Abstract
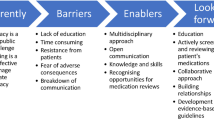
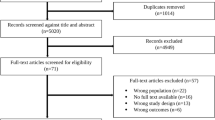
Background Understanding how patient values and preferences towards polypharmacy and deprescribing have been studied is important to gain insight on current knowledge in this area and to identify knowledge gaps. Aim To describe methods and outcomes for studying patient values and preferences towards polypharmacy and deprescribing, and to identify gaps in the existing literature. Method A scoping review was conducted on English-language studies that examined patient preferences and values related to polypharmacy and/or deprescribing among community-dwelling adults. MEDLINE, Embase, PubMed, PsycINFO, EconLit, Social Science Citation Index, Science Citation Index Expanded, International Pharmaceutical Abstracts, and CINAHL/AgeLine were searched. Results Thirty articles were included. Surveys (n = 17, 56.7%), interviews/focus groups (n = 9, 30.0%), and mixed methods (n = 3, 10.0%), were commonly used methods. Patients Attitudes Towards Deprescribing (PATD) was the most common tool used (n = 9, 30.0%). Twelve themes related to attitudes, social pressure, and control of polypharmacy/deprescribing were identified. The most frequently-encountered themes included desire or willingness to reduce medication load and influence of healthcare provider on medication use. Conclusion PATD was commonly used to assess preferences and values towards polypharmacy and limited knowledge on patient-important outcomes were addressed. Future research should focus on shared decision-making and communicating risk versus benefit of medications.

Similar content being viewed by others
References
Maher RL, Hanlon J, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf. 2014;13(1):57–65.
Cantlay A, Glyn T, Barton N. Polypharmacy in the elderly. InnovAiT. 2016;9(2):69–77.
Canadian Institute for Health Information. Seniors and the health care system: what is the impact of multiple chronic conditions? (2011). Available: https://secure.cihi.ca/free_products/air-chronic_disease_aib_en.pdf. Accessed 27 Jan 2021.
Reason B, Terner M, Moses McKeag A, Tipper B, Webster G. The impact of polypharmacy on the health of Canadian seniors. Fam Pract. 2012;29(4):427–32.
Fick DM, Semla TP, Steinman M, et al. American Geriatrics Society 2019 updated AGS beers criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674–94.
O'Mahony D, O'Sullivan D, Byrne S, O'Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2014;44(2):213–8.
Bruyere Research Institute Deprescribing Guidelines Research Team. Deprescribing Guidelines and Algorithms. Available: deprescribing.org. Accessed 2 July 2021.
Institute of Medicine (US) Committee on Quality of Health Care in America, Crossing the quality chasm: a new health system for the 21st century, National Academies Press; 2001.
National Institute for Health and Care Excellence (NICE) 2021. Standards framework for shared-decision-making support tools, including patient decisión aids (ECD8). Published 17 June 2021. Available: www.nice.org/uk/corporate/ecd8. Accessed 13 July 2021.
Munro S, Stacey D, Lewis KB, Bansback N. Choosing treatment and screening options congruent with values: Do decision aids help? Sub-analysis of a systematic review. Patient Educ Couns. 2016;99:491–500.
Llewellyn-Thomas HA, Crump RT. Decision support for patients values clarification and preference elicitation. Med Care Res Rev. 2013;70(1 suppl):50S-79S.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5:210–20. https://doi.org/10.1186/s13643-016-0384-4.
Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–73.
Rich A, Brandes K, Mullan B, Hagger MS. Theory of planned behavior and adherence in chronic illness: a meta-analysis. J Behav Med. 2015;38:673–88.
Martin P, Tannenbaum C. A realist evaluation of patients’ decisions to deprescribe in the EMPOWER trial. BMJ Open. 2017;7(4):e015959.
Michie S, Dormandy E, Marteau TM. The multi-dimensional measure of informed choice: a validation study. Patient Educ Couns. 2002;48(1):87–91.
Aoki T, Yamamoto Y, Ikenoue T, Fukuhara S. Factors associated with patient preferences towards deprescribing: a survey of adult patients on prescribed medications. Int J Clin Pharm. 2019;41(2):531–7.
Kua KP, Saw PS, Lee SWH. Attitudes towards deprescribing among multi-ethnic community-dwelling older patients and caregivers in Malaysia: a cross-sectional questionnaire study. Int J Clin Pharm. 2019;41(3):793–803.
Tegegn HG, Tefera YG, Erku DA, Haile KT, Abebe TB, Chekol F, et al. Older patients’ perception of deprescribing in resource-limited settings: a cross-sectional study in an Ethiopia university hospital. BMJ Open. 2018;8(4):020590.
Kovačević SV, Miljković B, Vučićević K, Ćulafić M, Kovačević M, Golubović B, et al. Elderly polypharmacy patients’ needs and concerns regarding medication assessed using the structured patient-pharmacist consultation model. Patient Educ Couns. 2017;100(9):1714–9.
Schiøtz ML, Frølich A, Jensen AK, Reuther L, Perrild H, Petersen TS, et al. Polypharmacy and medication deprescribing: a survey among multimorbid older adults in Denmark. Pharmacol Res Perspect. 2018;6(6):e00431.
Sirois C, Ouellet N, Reeve E. Community-dwelling older people’s attitudes towards deprescribing in Canada. Res Soc Adm Pharm. 2017;13(4):864–70.
Leydon GM, Rodgers L, Kendrick T. A qualitative study of patient views on discontinuing long-term selective serotonin reuptake inhibitors. Fam Pract. 2007;24(6):570–5.
Horner E, Fleming J, Studd J. A study of women on long-term hormone replacement therapy and their attitude to suggested cessation. Climatcteric. 2006;9(6):459–63.
Hopper I, de Silva C, Skiba M, Tonkin A, Krum H. Attitudes of patients and prescribing clinicians to polypharmacy and medication withdrawal in heart failure. J Card Fail. 2016;22(9):743–4.
Ng WL, Tan MZW, Koh EYL, Tan NC. Deprescribing: What are the views and factors influencing this concept among patients with chronic diseases in a developed Asian community? Proc Singap Healthc. 2017;26(3):172–9.
Straand J, Sandvik H. Stopping long-term drug therapy in general practice. How well do physicians and patients agree? Fam Pract. 2001;18(6):597–601.
Turner JP, Tannenbaum C. Older adults’ awareness of deprescribing: a population-based survey. J Am Geriatr Soc. 2017;65(12):2691–6.
Jia Hao L, Omar MS, Tohit N. Polypharmacy and willingness to deprescribe among elderly with chronic diseases. Int J Gerontol. 2018;12(4):340–3.
Linsky A, Simon SR, Stolzmann K, Meterko M. Patient attitudes and experiences that predict medication discontinuation in the Veterans Health Administration. J Am Pharm Assoc (2003). 2018;58(1):13–20.
Linsky A, Meterko M, Bokhour BG, Stolzmann K, Simon SR. Deprescribing in the context of multiple providers: Understanding patient preferences. Am J Manag Care. 2019;25(4):192–8.
Reeve E, Wiese MD, Hendrix I, Roberts MS, Shakib S. People’s attitudes, beliefs, and experiences regarding polypharmacy and willingness to deprescribe. J Am Geriatr Soc. 2013;61(9):1508–14.
Reeve E, Low L-F, Hilmer SN. Attitudes of older adults and caregivers in Australia toward deprescribing. J Am Geriatr Soc. 2019;67(6):1204–10.
Iliffe S, Curran HV, Collins R, Fletcher S, Woods B. Attitudes to long-term use of benzodiazepine hypnotics by older people in general practice: findings from interviews with service users and providers. Aging Ment Health. 2004;8(3):242–8.
Schöpf AC, Von Hirschhausen M, Farin E, Maun A. Elderly patients’ and GPs’ perspectives of patient-GP communication concerning polypharmacy: a qualitative interview study. Prim Health Care Res Dev. 2018;19(4):355–64.
Weir K, Nickel B, Naganathan V, Bonner C, McCaffery K, Carter SM, et al. Decision-making preferences and deprescribing: perspectives of older adults and companions about their medicines. J Gerontol B Psychol Sci Soc Sci. 2018;73(7):e98–107.
Krska J, Morecroft CW, Poole H, Rowe PH. Issues potentially affecting quality of life arising from long-term medicines use: a qualitative study. Int J Clin Pharm. 2013;35(6):1161–9.
Cook JM, Biyanova T, Masci C, Coyne JC. Older patient perspectives on long-term anxiolytic benzodiazepine use and discontinuation: a qualitative study. Med. 2007;22:1094–100.
Linsky A, Simon SR, Bokhour B. Patient perceptions of proactive medication discontinuation. Patient Educ Couns. 2015;98(2):220–5.
Moen J, Bohm A, Tillenius T, Antonov K, Nilsson JLG, Ring L. “I don’t know how many of these [medicines] are necessary..”—a focus group study among elderly users of multiple medicines. Patient Educ Couns. 2009;74(2):135–41.
Williams B, Shaw A, Durrant R, de Lusignan S. Patient perspectives on multiple medications versus combined pills: a qualitative study. QJM. 2005;98(12):885–93.
Reeve E, Low L-F, Hilmer SN. Beliefs and attitudes of older adults and carers about deprescribing of medications: a qualitative focus group study. Br J Gen Pract. 2016;66(649):e552–60.
Clyne B, Cooper JA, Boland F, Hughes CM, Fahey T, Smith SM, et al. Beliefs about prescribed medication among older patients with polypharmacy: a mixed methods study in primary care. Br J Gen Pract. 2017;67(660):e507–18.
Luymes CH, Boelhouwer NJ, Poortvliet RKE, de Ruijter W, Reis R, Numans ME. Understanding deprescribing of preventive cardiovascular medication: a Q-methodology study in patients. Patient Prefer Adherence. 2017;11:975–84.
