Abstract
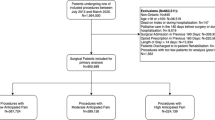
Background The changing of opioids during the transition of care from hospital to home may be associated with harm. Objective To compare patients receiving tapentadol IR versus oxycodone IR following orthopaedic surgery during hospitalisation with regard to the changing of opioids at hospital discharge. Setting A major metropolitan tertiary referral hospital in Australia. Methods This is a retrospective cohort study. Participants included adult orthopaedic surgery patients receiving postoperative tapentadol IR or oxycodone IR during hospitalisation between 1 January 2018 and 30 June 2019. Main outcome measure The proportion of patients for whom the opioid prescribed was changed at hospital discharge. Results The study cohort included 199 patients. Of these, 100 patients received oxycodone and 99 patients received tapentadol post-operatively during hospitalisation. The mean age was 66 years (SD, 12 years) and 111 (56%) were female. The most common surgeries were total knee arthroplasty (91, 46%), total hip arthroplasty (63, 32%) and shoulder surgery (26, 13%). Patients in the tapentadol group were more likely to be changed to a different opioid upon hospital discharge than the oxycodone group (57% versus 9%, difference 48% [95% CI 36–59%, p < 0.01). After adjusting for confounders, post-operative tapentadol use was more likely to be associated with opioid changing upon discharge (OR 16.5, 95% CI 6.7 to 40.8, p < 0.01). Conclusions The post-operative use of tapentadol IR during hospitalisation was associated with an increased likelihood of opioid changing at hospital discharge. This practice could have patient safety implications.

Similar content being viewed by others
Availability of data and material
The datasets generated during and/or analysed during the current study are not publicly available due to ethical restrictions but are available from the corresponding author on reasonable request.
Code availability
The code of this study is available on request from the corresponding author.
References
Schwartz S, Etropolski MS, Shapiro DY, Rauschkolb C, Vinik AI, Lange B, et al. A pooled analysis evaluating the efficacy and tolerability of tapentadol extended release for chronic, painful diabetic peripheral neuropathy. Clin Drug Investig. 2015;35:95–108. https://doi.org/10.1007/s40261-014-0249-3.
Tzschentke TM, Christoph T, Kogel B, Schiene K, Hennies HH, Englberger W et al. (-)-(1R,2R)-3-(3-dimethylamino-1-ethyl-2-methyl-propyl)-phenol hydrochloride (tapentadol HCl): a novel mu-opioid receptor agonist/norepinephrine reuptake inhibitor with broad-spectrum analgesic properties. J Pharmacol Exp Ther. 2007;323:265–76.
Polati E, Canonico PL, Schweiger V, Collino M. Tapentadol: an overview of the safety profile. J Pain Res. 2019;12:1569–76. https://doi.org/10.2147/jpr.S190154.
Wang X, Narayan SW, Penm J, Patanwala AE. Efficacy and Safety of Tapentadol Immediate Release for Acute Pain: A Systematic Review and Meta-analysis. Clin J Pain. 2020;36:399–409. https://doi.org/10.1097/AJP.0000000000000809.
Chou R, Gordon DB, de Leon-Casasola OA, Rosenberg JM, Bickler S, Brennan T, et al. Management of postoperative pain: a clinical practice guideline from the american pain society, the american society of regional anesthesia and pain medicine, and the american society of anesthesiologists’ committee on regional anesthesia, executive committee, and administrative council. J Pain. 2016;17:131–57. https://doi.org/10.1016/j.jpain.2015.12.008.
Stanley B, Norman AF, Collins LJ, Zographos GA, Lloyd‐Jones DM, Bonomo A, et al. Opioid prescribing in orthopaedic and neurosurgical specialties in a tertiary hospital: a retrospective audit of hospital discharge data. ANZ J Surg. 2018;88:1187–92. https://doi.org/10.1111/ans.14873.
Calcaterra SL, Yamashita TE, Min SJ, Keniston A, Frank JW, Binswanger IA. Opioid prescribing at hospital discharge contributes to chronic opioid use. J Gen Intern Med. 2016;31:478–85. https://doi.org/10.1007/s11606-015-3539-4.
Fine PG, Portenoy RK, Ad Hoc Expert Panel on Evidence R, Guidelines for Opioid R. Establishing "best practices" for opioid rotation: conclusions of an expert panel. J Pain Symp Manag. 2009;38:418–25. https://doi.org/10.1016/j.jpainsymman.2009.06.002.
