Abstract
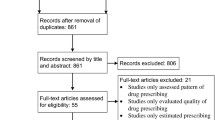
Background Drug-drug interactions are frequently observed in kidney transplant recipients due to polypharmacy and use of immunosuppressants. However, there is only one study evaluating clinically relevant potential drug-drug interactions of immunosuppressants specially in kidney transplant recipients by means of online databases and Stockleys Drug Interactions, as a gold standard. Aim This study aimed to compare four online databases used frequently to determined clinically relevant potential drug-drug interactions of immunosuppressants in kidney transplant recipients according to the Renal Drug Handbook. Method This was a descriptive cross-sectional study conducted between October 1, 2019, and March 18, 2020, in the nephrology ward of Ankara University School of the Medicine, Ibn-i Sina Hospital. In total, 52 adult patients’ discharge prescriptions were retrieved from their medical records and analyzed retrospectively. Micromedex®, Lexicomp®, Medscape, and Drugs.com databases were used to evaluate drug interactions. The Renal Drug Handbook was used as a gold standard to do specificity and sensitivity analysis. Results A total of 127 potential drug-drug interactions between the immunosuppressants and co-medications were detected by at least one online database. 32 (25.2%) of these were approved as clinically relevant potential drug-drug interactions by the Renal Drug Handbook. Lexicomp® and Drugs.com have exhibited the highest sensitivity (0.72 and 0.75) while Micromedex® has shown the highest specifity (0.83). Furthermore, the highest positive predictive value has been observed in Micromedex® (0.53). Micromedex® and Medscape had the highest negative predictive value (0.83 and 0.82). However, the kappa value of all was low. The values of inter-rater agreement (Kappa index) between online databases and the Renal Drug Handbook were weak (range 0.05–0.36). In addition, only 11 (8.7%) of potential drug-drug interactions were identified by all online databases. Conclusion This study showed that there was a weak compatibility between each database examined and the Renal Drug Handbook to detect clinically relevant potential drug-drug interactions for immunosuppressants in kidney transplant recipients. Therefore, we suggest that although databases might be practical to take a quick glance in detection of potential drug-drug interactions between immunosuppressants and co-medications, the data should be evaluated in detail and interpreted with caution in combination with a reference book like Renal Drug Handbook.


Similar content being viewed by others
References
Cameron J, Whiteside C, Katz J, et al. Differences in quality of life across renal replacement therapies: a meta-analytic comparison. Am J Kidney Dis. 2000;35:629–37.
Tonelli M, Wiebe N, Knoll G, et al. Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant. 2011;11:2093–109.
Ojo AO, Hanson JA, Wolfe RA, et al. Longterm survival in renal transplant recipients with graft function. Kidney Int. 2000;57:307–13.
World Health Organization (WHO) and the Spanish Transplant Organization, Organización Nacional de Trasplantes (ONT). Global Observatory on Donation and Transplantation. Available from:http://www.transplant-observatory.org/. Accessed 19.04.2021.
Turkish Society of Nephrology. Registry of the Nephrology, Dialysis and Transplantation in Turkey, Registry 2020. ISBN 978-605-62465-0-0. Available from: https://www.nefroloji.org.tr/icerik.php?gid=88. Accessed 10.05.2021.
Bauer AC, Franco RF, Manfro RC. Immunosuppression in kidney transplantation: state of the art and current protocols. Curr Pharm Des. 2020;26(28):3440–50.
Stemer G, Lemmens-Gruber R. Clinical pharmacy services and solid organ transplantation: a literature review. Pharm World Sci. 2010;32(1):7–18.
Al Raiisi F, Stewart D, Fernandez-Llimos F, et al. Clinical pharmacy practice in the care of chronic kidney disease patients: a systematic review. Int J Clin Pharm. 2019;41(3):630–66.
Leape LL, Bates DW, Cullen DJ, et al. Systems analysis of adverse drug events. ADE Prevent Study Group JAMA. 1995;274:35–43.
Leape LL, Berwick DM. Five years after To Err Is Human: what have we learned? JAMA. 2005;293:2384–90.
Tecen-Yucel K, Bayraktar-Ekincioglu A, Yildirim T, et al. Assessment of clinically relevant drug interactions by online programs in renal transplant recipients. J Manag Care Spec Pharm. 2020;26(10):1291–6.
Amkreutz J, Koch A, Buendgens L, et al. Clinical decision support systems differ in their ability to identify clinically relevant drug interactions of immunosuppressants in kidney transplant patients. J Clin Pharm Ther. 2017;42(3):276–85.
Vonbach P, Dubied A, Krähenbühl S, et al. Evaluation of frequently used drug interaction screening programs. Pharm World Sci. 2008;30(4):367–74.
Moradi O, Karimzadeh I, Davani-Davari D, et al. Drug-drug interactions among kidney transplant recipients in the outpatient setting. Int J Organ Transplant Med. 2020;11(4):185–95.