McKillop G, Joy J. Patients’ experience and perceptions of polypharmacy in chronic kidney disease and its impact on adherent behaviour. J Ren Care. 2013;39(4):200–7.
Reeve E, Shakib S, Hendrix I, Roberts MS, Wiese MD. Development and validation of the patients’ attitudes towards deprescribing (PATD) questionnaire. Int J Clin Pharm. 2013;35(1):51–6.
Neame R, Hammond A. Beliefs about medications: a questionnaire survey of people with rheumatoid arthritis. Rheumatol. 2005;44(6):762–7.
Bachinger SM, Kolk AM, Smets EM. Patients’ trust in their physician—psychometric properties of the Dutch version of the “Wake Forest Physician Trust Scale.” Patient Educ Couns. 2009;76(1):126–31.
Horne R, Weinman J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychom Res. 1999;47:555–67.
Eidam A, Roth A, Lacroix A, Goisser S, Seidling HM, Haefeli WE, et al. Methods to assess patient preferences in old age pharmacotherapy—a systematic review. Patient Prefer Adherence. 2020;14:467–97.
Mangin D, Stephen G, Bismah V, Risdon C. Making patient values visible in healthcare: a systematic review of tools to assess patient treatment priorities and preferences in the context of multimorbidity. BMJ Open. 2016;6:e010903.
Stacey D, Legare F, Lewis K, Barry MJ, Bennett CL, Eden KB et al. Decision aids for people facing health treatment or screening decisions. Cochrane Syst Rev. 2017;4:CD001431.
Acknowledgements
The authors would like to acknowledge funding from the College of Pharmacy, University of Manitoba for supporting Melissa Ireland and the Centre on Aging Research Team Small Grant for supporting Evan Forest to complete this work. The Centre on Aging did not have a role on the conduct of the scoping review. The authors would like to acknowledge the Neil John Maclean Library librarian, Janet Rothney, for her assistance with the scoping review search strategy and methods.
Funding
Centre on Aging Research Team Small Grant supported Evan Forest to complete this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
-
1.
*“Patient Acceptance of Health Care”/
-
2.
*Patients/ed, px [Education, Psychology]
-
3.
*Family/ed, px [Education, Psychology]
-
4.
*Patient Satisfaction/
-
5.
(choice$ or empower$).m_titl.
-
6.
((patient or patients or individuals or family or families or familial or kindred* or relative or relatives or care giver* or caregiver* or carer or carers) adj3 (preference* or input or experience or experiences or value or values or perspective* or expectation* or choice* or choose* or choosing or "day-to-day" or participat* or symptom or symptoms or limitations or survey* or lives or burden or attitude* or belief* or knowledge or lessons or reaction* or motivation* or intention* or involv* or engag* or consult* or interact* or dialog* or conversation* or decision* or decide* or deciding)).m_titl.
-
7.
(acceptance or acceptability or quality of life or satisfaction or compliance or adherence or cooperation or co-operation or nonadherence or noncompliance or interview*).m_titl.
-
8.
((patient or patients or proband* or individuals or survivor* or family or families or familial or kindred* or relative or relatives or care giver* or caregiver* or carer or carers) adj3 (preference* or input or experience or experiences or value or values or perspective* or expectation* or choice* or choose* or choosing or "day-to-day" or participat* or acceptance or acceptability or limitations or survey* or lives or interview* or quality of life or satisfaction or burden or attitude* or belief or knowledge or lessons or reaction* or motivation* or intention* or involvement or engag* or consult* or interact* or dialog* or conversation* or decision* or decide* or deciding or compliance or adherence or cooperation or co-operation or nonadherence or noncompliance)).ab. /freq = 2
-
9.
patient*.jw.
-
10.
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9
-
11.
exp *polypharmacy/
-
12.
deprescribing.mp.
-
13.
11 or 12
-
14.
10 and 13
-
15.
((patient or patients or individuals or family or families or familial or kindred* or relative or relatives or care giver* or caregiver* or carer or carers) adj3 (preference* or input or views or experience or experiences or value or values or perspective* or expectation* or choice* or choose* or choosing or "day-to-day" or participat* or symptom or symptoms or limitations or survey* or lives or burden or attitude* or belief* or knowledge or lessons or reaction* or motivation* or intention* or involv* or engag* or consult* or interact* or dialog* or conversation* or decision* or decide* or deciding)).m_titl.
-
16.
((patient or patients or proband* or individuals or survivor* or family or families or familial or kindred* or relative or relatives or care giver* or caregiver* or carer or carers) adj3 (preference* or input or experience or experiences or value or values or perspective* or expectation* or choice* or choose* or choosing or "day-to-day" or participat* or acceptance or acceptability or limitations or survey* or lives or interview* or quality of life or satisfaction or burden or attitude* or belief or knowledge or lessons or reaction* or motivation* or intention* or views or involvement or engag* or consult* or interact* or dialog* or conversation* or decision* or decide* or deciding or compliance or adherence or cooperation or co-operation or nonadherence or noncompliance)).ab./freq = 2
-
17.
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 15 or 16
-
18.
13 and 17
Appendix 2: Data extraction table
First author | Year | Setting | Study design | Objective(s) | Polypharmacy definition | Medication(s) studied | Outcomes measured | Population | Sample size | Interventions/scale(s) | Results |
|---|---|---|---|---|---|---|---|---|---|---|---|
Kua, Kok Kim | 2019 | Malaysia | Multicenter cross-sectional study | Determine patients’ attitudes, beliefs, perceptions, and experiences regarding the number of medications they were taking and their opinions regarding deprescribing | "5 or more prescribed drugs" | Multiple/Nonspecific Polypharmacy (≥ 5 medications) | Patients’ and caregivers’ attitudes and beliefs towards reducing medications and characteristics of patients, such as age, gender, education level, number of medications taken and number of medical centers managing the patient | Patients ≥ 60, or their caregivers, who are taking ≥ 1 long-term medication. Living at home alone, at home with friends or family, or in a nursing/old folks home. Patient's took a median of 3 medications | Total N = 574 n = 336 recruited from community pharmacies (med. Age 66, range 60–91, 169 F) n = 336 recruited from health clinic (med. Age 67, r 60–93, 82 F) n = 32 care recipients, health clinic (med. Age 74, r 60–94, 23 F) n = 20 care recipients, community pharmacy (med. age 68, r 63–89, 10 F) | Participants completed the Revised Patients’ Attitudes Towards Deprescribing (rPATD questionnaire. The questionnaire has four domains: perceived burden of medication taking, belief in appropriateness of medication use, concerns about stopping the medication, and level of involvement/knowledge of medications | Older adult perceptions: Most were satisfied with their current medications (88.1%), 33.7% felt they were taking a large number of medications, 26.9% felt daily medications was very inconvenient, 33.1% felt medications were a burden, 66.7% would like to try stopping or reducing the dose of their medications, especially when doctor recommended. When stratified by location: Community pharmacy participants—66.3% felt they spend a lot of money on medications, 54.2% felt medications were a burden, 50% would like to reduce/stop medications. Analysis of total score for each domain revealed greater perceived burden, concerns about stopping, and involvement among participants from Health clinic compared to community pharmacies. Caregivers perceptions: 82.7% satisfaction towards care recipients medications, 50% would like to be more involved in recipient's management, 48.1% felt care recipient was taking a large amount of medications, 65.4% expressing willingness to stop/reduce drugs by doctor's recommendation Influence of characteristic's on willingness to deprescribe: Those ≥ 75 felt they needed to be more involved in decision making of their medications, and more willing for meds to be deprescribed. Participants with 1 doctor had lower scores of perceived burden and medication appropriateness |
Aoki, Takuya | 2019 | Japan | Nationwide cross-sectional survey | Investigate factors associated with patient preferences toward deprescribing in a representative sample in Japan | "Defined as the use of multiple regular medications for the treatment of one to several medical conditions and has the potential to increase the rates of adverse drug reactions, reduced quality of life, hospitalization, and mortality" (p. 532) | Multiple/Nonspecific *Non-Polypharmacy specific (≥ 1 med required. 23.53% of sample had polypharmacy) | Patients’ willingness to deprescribe, defined as a preference of withdrawal of one or more of inappropriate regular prescription medications under the supervision of doctors. As well, secondary analyses of the outcome in relation to treatment-related burden, health status, and demographic factors | Outpatients ≥ 18 taking ≥ 1 regular prescription medications | N = 1483 (590 ≥ 65 y/o; 728 F, mean age not reported; range 18—over 75) Total: 1483 participants, 590 were ≥ 65 (39.7%) 774 were multimorbid and 349 patients had polypharmacy | Patients’ willingness to deprescribe was assessed using a global question in the patients’ attitudes towards deprescribing (PATD) questionnaire “If my doctor said it was possible, I would be willing to stop one or more of my regular medications.” Participants were asked to rate this question on a 5-point Likert scale, and were identified as willing if they answered 1 = strongly agree and 2 = agree | 67.8% of patients were willing to deprescribe. 69.3% of patients aged ≥ 65 were willing to deprescribe (409). 73.9% of patients with polypharmacy were willing, 71.7% of multimorbid patients were willing. Multimorbidity and polypharmacy were positively associated with patients’ willingness to deprescribe. Similar associations were found with frequent visits to medical institutions and increasing age |
McKillop, Gus | 2013 | Scotland* | Mixed methods study | Gain a better understanding of adherent behaviour towards medications among people with CKD and inquire about patients feelings towards precribed medications | "For this study, polypharmacy is defined as the prescription of more than five different oral medicines." | Multiple/Nonspecific* (all patients diagnosed with CKD) Polypharmacy (≥ 5 medications) | Patients perceived adherence to medications, their attitudes towards adherence and reasons for/against, their general attitudes towards polypharmacy | Participants had a diagnosis of CKD, attended a nephrology clinic at a recruiting hospital, were prescribed 5 or more oral medications, and able to provide consent to interview. Average age was 60 (range = 29–82) | N = 10 (m age 60, range 29–82, 5 female) | Participants were interviewed using a general interview guide to determine their attitude's towards polypharmacy and adherence | Major themes were identified: General attitudes towards medicine—A variety of attitudes was apparent during the interview process, hostility towards medications, ambivalence towards the need for multiple medications and the desire to be taking as few medications as necessary emerged in several interviews, there was a tension between the recognition that multiple medicines were necessary and concerns about the long-term health effects of polypharmacy, concern was voiced around the potential for drug interactions, embarassment around taking so many medications was expressed by a participant—stating it contributed to poor adherence, Impact of complex medicine regimes—Many participants stated that complex medication regimes made nonadherence more likely and sometimes found it difficult to cope with the complexity of their prescriptions. Reasons for nonadherent behaviour—nonadherence occured for many different reasons, including increased pill burden, tiredness and feeling unwell, side effects, and forgetfullness. Reasons for adherence and long-term persistence with prescribed medicine—often adherence improved when the threat to health became more apparent. The relationship between patients and health care professionals—participants generally trusted the health professionals who were prescribing medicines for them, one felt angry that the reason for stopping a medicine was not adequately explained and focused on this issue in the interview. The prioritisation of medicines—most participants appeared to have weighed the comparative benefits of medicines and subsequently ranked some as more important than others, but not all participants came to the same conclusions in their rank of importance. Medicines perceived to be of direct benefit to kidney function were highlighted as a priority medicine, especially when participants believed there was potential to slow CKD progression |
