use, benefits and safety of medicines in Australia: History, challenges and a roadmap for the future. Int J Environ Res Public Health. 2021;18(24):13345. https://doi.org/10.3390/ijerph182413345.
Bates DW. Preventing medication errors: a summary. Am J Health Syst Pharm. 2007;64(14 Suppl 9):S3–9; quiz S24–6. https://doi.org/10.2146/ajhp070190.
Chauhan A, Walton M, Manias E, et al. The safety of health care for ethnic minority patients: a systematic review. Int J Equity Health. 2020;19(1):118. https://doi.org/10.1186/s12939-020-01223-2.
Gordon KJ, Smith FJ, Dhillon S. The development and validation of a screening tool for the identification of patients experiencing medication-related problems. Int J Pharm Pract. 2005;13(3):187–93. https://doi.org/10.1211/ijpp.13.3.0004.
Stowasser DA, Allinson YM, O’Leary M. Understanding the medicines management pathway. J Pharm Pract Res. 2004;34(4):293–6. https://doi.org/10.1002/jppr2004344293.
Pham TTL, Berecki-Gisolf J, Clapperton A, et al. Definitions of culturally and linguistically diverse (CALD): a literature review of epidemiological research in Australia. Int J Environ Res Public Health. 2021;18(2):737. https://doi.org/10.3390/ijerph18020737.
Singh M, de Looper M. Australian health inequalities: birthplace. Canberra: AIHW; 2002.
Australian Bureau of Statistics (ABS). Census reveals a fast changing, culturally diverse nation 2016. https://www.abs.gov.au/ausstats/abs@.nsf/lookup/Media%20Release3. Accessed 21 Jan 2023.
Schwappach DL, Meyer Massetti C, Gehring K. Communication barriers in counselling foreign-language patients in public pharmacies: threats to patient safety? Int J Clin Pharm. 2012;34(5):765–72. https://doi.org/10.1007/s11096-012-9674-7.
Herrera H, Alsaif M, Khan G, et al. Provision of bilingual dispensing labels to non-native english speakers: an exploratory study. Pharmacy (Basel). 2019;7(1):32. https://doi.org/10.3390/pharmacy7010032.
Alhomoud F, Dhillon S, Aslanpour Z, et al. Medicine use and medicine-related problems experienced by ethnic minority patients in the United Kingdom: a review. Int J Pharm Pract. 2013;21(5):277–87. https://doi.org/10.1111/ijpp.12007.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71.
Saleem A, Steadman KJ, Fejzic J. Utilisation of healthcare services and medicines by Pakistani migrants residing in high income countries: a systematic review and thematic synthesis. J Immigr Minor Health. 2019;21(5):1157–80. https://doi.org/10.1007/s10903-018-0840-4.
Sattar R, Lawton R, Panagioti M, et al. Meta-ethnography in healthcare research: a guide to using a meta-ethnographic approach for literature synthesis. BMC Health Serv Res. 2021;21(1):50. https://doi.org/10.1186/s12913-020-06049-w.
Bunge M. How does it work?: The search for explanatory mechanisms. Philos Soc Sci. 2004;34(2):182–210. https://doi.org/10.1177/0048393103262550.
Buchman DZ, Skinner W, Illes J. Negotiating the relationship between addiction, ethics, and brain science. AJOB Neurosci. 2010;1(1):36–45. https://doi.org/10.1080/21507740903508609.
Critical Appraisal Skills Programme. CASP (Qualitative) Checklist 2018. https://casp-uk.net/casp-tools-checklists/. Accessed 22 Jan 2023.
Quine S. Health concerns and expectations of Anglo and ethnic older Australians: a comparative approach. J Cross Cult Gerontol. 1999;14(2):97–111. https://doi.org/10.1023/a:1006616230564.
White L, Klinner C. Medicine use of elderly Chinese and Vietnamese immigrants and attitudes to home medicines review. Aust J Prim Health. 2012;18(1):50–5. https://doi.org/10.1071/PY10099.
Bolton P, Hammoud S, Leung J. Issues in Quality use of medicines in two non-english speaking background communities. Aust J Prim Health. 2002;8(3):75–80. https://doi.org/10.1071/PY02046.
Blennerhassett J, Hilbers J. Medicine management in older people from non-english speaking backgrounds. J Pharm Pract Res. 2011;41(1):33–6. https://doi.org/10.1002/j.2055-2335.2011.tb00063.x.
Shaw J, Zou X, Butow P. Treatment decision making experiences of migrant cancer patients and their families in Australia. Patient Educ Couns. 2015;98(6):742–7. https://doi.org/10.1016/j.pec.2015.01.012.
Williams A, Manias E, Cross W, et al. Motivational interviewing to explore culturally and linguistically diverse people’s comorbidity medication self-efficacy. J Clin Nurs. 2015;24(9–10):1269–79. https://doi.org/10.1111/jocn.12700.