Smith WD, Hatton RC, Fann AM, et al. Evaluation of drug interaction software to identify alerts for transplant medications. Ann Pharmacother. 2005;39(1):45–50.
Riu-Viladoms G, San Martín EC, Martín-Conde MT, et al. Drug interactions with oral antineoplastic drugs: The role of the pharmacist. Eur J Cancer Care (Engl). 2019;28(1):e12944.
Kheshti R, Aalipour M, Namazi S. A comparison of five common drug–drug interaction software programs regarding accuracy and comprehensiveness. J Res Pharm Pract. 2016;5:257.
Akdemir-Kalkan I, Cinar G, Pehlivanli A, et al. Pattern of systemic antibiotic use and potential drug interactions: Evaluations through a point prevalence study in Ankara University Hospitals. Turk J Med Sci. 2021;51(2):523–9.
O’Shaughnessy M, Allen N, O’Regan J, et al. Agreement between renal prescribing references and determination of prescribing appropriateness in hospitalized patients with chronic kidney disease. QJM. 2017;110(10):623–8.
Jodoin K. The renal drug handbook the ultimate prescribing guide for renal practitioners, 4th edition. Eur J Hosp. 2016;23:248.
IBM Micromedex® Web Applications Access. Drug interactions checker. Available from: https://www.micromedexsolutions.com/micromedex2/librarian/PFDefaultActionId/pf.LoginAction. Accessed 29.06.2021.
Wolters Kluwer. Lexicomp. Database. Available from: https://www.wolterskluwercdi.com/lexicomp-online/. Accessed 29.03.2021.
Medscape. Drug interaction checker. Available from: https://reference.medscape.com/drug-interactionchecker. Accessed 29.03.2021.
Drugs.com. Drug interaction checker. Available from: https://www.drugs.com/interaction/list/. Accessed 29.03. 2021.
Ashley C, Dunleavy A. The Renal Drug Handbook: The Ultimate Prescribing Guide for Renal Practitioners. 5th Edition. CRC Press; 2018. ISBN-13978–1–138–62479–5.
Daniel WW, Cross CL. Biostatistics: a foundation for analysis in the health sciences. Hoboken: Wiley; 2013. ISBN 978-1-118-30279-8.
Lwanga SK, Lemeshow S, World Health Organization. Sample size determination in health studies: a practical manual / S. K. Lwanga and S. Lemeshow. Geneva: World Health Organization; 1991. Available from: http://www.who.int/iris/handle/10665/40062. Accessed 10.08.2021.
Bril F, Castro V, Centurion IG, et al. A systematic approach to assess the burden of drug interactions in adult kidney transplant patients. Curr Drug Saf. 2016;11(2):156–63.
Anthony J, Viere MD, Garrett PD. Understanding interobserver agreement: The kappa statistic. Fam Med. 2005;37(5):360–2.
Smith WD, Hatton RC, Fann AL, et al. Evaluation of drug interaction software to identify alerts for transplant medications. Ann Pharmacother. 2005;39:45–50.
Vonbach P, Dubied A, Krahenbuhl S, et al. Evaluation of frequently used drug interaction screening programs. Pharm World Sci. 2008;30:367–74.
Reis AMM, Cassiani SHDB. Evaluation of three brands of drug interaction software or use in intensive care units. Pharm World Sci. 2010;32:822–8.
Saverno KR, Hines LE, Warholak TL, et al. Ability of pharmacy clinical decision-support software to alert users about clinically important drug–drug interactions. J Am Med Inform Assoc. 2011;18:32–7.
Coleman JJ, van der Sijs H, Haefeli WE, et al. On the alert: future priorities for alerts in clinical decision support for computerized physician order entry identified from a European workshop. BMC Med Inform Decis Mak. 2013;13:111.
Abarca J, Malone DC, Armstrong EP, et al. Concordance of severity ratings provide in four drug interaction compendia. J Am Pharm Assoc. 2004;44:136–41.
Scheife RT, Hines LE, Boyce RD, et al. Consensus recommendations for systematic evaluation of drug–drug interaction evidence for clinical decision support. Drug Saf. 2015;38:197–206.
Zorina OI, Haueis P, Greil W, et al. Comparative performance of two drug interaction screening programmes analysing a crosssectional prescription dataset of 84,625 psychiatric inpatients. Drug Saf. 2013;36:247–58.
Acknowledgements
The authors received no specific funding for this work.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors have no potential conflict of interest that might be relevant to the contents of this manuscript.
Ethical approval
Ethical approval was obtained from Ethics Committee for Human Research of the School of Medicine at Ankara University.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pehlivanli, A., Eren-Sadioglu, R., Aktar, M. et al. Potential drug-drug interactions of immunosuppressants in kidney transplant recipients: comparison of drug interaction resources. Int J Clin Pharm 44, 651–662 (2022). https://doi.org/10.1007/s11096-022-01385-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-022-01385-9