Tegegn, Henok | 2018 | Ethiopia | Quantitative, cross-sectional survey | Assess older patients' attitude towards deprescribing of inappropiate medicines | "the practice of prescribing five or more medications to the same person," | Multiple/Nonspecific *Non-Polypharmacy specific (≥ 1 med required) | Identify older patients in Ethopias' attitude towards deprescribing | Patients aged 65 or older with at least one medication. Patients with severe physical or psychological problems who refused to participate were excluded | N = 316 (med age 70, IQR 67–75, 143 F) | Participants completed the Revised Patients’ Attitudes Towards Deprescribing (rPATD questionnaire, the scale was changed from the original 5 point Likert scale to a 4 point Likert scale (the midpoint "unsure' answer was removed). The previously validated tool "Belief in Medicine use Questionnaire-Overuse" was used for comparison and validation of the rPATD. It was also translated into Amharic. Most patients were interviewed due to low literacy of the participants | 62 participants (19.7%) were experiencing polypharmacy (the use of 5 or more medications). 67.7% thought they spent a lot of money on their medications, but 61.5% did not feel their medications were a burden to them. 50.6% felt they were taking a large number of medicines, 35.7% agreed that sometimes they felt they took too many medicines, 33.9% agreed they may be taking one or more medicines they no longer needed, 9.4% would like to try stopping one of their medicines to see how they felt without it, 90.2% felt one or more of their medications may not be working, 42.4% would like their doctor to reduce the dose of one or more of their medicines, 41.8% believed one or more of their medications was giving them side effects. 27.9% would be reluctant to stop a medicine they had been taking for a long time, 89.2% would worry about missing out on future benefits if one of their medicines was stopped, 46.9% feel stressed whenever changes are made to their medicines, 27.8% would feel their doctor was giving up on them if they recomendded stopping a medicine, 26.5% reported having a bad experience when stopping a medicine before. 67.4% report having a good understanding of the reasons they were prescribed each of their medicines, 60.5% like to know as much as possible about their medicines, 60.4% agreed they like to be involved in making decisions about their medicines with their doctors, 81.3% agreed they always ask their doctor, pharmacist, or other healthcare professional if there is something they don't understand about their medicines. 81.6% reported if their doctor said it was possible to stop one or more of their regular medicines they would be willing, and 92.1% agreed that overall they are satisfied with their current medicines. Patients who thought their medications were a burden to them were more likely to report side effects. Patient' willingness to stop their medications if their doctor was correlated with seven items on the rPATD—it was positively correlated even though they may be worried about missing out on future benefits and negatively correlated with the belief they were taking too many medications, were perceiving side effects, were reluctant to stop a medication they had been on for a long time, and perceieved their doctor’s were giving up on them if they recomendded stopping a medication |
Schöpf, Andrea | 2017 | Germany | Qualitative interview study | Gain initial insights into the perceptions of elderly patients and their GPs regarding communication on polypharmacy and medication safety, as well as empowerment approaches patients and GPs identify which might be useful to guide future research | ≥ 5 medications | Multiple/Nonspecific Polypharmacy (≥ 5 medications) | Differences in patient and practicioners' perceptions of communication about polypharmacy, medication plans/adherence, and responsibility | Patients aged 65 or older with polypharmacy (≥ 5 medications) (with their GPs in a German Primary Healthcare Centre) | Patients N = 6 (mean age 75, + − 4.8 yrs, 3 F) | Patients participated in semi-structured interviews consisting of open-ended questions, core questions, and additional questions associated with the core questions. All interviews were face-to-face (except one by telephone) | Dialogue concerning medications: whose responsibility? —Deprescribing potentially inappropriate medication: The patients fear that their condition might worsen and that they take up too much of the doctor's time, or they have concerns as the medication was prescribed by another specialist. In this sample it was usually the GPs who addressed potentially inappropriate medications, the GPs stated if patients ask for a discontinuation, they are usually young and only use the medication for a short time. One patient who stated that she had a good relationship with her doctor demonstrated her wish to discontinue a tablet, but then stated that she had to take the medicine in order to be an obedient patient. Another patient stated he had started the discontinuation process twice and the experience had differed strongly depending on the type of medication and the prescriber. Overall discussion: Patients' answeres initially implied that there are no communication problems and that they perceived the patient-GP communication regarding medication very open, but due to the qualitative nature of this study the narratives of patients necame more complete and it was possible to identify potentially problematic sequences during the interview course. Patients and GPs found it difficult to name ways of empowering patients to be more prepared for and active during medication discussions |
Clyne, Barbara | 2017 | Ireland | A convergent parallel mixed methods design was adopted (this study is analyzing data that was collected from another study—the OPTI-SCRIPT study, a RCT to reduce potentially inappropriate prescribing) | Explore patients' beliefs and attitudes towards medications and factors that influence medication beliefs | ≥ 5 medications daily | Multiple/Nonspecific Polypharmacy (≥ 1 med required. 82.6% polypharmacy in questionnaire recipients (range 3–23); 100% polypharmacy for interview recipients) | Patients' beliefs about medications based on a 5-point Likert scale questionnaire, factors that influence beliefs based on semi-structured interviews | Community dwelling patients aged ≥ 70 with pre-existing potentially inappropriate prescribing. The participants were from the OPTI-SCRIPT study | Questionnaire N = 196 (91 F, mean age 76.7, range 70–94) Interviews N = 11 (5 F, mean age 77, SD 3.9) | Participants completed the "Beliefs about Medicines Questionnaire"—a 5 point Likert scale questionnaire. Semi-structured qualitative interviews were conducted with a sample of XX participants | Older adult perceptions based on the questionnaire: 96.3% believed in the necessity of their medications to maintain health, 33.9% reported concerns regarding potential adverse effects of their medications, the difference between the necessity and concern scores was positive in 94% of participants—indicating strong beliefs that the benefits of medications outweigh the risks. Only 2.7% indicated a high belief medications were generally harmful, and 5.4% found medications to be generally overused. (to be considered in any of these percentages their Likert score had to be greater than the scale midpoint (it was a 5 point scale). When categorized by belief group 63.4% were accepting and 32.6% were ambivalent towards their medication (see additional notes). Results demonstrated that an increase in the number of repeat medications was significantly associated with an increased score on the necessity subscale. Perceptions based on interviews of participants (11 people): 6 were categorized as accepting on the subscale, 3 were ambivalent, and 2 had insufficient data to calculate their subscale. 3 themes emerged from these interviews: necessity and concern conflict, knowledge of medications (variable among participants), and relationships with healthcare providers (majority report a positive relationship) |
Weir, Kristie | 2018 | Australia | Qualitative study Semi-structured interviews—with older adults and companions | Explore the reasons behind variations in patient preferences, attitudes, and experiences towards polypharmacy and deprescribing. Identify key factors in decision-making about polypharmacy to be considered by physicians and patients | "Multiple medicines" | Multiple/Nonspecific Polypharmacy (most had ≥ 5 medications) | Participants' preferences in relation to decision-making about medications, and why they hold the preference they do | Older adults (aged ≥ 75) taking multiple medicines, they were encouraged to have their companion present if that reflected their usual situation. Companions were professional carers, partners, son/daughters, or relatives. (Interview questions were addressed to both participants) | Older Adults: N = 30 Age 75- ≥ 85, mean age 83 19 F 28 took ≥ 5 medications daily Demographics not provided for companions | Participants (and their companion if applicable) were asked how they liked to make decisions about their medications—5 statements were read to them and each indicated which statement best described their involvement preference. The reasoning behind their preference was then explored with open ended questions | 3 key themes emerged from the interviews: 1. attitudes towards medicines, openness to deprescribing, and decision-making preferences. Participants varied in their relation to these themes, resulting in them being categorized into 3 participants types (not always exclusively, some participants had traits in more than one participant type). Participants: Type 1—attached to medications (10 participants) —medications are perceived as highly important, participants were accepting of polypharmacy, and displayed a generally negative attitude towards deprescribing. A focus on benefits over harms of medications, which appeared related to decision-making preferences. Overall type 1 have high trust in their doctor's to make decisions, or strongly guide them. Self reported QOL as good or above. Type 2—would consider deprescribing (14 participants) —had ambivalence towards medications and discussed both the positive and negative aspects of medication. Although attitudes were still generally positive towards medications Type 2 may be more open to deprescribing. This group uniquely gathered information about their medications proactively and about half knew the reason (symptom relief versus illness prevention), which wasn't shown in Type 1 or 3. Self-rated health higher than the other groups, and QOL from fair to excellent. Type 3—(6 participants)—did not have strong opinions regarding their medications, were open to deprescribing, but prefer the doctor to make those decisions about their medications. Overall had a more limited knowledge about their medications. Self-rated health as fair or poor, and QOL as good or above. Companions: Of Type 1 s—companions were engaged in Type 1 participants medical care and daily living to varying degrees, held positive attitudes towards medications with some expressing that medication usage is a responsible act of reasonable older adults. Of Type 2 s—companions were involved in medical care, had a collaborative approach, supported their caree to be independent, and were aware of their carees' medications. Leaned towards a more negative attitude of medications if their caree had ambivalence towards the same. Of Type 3 s—had a large role in medication management, and management of other everyday life, some participants' companions were the only one who knew what the participant was taking and why—not the participant themselves. They perceived medications as an important aspect of every day life generally, and seemed to prefer a more hands off approach in medication decision-making |