O’Callaghan C, Quine S. How older Vietnamese Australian women manage their medicines. J Cross Cult Gerontol. 2007;22(4):405–19. https://doi.org/10.1007/s10823-007-9045-3.
Alzayer R, Chaar B, Basheti I, et al. Asthma management experiences of Australians who are native Arabic speakers. J Asthma. 2018;55(7):801–10. https://doi.org/10.1080/02770903.2017.1362702.
Alzubaidi H, Mc Mamara K, Chapman C, et al. Medicine-taking experiences and associated factors: comparison between Arabic-speaking and Caucasian English-speaking patients with Type 2 diabetes. Diabet Med. 2015;32(12):1625–33. https://doi.org/10.1111/dme.12751.
Almansour H, Chaar B, Saini B. Perspectives and experiences of patients with type 2 diabetes observing the Ramadan fast. Ethn Health. 2016;23:1–17. https://doi.org/10.1080/13557858.2016.1269156.
Ahmad A, Khan M, Aslani P. A Qualitative Study on Medication Taking Behaviour Among People With Diabetes in Australia. Front Pharmacol. 2021;12:1–10. https://doi.org/10.3389/fphar.2021.693748.
Bellamy K, Ostini R, Martini N, et al. Perspectives of resettled African refugees on accessing medicines and pharmacy services in Queensland, Australia. Int J Pharm Pract. 2017;25(5):358–64. https://doi.org/10.1111/ijpp.12324.
Mohammad A, Saini B, Chaar BB. Exploring culturally and linguistically diverse consumer needs in relation to medicines use and health information within the pharmacy setting. Res Social Adm Pharm. 2015;11(4):545–59. https://doi.org/10.1016/j.sapharm.2014.11.002.
Clark A, Gilbert A, Rao D, et al. “Excuse me, do any of you ladies speak English?” Perspectives of refugee women living in South Australia: barriers to accessing primary health care and achieving the Quality Use of Medicines. Aust J Prim Health. 2014;20(1):92–7. https://doi.org/10.1071/PY11118.
Whittaker A, Lohm D, Lemoh C, et al. Investigating understandings of antibiotics and antimicrobial resistance in diverse ethnic communities in Australia: findings from a qualitative study. Antibiotics (Basel). 2019;8(3):135. https://doi.org/10.3390/antibiotics8030135.
El Samman F, Chaar BB, McLachlan AJ, et al. Medicines and disease information needs of older Arabic-speaking Australians. Australas J Ageing. 2013;32(1):28–33. https://doi.org/10.1111/j.1741-6612.2012.00587.x.
Alzubaidi H, Marriott J. Patient involvement in social pharmacy research: Methodological insights from a project with Arabic-speaking immigrants. Res Social Adm Pharm. 2014;10(6):924–25. https://doi.org/10.1016/j.sapharm.2014.08.008.
Abdelmessih E, Simpson MD, Cox J, et al. Exploring the health care challenges and health care needs of arabic-speaking immigrants with cardiovascular disease in Australia. Pharmacy (Basel). 2019;7(4):151. https://doi.org/10.3390/pharmacy7040151.
Malhotra R, Bautista MAC, Tan NC, et al. Bilingual text with or without pictograms improves elderly Singaporeans’ understanding of prescription medication labels. Gerontologist. 2019;59(2):378–90. https://doi.org/10.1093/geront/gnx169.
Shnaigat M, Downie S, Hosseinzadeh H. Effectiveness of health literacy interventions on COPD self-management outcomes in outpatient settings: a systematic review. COPD. 2021;18(3):367–73. https://doi.org/10.1080/15412555.2021.1872061.
Culhane-Pera KA, Pergament SL, Kasouaher MY, et al. Diverse community leaders’ perspectives about quality primary healthcare and healthcare measurement: qualitative community-based participatory research. Int J Equity Health. 2021;20(1):226. https://doi.org/10.1186/s12939-021-01558-4.
Youssef J, Deane FP. Arabic-speaking religious leaders’ perceptions of the causes of mental illness and the use of medication for treatment. Aust N Z J Psychiatry. 2013;47(11):1041–50. https://doi.org/10.1177/0004867413499076.
Kirkpatrick CMJ, Roughead EE, Monteith GR, et al. Consumer involvement in quality use of medicines (QUM) projects – lessons from Australia. BMC Health Serv Res. 2005;5(1):75. https://doi.org/10.1186/1472-6963-5-75.
Funding
No specific funding was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sawalha, R., Hosseinzadeh, H. & Bajorek, B. Culturally and linguistically diverse patients’ perspectives and experiences on medicines management in Australia: a systematic review. Int J Clin Pharm 45, 814–829 (2023). https://doi.org/10.1007/s11096-023-01560-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-023-01560-6