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–9. https://doi.org/10.1016/j.jclinepi.2007.11.008.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81. https://doi.org/10.1016/j.jbi.2008.08.010.
Opioid Dose Equivalence. Faculty of Pain Medicine of the Australian and New Zealand College of Anaesthetists. http://fpm.anzca.edu.au/documents/opioid-dose-equivalence.pdf (accessed March 2020).
StataCorp. Stata Statistical Software: Release 16. In. TX:StataCorp LLC: College Station; 2019.
Knotkova H, Fine PG, Portenoy RK. Opioid rotation: the science and the limitations of the equianalgesic dose table. J Pain Symptom Manage. 2009;38:426–39. https://doi.org/10.1016/j.jpainsymman.2009.06.001.
About the PBS. Commonwealth of Australia, 2019. (Accessed November 2019, at http://www.pbs.gov.au/info/about-the-pbs#What_are_the_current_patient_fees_and_charges )
Oxycodone. Commonwealth of Australia, 2019. (Accessed November, 2019, at http://www.pbs.gov.au/medicine/item/2622B-5195K.)
Webster LR, Fine PG. Review and critique of opioid rotation practices and associated risks of toxicity. Pain Med. 2012;13:562–70. https://doi.org/10.1111/j.1526-4637.2012.01357.x.
Vogler S, Kilpatrick K, Babar ZU. Analysis of Medicine Prices in New Zealand and 16 European Countries. Value Health. 2015;18:484–92. https://doi.org/10.1016/j.jval.2015.01.003.
Kesselheim AS, Avorn J, Sarpatwari A. The high cost of prescription drugs in the United States: origins and prospects for reform. JAMA. 2016;316:858–71. https://doi.org/10.1001/jama.2016.11237.
Kwong WJ, Ozer-Stillman I, Miller JD, Haber NA, Russell MW, Kavanagh S. Cost-effectiveness analysis of tapentadol immediate release for the treatment of acute pain. Clin Ther. 2010;32:1768–81. https://doi.org/10.1016/j.clinthera.2010.09.011.
Lin J, Chow W, Kim MS, Rupnow MF. Real-world treatment pattern and outcomes among patients who took tapentadol IR or oxycodone IR. J Med Econ. 2013;16:685–90. https://doi.org/10.3111/13696998.2013.780177.
Paris A, Kozma CM, Chow W, Patel AM, Mody SH, Kim MS. Modeling the frequency and costs associated with postsurgical gastrointestinal adverse events for tapentadol IR versus oxycodone IR. Am Health Drug Benefits. 2013;6:567–75.
Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain-United States, 2016. JAMA. 2016;315:1624–45. https://doi.org/10.1001/jama.2016.1464.
Inacio MCS, Pratt NL, Roughead EE, Paxton EW, Graves SE. Opioid use after total hip arthroplasty surgery is associated with revision surgery. BMC Musculoskelet Disord. 2016;17:122. https://doi.org/10.1186/s12891-016-0970-6.
Namba RS, Inacio MCS, Pratt NL, Graves SE, Roughead EE, Paxton EW. Persistent opioid use following total knee arthroplasty: a signal for close surveillance. J Arthroplasty. 2018;33:331–6. https://doi.org/10.1016/j.arth.2017.09.001.
Rhon DI, Snodgrass SJ, Cleland JA, Sissel CD, Cook CE. Predictors of chronic prescription opioid use after orthopedic surgery: derivation of a clinical prediction rule. Perioper Med. 2018;7:25. https://doi.org/10.1186/s13741-018-0105-8.
Micromedex® RED BOOK® (electronic version). IBM Watson Health, Greenwood Village, Colorado, USA. https://www-micromedexsolutions-com.ezproxy2.library.arizona.edu/ (acessed March 2020).
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Consent to participate
Consent was not required for this study
Consent to publication
Consent for publication is not required for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, X., Tay, H.P., Narayan, S.W. et al. Comparison of opioid prescribing upon hospital discharge in patients receiving tapentadol versus oxycodone following orthopaedic surgery. Int J Clin Pharm 43, 1602–1608 (2021). https://doi.org/10.1007/s11096-021-01290-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-021-01290-7