Krska, Janet | 2013 | England | Qualitative study Face-to-face semi-structured interviews | To determine what medication-related challenges patients who take long-term medications consider to affect their everyday life, including QOL | Multiple medicines—study range 4 to 17, avg 7.8 per patient | Multiple/Nonspecific Polypharmacy (most had ≥ 5 medications) | Issues related to long-term multiple medication use | Community dwelling adults prescribed ≥ 4 regular medications for at least 1 year, who were ≥ 18 years of age (age in this study ranged from ~ 20 to over 80) | N = 21 10 F Age range “Approx 20 to > 80” Range 4–17, avg 7.8 medications per patient 163 medications | Participants were asked a series of open ended questions: Can you tell me about or show me your medicines? How do you use your medicines? How important do you feel your medicines are to you? Is there anything you don't like about your medicines? Do you feel you know enough about your medicines? how do you actually get your medicines? How do your medicines fit in with your life? How you know if your medicines are OK for you? Do you have any worries about your medicines? Would you change anything about your Medicines if you could? | 8 themes emerged from the interviews: relationships with health professionals, practicalities, information, efficacy, side effects, attitudes, impact, and control. (results relevant to polypharmacy/deprescribing highlighted). Attitudes towards medications: 6 patients felt medications were necessary to relieve symptoms or prolong life while simultaneously wishing they did not need medications, 7 patients had negative attitudes towards taking medications, 3 patients expressed concern about long-term medication use both in terms of dependency and the need to accept theoretical long-term benefits of prophylaxis against future problems. Impact of medications on everyday life: 6 patients described disruptive effects of medications on everyday activities like meal times, sleeping, and sex life. Control: 2 patients considered their lives to be controlled by medications |
Schiøtz, Michaela | 2018 | Denmark | A survey study | Determine patients' attitudes towards their medications and potential deprescribing | "Excessive or severe polypharmacy (ie ≥ 10 medicine)" | Multiple/Nonspecific Polypharmacy (≥ 10 medications) | Patients' beliefs and attitudes towards their medications and deprescribing. Their interest in attending an appointment dedicated to a discussion around their medications and polypharmacy | Outpatient adults aged ≥ 65 with 10 or more prescribed medications. Those included were Danish speaking | N = 100 Med age 75, range 65–92 63 F med 12 medications, range 10–32 | Participants completed the PATD questionnaire translated to the Danish language. Question 9 (assess the impact of medication costs) was modified to make it applicable with respect to the Danish Healthcare system. Revised to "the cost of medications impacts my willingness to stop one or more of them." They included demographic items on the questionnaire (age, gender, educational level), self-rated health (one item), and health literacy (four items from The Australian Health Literacy Questionnaire), (all translated into Danish) participants were also asked if they were interested in being contacted for an outpatient appointment with a focus on their medications | 81% of patients felt they were taking a large number of medications. 65% reported feeling confident about taking the amount of medications they did, 79% believed their medications were necessary. When responding to visual cues (pictures showing X amount of tablets/capsules) 62% of patients reported they were comfortable with a daily maximum intake of 8 tablets or capsules. 85% reported they would be willing to stop one or more of their medications if their doctor told them they could do so. 11% felt they were taking at least one regular medication that they no longer needed. 71% reported it would be acceptable to take even more medications than they did presently for their conditions, 40% believed that one or more of their medications were causing side effects. 85% reported they had a good understanding of the indications of their medications, 18% reported that the cost of medications influenced their willingness to deprescribe. 42% had experience with stopping one of their medications with 38% of those reported they did not need the discontinued medication and 60% reporting they had to restart the medication or start a new one. 67% reported they would prefer personal contact, with 48% also wanting written information with regards to follow-up if a medication was deprescribed. 19% reported they would prefer a phone call follow-up, and 8% indicated they would prefer no follow-up. 41% reported interest in a consultation in an outpatient setting focusing on polypharmacy, 42% were not interested, 15% were unsure, and 2% did not respond. There was no association between the participants' attitudes towards medications and deprescribing and their self-reported health, of between their attitudes and health literacy |
Linsky, Amy | 2015 | United States | Qualitative study: Using focus groups and in-depth interviews | Identify key patient elements that contribute to shared decision-making about deprescribing | 5 or more medications | Multiple/Nonspecific Polypharmacy (≥ 5 medications) | Patients' experiences with and attitudes towards taking multiple medications, their preferences towards reducing their number of medications, communication with their providers surrounding medications, and actual/hypothetical response to the suggestion by their provider of stopping a medication | Veterans taking 5 or more medications who had visited primary care at 1 of 2 Veterans Affairs Medical Centers (VAMC) at least twice in the previous 2 years | N = 27 participants. One focus group with 3 veterans, one focus group with 4 veterans, interviews with 20 additional veterans | The focus groups were moderated by 1 or 2 interviewers, a flexible interviewer's guide was used to query patients' experiences and attitudes, unanticipated topics raised by patients were followed up on | 3 main themes emerged: 1. conflicting views of medications 2. importance of patient-provider relationship 3. limited experience with medication discontinuation. The majority of the veterans expressed an overall desire to take fewer medications while simultaneously wishing to avoid negative consequences of such. Many of the veterans reported good adherence to their medications stating they were necessary for their health. Patient-provider relationships exerted a large influence on veterans perceptions and attitudes towards medications and adherence—the quality of the relationship influenced whether or not they trusted a particular clinician's suggestions. Some expressed how their lack of expertise on the matter results in them following the doctor's orders, preferring to let the clinician make the decisions, even if they had a general preference to take fewer medications. Some expressed the desire for shared decision-making—at minimum they wanted to be informed about the decision to deprescribe. Some veterans described the complexity of balancing differing recommendations from different providers with some expressing willingness to have a provider discontinue a medication that was originally prescribed by another provider. (this point may be more specific to the VAMC where it appears the doctors work more closely together than some other practices which may have lead to higher incidence of this comfort). Few participants could directly call a specific incidence of a medication being stopped, but when reviewing their electronic medical records several had discrepancies between what they were taking and what was in their records. Some had been told to stop a medication without that being documented in their records. As well, when asked if there were medications they had taken in the past and were no longer on many replied affirmatively |
Sirois, Caroline | 2016 | Quebec, Canada | A survey study | Describe community-dwelling older adult's attitudes and perceptions towards deprescribing | Not explicitly defined, inferred as such: "two thirds of Canadians 65 years and over used at least 5 unique prescription medications, and nearly a third used more than 10" | Multiple/Nonspecific Polypharmacy* (m 6 medications, range 3–8) | Patients' attitudes towards their medications and deprescribing (results section gives percentage answers to each question asked) | Community-dwelling adults aged 65 or older taking at least one medication | N = 129 81 F Med age 76, range 71–80 | A survey was created, adapted from the PATD questionnaire where participants rated their agreement on a 5-point Likert-type scale for 10 questions and answered 5 multiple choice questions about polypharmacy and deprescribing | 51% of participants felt they were taking a large number of medications, 81% felt comfortable with the number of medications they were taking, 84% believed all of their medications were necessary, 72% would be willing to stop one or more of their medications if their doctor said it was possible, 50% would like to reduce the number of medications they were taking, 22% felt they were taking a medication they no longer needed, 80% would accept taking more medications for their health conditions, 91% stated they have a good understanding of the reasons they were prescribed each of their medications, 33% agreed that having to pay for fewer medications would play a role in their willingness to stop one or more of their medications, and 25% believed one or more of their medications were giving them side effects. 60.5% answered "no" to having ever tried to stop a regular medication, only 66% (81) answered the question asking how many different tablets or capsules per day would you consider to be a lot (and no consensus emerged on how many was considered a lot—median response was 5 but responses varied widely), 51.2% reported they would be comfortable with a pharmacist being involved in stopping one or more of their medications and providing the follow-up, and 42.6% reported they would comfortable if a nurse was involved in the same. If a medication was stopped, in regards to follow-up 74.4% would like a face-to-face appointment, 12.4% would like a telephone call, 2.3% would like written information sent in the mail, 3.9% would like written information sent my email, and 7.0% would like no planned follow-up needed. 1.6% reported "other" for the follow-up they would like. The desire to reduce medications was strongly associated with the belief that individuals were taking a large number of medications, used medications that they felt were no longer needed, or had side effects from their medications. Oppositely, individuals that were comfortable with the number of medications they take or believe all their medications were necessary was negatively correlated with the desire to reduce the number of medications. There was no correlation between age and desire to reduce medication usage |
Linsky, Amy | 2019 | United States | National mail survey of Veterans receiving Veterans Affairs primary care | Characterize patients' willingness to accept deprescribing of their medications by different providers, as might occur in the context of hierarchy of professional authority | 5 or more medications | Multiple/Nonspecific Polypharmacy (≥ 5 medications) | Primary outcome: A measure of relative deprescribing authority (RDA)—defined as the extent to which patients afforded different providers the authority to discontinue a medication prescribed by another provider | Patients with 5 or more concurrent prescriptions in a 90 day period in the medical record, at least 1 primary care visit during that same time frame, and at least 1 additional visit in the prior year. respondents were older and took slightly fewer medications than nonrespondents but similar in race and region of the country, 85% of respondents were men. 60% were older than 65. 6% reported taking fewer than 5 medications | N = 803 735 answered both questions used to create the RDA outcome measure age range: ≤ 55 to ≥ 76 mean age 65.5 120 Female | Participants completed the "Patient Perceptions of Discontinuation (PPoD)" survey—43 medication discontinuation-related items, 8 attitudinal scales and 14 patient characteristics and background items | Attitudes toawards medications and their providers were generally favourable with a score of 3.75 on Provider knowledge and 3.56 on Trust-provider. Respondents generally disagreed that medications were either unimportant or overused, with a mean score of 2.39 and 2.91 on each respectively (based on a scale of 1–5 with 1 equalling strongly disagree and 5 equalling strongly agree). Respondents were generally interested in stopping medicines with a score of 3.42. RDA outcome measure: 38% were uncomfortable with both a PCP or clinical pharmacist stopping a specialist-prescribed medication, 20% reported they would be comfortable with both a PCP or clinical pharmacist stopping a specialist-prescribed medication, 21% reported no the PCP stopping the special-prescribed medication and yes to the clinical pharmacist doing the same, and 21% reported yes to the PCP's authority but no to the clinical pharmacist's. When setting the group who responded no to both the pharmacist and the PCP stopping a specialist-prescribed medication as the reference several factors influenced the liklihood of being in 1 of the 3 other RDA groups (Pharmacist no/PCP yes, pharmacist yes/PCP no, and both yes). Those with chronic lung disease were less likely to be in PCP yes/pharmacist no group, those with higher trust in their PCP were less likely to be in the PCP no/pharmacist yes group but more likely to be in the pharmacist no/PCP yes group. Patients with greater concerns about their medications were more likely to be in the both yes group, and veterans interested in being involved in shared decision making were more likely to respond PCP no/pharmacist yes |
Moen, Janne | 2008 | Sweden | Focus group | To conduct an exploratory study describing multiple medicine use from the elderly paient's perspective | 5 or more medications | Multiple/Nonspecific Polypharmacy* (m 7 medications, range 3–15) | Identify perceptions about the use of multiple medicines through discussion | 65 years or older, currently using five or more medicines (including prescription and OTC, daily or as needed for chronic conditions), willing and able to comply with and understand study requiement, sufficient hearing for group discussion, and Swedish-speaking | N = 59 (mean age 76, 50.8% female) | Conventional content analysis approach using semi-structuered focus group was used. One moderator. 12 focus groups (1–1.5 h) were done during Nov and Dec 2006. Conducted until saturation was reached on rsearch questions. Same-sex focus groups were done (i.e., 6 male, 6 female) to provide a secure environment to discuss sensitive drugs/diseases. NVivo 1.2 software | Three themes: 1. Belief about medicines (attitude to medicines, definition of multiple medicine use, benefit from medicine, adverse effects and interactions), 2. Thoughts and unanswered questions (taking responsibility, adherence), 3. Relaionship to doctor (trust and distrust, access) |
Leydon, Geraldine | 2007 | England | Qualitative study Face-to-face semi-structured interviews | Examine patient perspetives of discontinuing SSRIs | N/A | SSRIs | Themes and commonalities among patients who have been taking SSRIs for a long period and what may be influencing their decisions to stay on or go off these medications | Participants recruited from a group practice in Southampton. Patients had been taking SSRIs for a minimum of 1 year, with an average of 4 years, and were diverse in their history of depression (i.e., number of depressive episodes). Recruited participants had to have been deemed "well enough" by the practicioner to be able to participate | N = 17(10 female, ages 28 to 64) | Thematic analysis of participant stories and experiences regarding SSRI use. A "topic guide" was used to make sure all relevant topics were touched on in the interview | Three main themes identified: (1) Uncertainty about benefits of and need to continue SSRIs—how much improvement to expect, sources of improvement (i.e., whether it was the SSRI or outside influence), whether they had improved at all (2) Barriers to discontinuation—patients were discouraged to discontinue SSRIs out of fears and/or experience of relapse of depressive and withdrawal symptoms. Previous experience with withdrawal/depressive symptoms (by patients who had gone off medication by themselves) represent a strong discouragement. Patients who had not previously experienced withdrawal are more receptive to discontinuation, provided they go off gradually (3) Importance of GP's role—Lack of communication with GP may lead to perceived sense of lack of opportunities to go off medication. Some patients find it difficult to reach out and have these discussions with their GP. A strong degree of involvement by the GP was associated with feeling more comfortable trying to discontinue SSRIs. GPs should initiate discussions about discontinuing, and not rely on patients to do so |
Martin, Phillipe | 2017 | Quebec, Canada | Mixed methods study utilizing a pragmatic randomized intervention | Test whether the EMPOWER trial increased motivation to deprescribe, increased knowledge about benzodiazepines, improved self-efficacy, and increased opportunities to reach out to healthcare providers to taper/deprescribe | N/A | Benzodiazepines | Quantiative data: Preintervention and 1-week-postintervention. Includes BMQ-Specific (assesses beliefs about necessity + concerns about benzodiazepines—5 point likert scale); single Risk perception question (Do participants perceive same, more, or less risk of benzodiazepines following intervention); Medication Reduction self-efficacy scale (rates 0 to 100 confidence in tapering medication) Qualitative data: Semistructured interviews in participants' homes; | Older chronic benzodiazepine users recruited from Montreal area pharmacies | N = 303 (recruited) N = 261 with eligible follow-up data for quantitative analysis (mean age 74.6, 72% female) | EMPOWER brochure mailed out to participants, providing self-asssessment and information about benzodiazepine risk in older users, as well as information about self-directed medication tapering | 64% (or n = 127) of participants experienced increased motivation to deprescribe, with improved knowledge, lower perceived necessity, increased concern, and increased perception of risk about benzodiazepines. The EMPOWER intervention improved capacity for tapering in individuals who decided to deprescribe. ~ 50% of individuals who had their motivation improved talked to a physician about deprescribing, and 25% talked to their pharmacist. This aligns with theory that states that increased knowledge gives patients more motivation + self-efficacy to initiate conversations about deprescribing with their healthcare providers Motivation is not 100% stable: internal (concerns about health, goals, fears of symptom recurrence, psychological dependancy) and external (lack of support from healthcare provider) are highly influential on decisions to deprescribe The strategies behind EMPOWER/the intervention itself are necessary but not sufficient for triggering change in capacity to deprescribe, and additional strategies/improved support + knowledge about risks of benzodiazepines from healthcare providers are key to keep patients engaged in the deprescribing process |
Horner, E | 2009 | United Kingdom | Quantitative, cross-sectional questionnaire | Understand women's knowledge of risks of long-term HRT, understand effect of increased public knowledge about risks of HRT, and explore patients' attitudes towards discontinuing HRT | N/A—Focuses on hormone replacement therapy | Hormone Replacement Therapy, incl Estrogen implants Testosterone implants Estradiol Progestogen | Estradiol + testosterone levels at time of questionnaire Knowledge of risks and attitudes towards HRT/discontinuing treatment were evaluated | Postmenopausal women receiving long-term estrogen + testosterone implants (hormone replacement therapy; HRT) without a history of side effects | N = 100 (100 F, median age 64.5 years); women were an average of 46.5 years of age when they began HRT, and had been on HRT for an average of 17.65 years Health conditions present: Total abdominal hysterectomy + bilatearl salpingooophorectomy (n = 69) Total abdominal hysteroectomy w/out BSO (n = 12) Ovaries + uterus intact (n = 19) | 10-question questionnaire: Have you been informed of the effects of estrogens regarding WHI/MWS? Do you accept that there is probably a small excess risk of breast cancer? Do you think this risk is dose-dependent? Do you think this risk s duration-dependent? Would you be happy to discontinue HRT? Do you have symptoms returning as the implant wears off? Would you be happy to try a lower dose? Would you be happy to switch to another route of administration of hormones? | Have you been informed of the effects of estrogens regarding WHI/MWS? (100% YES, 0% NO, 0% UNSURE) Do you accept that there is probably a small excess risk of breast cancer? (76% YES, 8% NO, 16% UNSURE) Do you think this risk is dose-dependent? (22% YES, 26% NO, 52% UNSURE) Do you think this risk is duration-dependent? (20% YES, 37% NO, 43% UNSURE) Would you be happy to discontinue HRT? (3% YES, 97% NO) Do you have symptoms returning as the implant wears off? (96% YES, 4% NO) Would you be happy to try a lower dose? (26% YES, 38% NO, 36% YES) Would you be happy to switch to another route of administration of hormones? (14% YES, 83% NO, 3% UNSURE) Summary: Women acknowledge risks, downplay effects of media/increased knowledge; this sample overwhelmingly wants to remain on treatment because they do not want to return to negative quality of life pre-HRT |
Reeve, Emily | 2019 | Australia | Quantitative, cross-sectional questionnaire | Assess attitudes and beliefs towards deprescribing and specific characteristics in line with these | N/A—Looked at ≥ 1 prescription medications | Multiple/Nonspecific *Non-Polypharmacy specific (≥ 1 med required) | Attitudess towards deprescribing in both caregivers and older adults using polypharmacy Specific characteristics associated with being open or not open to deprescribing | Older adults (65 +) taking at least one regular prescription medication and who could complete a written quesitonnaire in English Caregivers (NOT paired w/ the older adults; 18 +) who played a role in family/friend's health/medication plan in a informal/unpaid manner | Older adults: N = 386 (median age 74, 43% male) Caregivers: N = 205 (median age 67, 75% female) Polypharmacy: Between 47.1% (self-managed) and 54.6% (care recipient) of participants took than 5 medications | Participants completed the Revised Patients’ Attitudes Towards Deprescribing (rPATD questionnaire. The questionnaire utilizes a 5-point likert scale (strongly agree to strongly disagree); however, the question "I would be willing to stop one or more of my medicines if my doctor said it was possible" was converted to a binary (yes or no) option, pooling all disagree options and 'unsure' into the 'no' option for the purpose of one analysis In addition: Wake Forest Trust in Physician Scale Patient Autonomy Index Beliefs about Medicines Questionnaire (BMAQ) Demographic participant variables and ‘self perceived health’ Hard copy or online, split fairly evenly | 88% of surveyed older adults and 84% of caregivers would be willing to stop a medication if doctor said it was possible Lower concerns about stopping are correlated with oppeness to deprescribe—strongest predictor in older adults (if below median, 8 × more likely, (G = − 0.216; p = 0.003) Caregivers are more likely to be open to deprescribe if patient health is good—strongest predictor in caregivers (; in contrast to healthcare professionals, where previous research has found GPs/etc. do not want to deprescribe if the person is doing well No relationship found between trust in physician/healthcare practicioner and willingness to deprescribe (surprising) |
Hopper, Ingrid | 2016 | Australia | Quantitative, cross-sectional survey | Examine heart failure (HF) patient and practicioner attitudes about polypharmacy and medication withdrawal/cessation | "here defined as the use of 5 or more prescription medications" | Heart Failure (HF) medications, including but not limited to: Beta-blockers Aspirin Statin Spironolactone ACE inhibitors | Satisfaction about medication + attitudes towards stopping/cessating medication For practicioners, attitudes about medications and comfort levels for withdrawing medication in hypothetical scenarios | Patients with heart failure (HF), taking 5 or more medication for HF Prescribing clinicians | Patients: N = 85 (73% or 62 M, mean age 61 (range 49 to 73) average of 8.4 total medications (5.4 specifically cardiac)) Practicioners (N = 74; n = 51 cardiologists, n = 14 nurse practicioners, n = 9 GPs; further demographics not reported for this group) | Survey assessing attitudes towards medication for patients For practicioners, survey presenting different hypothetical scenarios of withdrawing medications and asking them to rate their comfort level doing so | Patients Number of medication satisfaction: 52% of patients were satisfied, 32% neutral, 15% unsatisfied or very unsatisfied with number of medication they were on 59% of participants said there was not a medication they would stop if they could 41% who said yes, common answers included: frusemide, warfarin, ACE inhibitors, beta blockers, potassium supplements, statins Practicioners On a 5-point likert scale, Practicioners were most comfortable hypothetically withdrawing digoxin (4.01), statin in idiopathic HF patients (3.93), aspirin in idiopathic HF patients (3.74), and spironolactone in patients with normal ejection fraction (EF; 3.47) Practicioners were least comfortable ceasing statin (1.73) and aspirin (1.85) in patients in ischemic HF; also uncomfrtable ceasing ACE inhibitors and beta blockers (2.15, 2.45) in patients who were recovering to normal EF Summary: Sheer number, or polypharmacy itself, and cost of medications were least important issues. Treatment of HF symptoms (both groups) and kidney symptoms (patients) were most important |
Iliffe, Steven | 2003 | United Kingdom | Qualitative study Face-to-face semi-structured interviews (patients) and non-standardized conversational interviews (practicioners) | Assess beliefs and attitudes of older patients and practicioners on stopping/continuing benzodiazepine hypnotic use | N/A | Benzodiazepine hypnotics | Beliefs and attitudes of older patients and practicioners on stopping or continuing benzodiazepine hypnotic use | Older (65 +) Benzodiazepine hypnotic users from inner-city, suburban, and rural London/London area. Patients were required to take benzodiazepine hypnotics for at least six months on a daily basis. Patients w/ dementia, cognitive disability, terminal care, seizures, severe psychiatric disorders, epilepsy, severe deafness/blindness, or where discontinuation of the hypnotics was "clinically inappropriate" as deemed by the GP | Patients: N = 192; (mean 77 yrs, 65–93 yrs; 72% female) | Patients Semi-structured interview covering the following topics: Type, dose, length, frequency of benzodiazepine hypnotic use Initial and current reasons for prescription Belief in efficacy of medication Concern about effects of long-term use Any attempt to stop previously Perceived advantages and disadvantages of stopping use Following interview, patients were invited to participate in a withdrawal program—attitudes were then broken up by group ("continuers" vs "withdrawers") Practicioners Review practicioners' concepts of benzodiazepine hypnotic use, incl. advantages and disadvantages of discontinuing benzodiazepine use with their older patients, and any issues they may raise on their own that the researchers had not considered | Patients 109 withdrawers, 83 continuers (56.77% of participants chose to withdraw) No group effect of age, gender, or dosage (continuers vs withdrawers) Only 4–5% of patients (either group) found the medication "not at all helpful"; overwhelming majority felt medication was helpful Withdrawers were more likely to experience sleeping problems in spite of medication over continuers (28% vs 15% of "very often" or "nearly always") 65% of continuers and 68% of withdrawers had never been told their benzodiazepine use may be harmful of those that did know for risks, 17% in each group heard the info about risks from a GP, while 11%(W) and 9%(C) learned "from their own research" Most (74% of W, 86% of C)had not worried about harmful side effects, but withdrawers were significantly more likely to worry nonetheless 67% of W, 61% of C worried about insomnia following potential withdrawal Withdrawers were able to cite clear advantages of withdrawing—i.e., better memory, clearer thinking; continuers could not (difference was significant) Practicioners 48% were concerned about increased demand on the GP 51% anticipated difficulty in convincing their older patients to withdraw, citing concerns such as insomnia, anxious or upset patients, and unmasked depression Benefits cited included fewer falls (57% of respondents); better sleep (25%), increased quality of life (18%), reduced depression/increased independence (9%) 65% of practicioners felt their practice would benefit because deprescribing is "best practice"; 34% felt it would be beneficial to operating costs 22% believe reducing benzodiazepine use amongst older patients is a "public health issue" |
Reeve, Emily | 2016 | Australia | Qualitative study—Focus group | Assess attitude and beliefs of older adults and caregivers towards deprescribing | N/A—Focuses on inappropriate medication use; most participants use 3 or more prescribed medications | Multiple/Nonspecific *Non-Polypharmacy specific (≥ 1 med required) | Direct content analysis (DCA) and conventional content analysis (CCA) to establish themes around deprescribing. A previous DCA framework utilizing 5 main themes (appropriateness, process, influence, dislike, fear) was used to guide the DCA. CCA was used to create themes where text did not fit one of the aforementioned 5 themes | Older Australian adults and (non-paid) carers, either living or caring for someone living in community or in a "retirement village" | N = 28 n = 8 community carers (5 F; focus group 1; mean age 70.3; avg of 7.0 medications) n = 6 care facility carers (6 F; group 4, mean age 79, 3.4 meds) n = 11 community older adults (4 F; group 2, m 79.4, 3.4 meds) n = 3 retirement village adults (2 F; group 3, m 79, 3.4 meds) | Analysis of themes in focus group interviews and establishment of themes/barriers/enabler to deprescribing | Themes that emerged: Why? What is the benefit of withdrawing and what impact does it have on quality of life? Benefits (barrier to stopping)—if it's successful, why stop? Acceptance (barrier)—or, medication as a necessity Long-term use (barrier)—if patients have been using it for so long, it should remain/is appropriate Lack of current harm (barrier)—lack of current side effects Lack of benefit (enabler)—the condition is resolved or goals have changed, so the medication is no longer perceived as necessary Alternative available (enabler)—a better medication or lifestyle change may be a different option Drug interactions (enabler)—concerns about medication interaction Side effects (enabler)—***often the first theme brought up as an enabler to withdrawal Discussion—discussions with the practicioner should include "why" and "what to expect" Monitoring and follow-up—patients want to know what is required; carers feel they are in a good position to achieve this Trial basis—more willing to deprescribe if it is on a trial basis Other—medications should be weaned off, not just cessated; they should be weaned off one by one; lack of liasion/communication/oversight between healthcare practicioners is a concern; there may be a reversal of drug interactions Healthcare professionals—GPs may use personal examples to influence patients who don't want to be on a medication to stay on; GPs may just provide repeats continually, suggesting it is still appropriate to patients. ‘Overwhelmingly’, if the GP suggested withdrawal the adult/caregiver would agree due to trust and the GP’s knowledge Family and friends—these opinions are valuable, though this perspective was mixed amongst the participants Previous negative withdrawal experience—makes cessating that specific medication more difficult Other—age, number of medications, media, family history, "regulatory influences", expectations of how a medication should go Fear (barrier)—fear of returning symptoms, non-specific fear, fear of withdrawal reactions Dislike of medication (enabler)—many believe that medication can be replaced by lifestyle changes Cost (enabler)—cost of medications can be a motivator to reduce, but is rarely a sole motivator Inconvenience—to self and care recipient Implications for practice:—GPs are the main driver of withdrawal, and should not be discouraged by patient resistance The process between the healthcare professional and the patient needs to be detailed, and emphasize the why and expectations When resistance to deprescribing is presence, practicioners must engage in shared decision-making and engage in discussion to find the sources behind resistance |
Ng, Wei Ling | 2017 | Singapore | Quantitative, cross-sectional survey | Determine amount of Singaporean patients open to deprescribing in a sample, and to assess their attitudes/beliefs about deprescribing, especially as the ambulatory setting/health care system of Singapore lends itself to high levels of polypharmacy/inappropriate prescription | "5 or more prescribed medications" | Multiple/Nonspecific Polypharmacy (≥ 5 medications) | Sociodemographic information and attitudes towards deprescribing | Patients between 45 and 84 receiving treatment for more than one chronic disease; excluded any patients who did not understand English or had clinical diagnosis of dementia/cognitive impairment | N = 137 (45–84; median age 68; 41.2% or 57 F); majority Chinese (69.9%), Malay (8.8%), Indian (15.4%); median of 4 medical conditions an 6 medications | Demographic data PATD Wake Forest Physician Trust Scale | 93.4% of all patients, or 91.6% of elderly (≥ 65 yrs) would be willing to stop a medication if advised to by their doctor. 72.8% would like to reduce the number they were taking 82.4% of participants were comfortable with amount of medication, and 88.88% believed their medications were necessary 25% felt they were taking a medication(s) that was no longer necessary. 30% cited one or more of their medications was giving them side effects Willigness to stop a medication was most strongly associated with desire to take fewer medications. Patients are willing to stop a medication even if they are OK with the number and believed all their medications were necessary Sheer number of medications did not make participants uncomfortable Experience of side effects was more strongly associated with the belief that all medications were not necessary, but not with willignness or desire to stop Younger age (< 65) positively associated with willigness to deprescribe Trust in physician positively associated with willigness to deprescribe Medication discount card (or, considered more broadly, cost) became non-significantly associated with willigness to deprescribe if more factors were considered |
Kovačević, Sandra | 2017 | Serbia | Qualitative questionnaire and consultation with practicioner | Examine elderly polypharmacy patients' concerns and needs regarding their medication using the Structured Patient-Pharmacist Consultation (SPCC) framework | Polypharmacy as ≥ 5 medications | Multiple/Nonspecific Polypharmacy (≥ 5 medications) Stated interest in: Cardiovascular Alimentary Musculoskeletal Respiratory Medications | Participants completed a "MyChecklist" examining knowledge, expectations, problems, concerns and reasons to stop treatment (open-ended questions); and then a consultation to learn more about medication and express their concerns | 65 + , using 5 or more medications for medical conditions present for at least 6 months. Translations were provided for participants who did not speak the local language Exclusion criteria: Physically frai (as assessed by doctor)l/Alzheimers/cannot leave their homes/cognitive disability | Pharmacists N = 44 Participants N = 440 (mean age 73 + − 6.3, 54.1% or 238 F) | Open-ended "MyCheckList" questionnaire to assess knowledge, problems, expectations, reasons to stop treatment, and concerns Structured Patient-Pharmacist Consultation (SPPC) with their pharmacist—this framework examines patient involvement, concerns, and attitudes with regards to their medications | More than 50% of participants raised questions to discuss with their pharmacist. (approximately 250?) 54 participants asked if they should take drugs consistently or as needed; and appropriate times/dosages 12 were concerned they were on too many drugs 26 expressed concerns about interactions 23 wondered about duration 5.2% wondered why they were on certain medications Majority were satisfied with medications—53.4% and 23.4% say expectations have been absolutely or partially met, respectively 40%, or 117, participants reported problems—regimen/administration issues (forgetting instructions, not splitting drugs) 30.7% concerned about side effects ”Almost half” expressed concerns about therapy, including side effects, polypharmacy complexity/fear of number of drugs Addiction concerns raised by 6.8%; 6.1% were concerend about lifelong treatment; 4.5% felt drugs were ineffective 27.7% had considered stopping treatment—most common sources included adverse reactions (7.5%) and cost (6.8%). Feeling in control of condition, administration difficulty, intereference with daily routine, are also concerns Summing up multiple concerns (Costs, addiction, long-term effects), 73.6% of participants report concerns 27.7% of participants demonstrated non-adherence, compared to estimate of 50% for most elderly polypharmacy patients Specific Drugs/Conditions: Atrial fibrilation associated with more expectations being met Anticoagulants and COPD increased risk of treatment discontinuation Benzodiazepines increased adverse reactions, risk of treatment discontinuation, and increased risk of referall to doctor because of non-adherence Beta agonists/corticosteroids associated with increased risk of referral to doctor Dyslipidemia and Long-acting nitrates associated with less concern about medications Long-acting nitrates and previous myocardial infarction associated with poorer understanding of medications post-consultation Diabetes associated with better understanding as well as lower rates of referral to doctor for non-adherence |
Turner, Justin | 2017 | Canada | Quantitative, cross-sectional survey | Examine older Canadian adults' perceptions of deprescribing and medication risks. Ascertain how patients seek out this information and what factors play a role in patient-initiated deprescribing conversations | Not stated—Not focused on | Multiple/Nonspecific *Non-Polypharmacy specific (surveyed across Canada regardless of medication use) | Demographics: age, sex, number of medications Questions about: Awareness of the term "deprescribing" Past history of INITIATING a conversation w/ a doctor about deprescribing Behaviours of seeking information about medication Knowledge of harmful effects of medications | English or French-speaking community-dwelling ≥ 65 men and women recruited from across Canada (randomized phone number recruitment from each province) | N = 2665 Mean age 74.9 + -7.2 (range 65–100) 66.3 (~ 1776) F 23.8% French 88.3% had consumed ≥ 1 prescription medication over the last 12 months* (41.6% had consumed a sedative-hypnotic*, glyburide, or PPI*) {* = females more likely to have done so} Oldr age pos. associated with sedative-hypnotic and neg. associated with PPI use | Survey utilizing "perceived severity" and "perceived susceptibility" frameworks from the Health Belief Model of behavior change | 65.2% of participants acknowledged some medications could be harmful 41.8% had initiated a conversation about deprescribing with a healthcare professional, of which women, individuals < 80, and those who were aware of medication harms were more likely to do so 6.9% were familiar with the term "desprescribing"—those who did were more likely to initiate that conversation French people were less likely to know about deprescribing and less likely to know about medication-related harms 48% of participants independently searched for information about medication—they were 4 × more likely to initiate deprescribing conversations. Most common source was Internet—individuals who looked on the internet specifically were 3 × more likely to initiate the conversation (important b/c past research lessened the impact of the internet in changing health behaviours) For those taking benzodiazepines, PPIs, and glyburide, ~ half considered dose reduction/substitution/cessation Overall, althoguh deprescribing is becoming more popular among academics, it is still very poorly known as a term amongst older adults |
Cook, Joan | 2007 | Pennsylvania, United States | Qualitative study Face-to-face semi-structured interviews | Understand causes behind chronic benzodiazepine use in older adults, explore intervention/cessation strategies | Not stated—Not focused on | Benzodiazepine anxiolytics | Thematic analysis of qualitative interviews | ≥ 60, currently taking a benzodiazepine anxiolytic for a min. 3 month period, score > 16 on the Short Blessed Test (cognitive funcitoning) Recruited from Philadelphia-area practices via their healthcare practicioner | N = 50 85% F 81% white, 19% Black M age 71.13, range 61–95, SD 7.73 (This also include a lot of info on marriage status/ income, let me know if you'd like me to include this—most studies don't, so I just kept it basic here) 14% had taken their benzodiazepines < 1 yr; 8% for over 20 years Anxiety and bereveament most common sources of benzodiazepine prescription | Qualitative guided interview | Thematic analysis revealed 3 themes: -Purpose and Importance of Benzodiazepines Many feel the drugs are a key part of their lives/routine But, less clear about details (i.e., can't recall the exact mg dose they take) Benzodiazepines represent a mean to cope with anxiety, sleep Life-transforming properties (can't function without / make patients feel 'like themselves') Lack of awareness/understimation/disregard for side effects (patients view the benzo's benefits as outweighing any risks, and often were not aware of any side effects—no input from doctor; minimizing the impact these effects could have; acknowledged side effects usually impacted mental acuity. Side effects were always 'worthwhile') Attitudes towards tapering/discontinuation negativity/resistance (fear of consequences, i.e. that they would suffer from a mental health standpoint) many were initially open to tapering/substituting, but further investigation revealed a lot of resistance—resistance to change, citing side effects/age, citing wanting to avoid mental suffering, etc.—once again, resistance to "rocking the boat" if it's working—lots of anxiety and fear—easy and routine to get refills—real or imagined discontinuation reactions are a deterrent—psychological over physical dependence emphasized—many feel they "could not go on", but didn’t particularly emphasize physical withdrawl effects —refusal of psychological interventions (lack of knowledge/too scared to try something new/don't think it would work on them) Power and influence in patient-physician relationship—complete faith in physician, will follow what the say—however, physicians often feel they don't have this power—they'll just prescribe benzodiazepines b/c they feel they have no alternative |
Linsky, Amy | 2018 | United States | Quantitative, cross-sectional survey | Identify characteristics that make patients more or less amenable to discontinuing/cessating medication | ≥ 5 medications | Multiple/Nonspecific Polypharmacy (≥ 5 medications) | Predictors and characteristics associated with being more/less open to deprescribing—multiple domains, including concerns, knowledge, importance of medicines | Via the U.S. Departments of Veterans Affairs (VA), Veterans taking ≥ 5 medications for 90 days who had visited a primary care within that 90 day frame and at least once in the preceding year | N = 803 15% or 121 F mean 67.0 yrs, mean number of medications 10.1 only 6% took < 5 medications 68% white, 17% Black 60% ≥ 65 y/o > 33% had a hospital admission in the past year | Patients Perceptions of Discontinuation (PPOD), which contains the scales: BMQ-Overuse (assesses overreliance on medications) Trust-Provider (assesses beliefs about if providers do what is best for patients) CollaboRATE (measures shared decision making) As well as the PPOD scales: Medication Concerns (assesses short and long-term effects of medications) Provider Knowledge (assesses medical knowledge of primacy care provider/PCP) Interest in Stopping Medicines (current level of interest in discontinuation) Patient involvement in Decision Making (assesses patients' interest in planning their medical care) Unimportance of Medicines (potential harms or low benefit of ≥ 1 their medications) These usually consist of 3–6 questions KEY question was: "Have you ever stopped taking a medication (with or without your doctor's knowledge)?" —Analyses restricted to those who said Yes or No, disregarded 'Unsure' | Participants Disagreed that medications were unimportant/overused Favourable views of providers (3.75/5 on Provider Knowledge, 3.56/5 on Trust-Provider) Generally interested In stopping medications (3.42/5) 53% of participants reported being told to stop a medicine by a provider, while 55% had asked a provider to be taken off a medication 34.1% reported having stopped a medication, with or without doctor's knowledge Model of Predictors of Medication Discontinuation: positive associations with discontinuing: provider recommendation (strongest), patient request (2nd strongest), higher education, greater interest in deprescribing, higher preference for shared decision making (last 3 not in order) negative associations with discontinuing: taking more medications, seeing a VA clinical pharmacist, greater trust in one's PCP Take homes: Patient-provider communication is key Many patients and physicians feel as though the control/power falls to the prescriber Patient-initiated conversations about deprescribing take away any uncertainty in the eyes of the physician and are a strong driver of discontinuing Pharmacists may feel they do not have the power to act on decisions re: medication changes Contrary Result: Participants taking multiple medications less likely to report discontinuation—this may be that those on less medications already have discontinued some, and those on a lot of medications may not have had the chance or opportunity to yet (speculative on behalf of the authors) |
Williams, B | 2005 | Scotland, England / United Kingdom | Focus group | Assess attitudes about medications and regimens amongst adults diagnosed with hypercholestrolaeima and hypertension, and assess oppeness to receiving a combined medication tablet/polypill | N/A | Prescriptions for hypercholesterolaeima and hypertension All patients were taking 6—20 pills/day | Attitudes towards medication consumption and polypill usage | UK individuals taking prescriptions for hypercholestrolaeima and hypertension between 45 and 72 | N = 92 (32 F), aged between 45 and 72. n = 69/92 (75%) ≥ 62 y/o | Framework' thematic analysis of focus group transcriptions | Most patients acknowledged medicines were necessary even though they may not like them Complexity is not a large issue—some patients may even make medication regimens more complex (splitting them up over the whole day) to make them easier to manage Complexity can be reduced with routine, but routines are subject to changes in patient's personal life; instability in prescription; confusion about drug appearances (colour, dosages, etc.); frequency or dosage changes; these can lead to non-adherence Patients alter dosages/regimens themselves Many patients were open to the concept of polypills initially, but then expressed doubt over whether a polypill could address all their needs. Overall, a majority suggested they would rather keep things the same than lose the potential effects of some of their medications if the polypill could not address all their medical needs Some patients would be willing to change regimens if their doctor suggested it |
Reeve, Emily | 2013 | Australia | Quantitative, cross-sectional survey | Investigate people's opinions about how many medications they take, and their attitudes towards deprescribing | N/A—Seemed to generally refer to multiple medications being taken, no specific number | Multiple/Nonspecific *Non-Polypharmacy specific (≥ 1 med required) | Demographics, medication info (number, dosages, conditions treated) Patient Attitudes Towards Deprescribing (PATD) questionnaire Geriatric Depression Scale Mini-Mental State Examination Morisky Medication Adherence Drug Burden Index Following study proper, participants were mailed: BMQ Wake Forest Physician Trust scale | Australians ≥ 18 years of older and taking one or more medication Note: Many conditions, medications for these conditions are chronic for this particular population (based on the type of clinic they recruited from) | N = 100 Age 20–91 (IQR 60–81, median age 71.5) Median 6 medical conditions Median 10 medications taken Medications, number of tablets per day, and conditions significantly increased with age Participants ≥ 65 y/o had median 7 medical conditions and took a median of 11 medications Most common conditions: Cardiovascular disease (86%) Diabetes mellitus (29%) Asthma/COPD (26%) | Demographics, medication info (number, dosages, conditions treated) Patient Attitudes Towards Deprescribing (PATD) questionnaire Geriatric Depression Scale Mini-Mental State Examination Morisky Medication Adherence Drug Burden Index Following study proper, participants were mailed: BMQ Wake Forest Physician Trust scale | 92% of patients would cease a medication if physician informed them it was possible (no effect of age—older adults [I believe defined as ≥ 60], 89%) 65% agreed they were taking "a large number of medications" 68% had a desire to reduce the number of medications they were taking 78% felt all their medications were necessary 16% felt they were taking a medication that was no longer necessary Willingness to stop positively associated with desire to take fewer medications, but no other factors from the PATD (i.e., feeling they have a large # of meds). Other factors: Higher physician trust positively associated w/ willigness to stop, medical discount card negatively associated w/ willigness to stop |
Jia Hao, Lim | 2018 | Malaysia | Quantitative, cross-sectional questionnaire | Examine attitudes about polypharmacy and deprescribing amongst elderly patients with chronic diseases | ≥ 5 medications daily | Multiple/Nonspecific Polypharmacy (≥ 5 medications) | Patient Attitudes Towards Deprescribing questionnaire (PATD) | Elderly ≥ 65 y/o, with at least one chronic disease and taking ≥ 5 medications daily | N = 222 128 F Median age 70 (IQR 67–73) | PATD | 60.4% were comrfortable with their # of medications daily 79.97% felt there medications were necessary 56.3% would like to reduce the # of medications 83.3% would stop one or more if their doctor informed them it was possible 12.2% felt they were taking a medication that was no longer necessary 81.1% felt they had a good understanding of the reasons they were on each medication 34.7% stated that paying for less medication would be a reason to stop 40.1% felt that one or more of their medications were giving side effects Age was negatively correlated with agreeing with the following: If my doctor said it was possible, I would be willing to stop 1 + of my medicaitons Would like to reduce the # of medications Good understanding of reasons why they are on medications Interestingly,Number of medications was positively correlated with: Belief in necessity Willigness to take more medications GOod understanding of the reasons behind prescription Negatively correlated with: Feeling of taking large number; desire to deprescribe; feeling they take no longer needed medications; perceptions of side effects Desire to stop 1 + medications was positively correlated with: feeling they take a large number of medications feeling of taking no-lonegr-needed medications having to pay for fewer medications belief of side effects negatively correlated with: willigness to take more; belief in necessity of medications Writers emphasize that trust must be created in medications Assessment regarding medications should be done towards those who are comforable iwth their current number, |
Straand, Jørund | 2001 | Norway | Quantitative, cross-sectional questionnaire | Measure how patients and physicians agree about deprescribing/factual information about when a drug was withdrawn | N/A | Multiple/Nonspecific *Non-Polypharmacy specific (≥ 1 med required) | Assess perceptions and knowledge of drug withdrawal amongst patients and their physicians | Norwegian GPs and a corresponding patient whom they had withdrew a medication from a drug regimen that had lasted ≥ 3 months | Physicians: N = 272 54 F Mean age 43, med. 42, range 28–68 Experience 13 years, med 12, range 1–40 Known corresponding patient for an average of 7 yrs, med 5, range 0–34 yrs Patients: N = 272 162 F Mean age 64, med 67, range 18–93 | Questionnaires for physicians: #1—Demographics and experience #2—Regarding a patient, what drug had been discontinued, who started/why was therapy started, info about patient, how drug withdrawal occurred (gradually or abruptly), and whether they felt the patient was satisfied Questionnaire for patients: If they knew what drug/why it was discontinued The nature of drug withdrawal If they had an appointment for follow-up Whether they felt satisfied | 100% concordance between patient and physician about what drug had been discontinued—High % (72%) were cardiovascular drugs; 32% were CNS drugs ('ATC main group N'); only 3.3% benzodiazepines 74% agreement for diagnostic indication/why the drug was prescribed 18% of cases, patient and physician disagreed about whether discontinaution was abrupt or gradual 9% disagreement about whether a new follow-up appointment had been scheduled Patients were more variable than doctors in perceptions of whether they were satisfied 73% of patients were satisfied or very satisfied vs 74% of GPs thinking they were very satisfied Some qualitative statements given by patients included the following themes, with an excerpt: Theme 1—What a Relief ("I am very satisfied because I was taking so many tablets every day. It is good to let go of this, also with regards to side effects.") Anxiety and skepticism— ("I am sceptical because the hospital doctor said I had to take Albyl E (acetylsalicylic acid) for the rest of my life.") Importance of good communication and follow-up ("But many doctors give too little information, and the patient becomes insecure") The doctor knows best (I have full confidence in my doctor, and I feel secure.) |
Luymes, Clare | 2017 | Netherlands | Q-methodology | Identify viewpoints in patients with low cardiovascular disease (CVD) risk regarding their (potentially unnecessary) medication, and examine how these relate to preferences for deprescribing from these unnecessary medications | N/A | Preventative CVD medication | Q-sort and group discussions | Patients from the Evaluating Cessation of STatins and Antihypertensive Treatment In primary Care (ECSTATIC) trial | Q-sort: N = 31 9 M 57.1 yrs + − 6.8 yrs Group discussions: N = 28 9 M 57.7 yrs + − 6.8 yrs | Q-methodology and group discussions amongst continuing and deprescription groups | Patients emphasized a GP with good communication skills/clear explanations All patients regarded hypertension management as the GP's responsibility 3 general viewpoints: afraid, controlling, autonomous Most patients with autonomous perspectives had their preventative medication deprescribed Some (n = 13) Patients put importance on periodical monitoring of BP/cholesterol levels by the GP Some (n = 8) Patients disagreed with taking more medications as a consequence of growing older, and did not feel physically better using their medication Some (n = 8) Patients independently researched and had knowledge Some (n = 8) Patients had autonomy to deprescribe from the prevantative medication Some (n = 8) Patients were afraid of developing a stroke or heart attack, as well as long-term effects of medications Afraid patients have fears, and have difficulties adjusting lifestyles Autonomous patients have littel fear, a lot of knowledge, are open to deprescribing, and havenegative attitudes towards medication use Controlling patients focus on healthy lifestyle, need monitoring of BP/cholesterol, and have no strong opinion towards medication use |
Rights and permissions
About this article
Cite this article
Forest, E., Ireland, M., Yakandawala, U. et al. Patient values and preferences on polypharmacy and deprescribing: a scoping review. Int J Clin Pharm 43, 1461–1499 (2021). https://doi.org/10.1007/s11096-021-01328-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-021-01328-w