Abstract
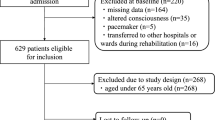
Background Polypharmacy or potentially inappropriate medications negatively affect the functional recovery of rehabilitation. However, limited research exists regarding the effect of decreasing in potentially inappropriate medications use on functional improvement of rehabilitation in geriatric Japanese patients. Objective To elucidate whether decreasing PIM during hospitalization could be a predictor of rehabilitation outcomes among geriatric patients in a convalescent rehabilitation setting. Setting This study was conducted at the convalescent rehabilitation ward in the Hitachinaka General Hospital in Japan. Methods This retrospective observational cohort study included consecutive geriatric patients admitted at the convalescent rehabilitation ward between 2010 and 2018. Participants were divided based on presence or absence of decreasing in potentially inappropriate medications use during hospitalization. A multiple linear regression analysis was performed to analyze whether decreasing potentially inappropriate medications use during hospitalization could be a predictor of Functional Independence Measure-Motor at discharge. Main outcome measures The primary outcome was the Functional Independence Measure-Motor at discharge. Results In total, 569 participants (interquartile range 73–85 years; 33.6% men) were included in the present study. A multiple linear regression analysis of Functional Independence Measure-Motor at discharge, adjusting for confounding factors, revealed that decreasing in potentially inappropriate medications use was independently correlated with Functional Independence Measure-Motor at discharge. In particular, the use of first-generation antihistamines, antipsychotics, benzodiazepines, and non-steroidal anti-inflammatory drugs among potentially inappropriate medications decreased significantly during hospitalization. Conclusion Decreased potentially inappropriate medications use during hospitalization may be a predictor of improvement of rehabilitation outcomes in geriatric patients.

Similar content being viewed by others
References
Kose E, Maruyama R, Okazoe S, Hayashi H. Impact of polypharmacy on the rehabilitation outcome of Japanese stroke patients in the convalescent rehabilitation ward. J Aging Res. 2016;2016:7957825.
Dumbreck S, Flynn A, Nairn M, Wilson M, Treweek S, Mercer SW, et al. Drug-disease and drug-drug interactions: systematic examination of recommendations in 12 UK national clinical guidelines. BMJ. 2015;350:h949.
Campbell SE, Seymour DG, Primrose WR. ACMEPLUS Project. A systematic literature review of factors affecting outcome in older medical patients admitted to hospital. Age Ageing. 2004;33(2):110–5.
Espino DV, Bazaldua OV, Palmer RF, Mouton CP, Parchman ML, Miles TP, et al. Suboptimal medication use and mortality in an older adult community-based cohort: results from the Hispanic EPESE Study. J Gerontol A Biol Sci Med Sci. 2006;61(2):170–5.
Hajjar ER, Cafiero AC, Hanlon JT. Polypharmacy in elderly patients. Am J Geriatr Pharmacother. 2007;5(4):345–51.
O'Connor MN, Gallagher P, O'Mahony D. Inappropriate prescribing: criteria, detection and prevention. Drugs Aging. 2012;29(6):437–52.
Spinewine A, Schmader KE, Barber N, Hughes C, Lapane KL, Swine C, et al. Appropriate prescribing in elderly people: how well can it be measured and optimised? Lancet. 2007;370(9582):173–84.
Kose E, Hirai T, Seki T, Hayashi H. Role of potentially inappropriate medication use in rehabilitation outcomes for geriatric patients after strokes. Geriatr Gerontol Int. 2018;18(2):321–8.
Kose E, Hirai T, Seki T. Clinical factors affecting potentially inappropriate medications at discharge in older stroke patients. Eur Ger Med. 2018;9(2):161–8.
Corsonello A, Pedone C, Lattanzio F, Lucchetti M, Garasto S, Muzio MD, et al. Potentially inappropriate medications and functional decline in elderly hospitalized patients. J Am Geriatr Soc. 2009;57(6):1007–144.
Nagai T, Wakabayashi H, Maeda K, Momosaki R, Nishiyama A, Murata H, et al. Influence of potentially inappropriate medications on activities of daily living for patients with osteoporotic vertebral compression fractures: a retrospective cohort study. J Orthop Sci. 2020;16(20):30086–90.
Kimura T, Ogura F, Yamamoto K, Uda A, Nishioka T, Kume M, et al. Potentially inappropriate medications in elderly Japanese patients: effects of pharmacists’ assessment and intervention based on Screening Tool of Older Persons’ Potentially Inappropriate Prescriptions criteria ver.2. J Clin Pharm Ther. 2017;42(2):209–14.
Fick DM, Semla TP, Steinman M, Beizer J, Brandt N, Dombrowski R, et al. American Geriatrics Society 2019 Updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674–94.
Bouillanne O, Morineau G, Dupont C, Coulombel I, Vincent JP, Nicolis I, et al. Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr. 2005;82(4):777–83.
Cereda E, Vanotti A. The new geriatric nutritional risk index is a good predictor of muscle dysfunction in institutionalized older patients. Clin Nutr. 2007;26(1):78–83.
Yamada K, Furuya R, Takita T, Maruyama Y, Yamaguchi Y, Ohkawa S, et al. Simplified nutritional screening tools for patients on maintenance hemodialysis. Am J Clin Nutr. 2008;87(1):106–13.
Shah B, Sucher K, Hollenbeck CB. Comparison of ideal body weight equations and published height-weight tables with body mass index tables for healthy adults in the United States. Nutr Clin Pract. 2006;21(3):312–9.
Kinugasa Y, Kato M, Sugihara S, Hirai M, Yamada K, Yanagihara K, et al. Geriatric nutritional risk index predicts functional dependency and mortality in patients with heart failure with preserved ejection fraction. Circ J. 2013;77(3):705–11.
Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the functional independence measure: a quantitative review. Arch Phys Med Rehabil. 1996;77(12):1226–322.
Stockl KM, Le L, Zhang S, Harada AS. Clinical and economic outcomes associated with potentially inappropriate prescribing in the elderly. Am J Manag Care. 2010;16(1):e1–e10.
Fick DM, Mion LC, Beers MH, Waller JL. Health outcomes associated with potentially inappropriate medication use in older adults. Res Nurs Health. 2008;31:42–51.
Iaboni A, Rawson K, Burkett C, Lenze EJ, Flint AJ. Potentially inappropriate medications and the time to full functional recovery after hip fracture. Drugs Aging. 2017;34(9):723–8.
Fabbietti P, Ruggiero C, Sganga F, Fusco S, Mammarella F, Barbini N, et al. Effects of hyperpolypharmacy and potentially inappropriate medications (PIMs) on functional decline in older patients discharged from acute care hospitals. Arch Gerontol Geriatr. 2018;77:158–62.
Varga S, Alcusky M, Keith SW, Hegarty SE, Canale SD, Lombardi M, et al. Hospitalization rates during potentially inappropriate medication use in a large population-based cohort of older adults. Br J Clin Pharmacol. 2017;83(11):2572–80.
de Nascimento MM, Mambrini JV, Lima-Costa MF, Araújo Firmo JO, Viana Peixoto SW, de Loyola Filho AI. Potentially inappropriate medications: predictor for mortality in a cohort of communitydwelling older adults. Eur J Clin Pharmacol. 2017;73(5):615–21.
Novak LP. Aging, total body potassium, fat-free mass, and cell mass in males and females between ages 18 and 85 years. J Gerontol. 1972;27(4):438–43.
Ancelin ML, Artero S, Portet F, Dupuy AM, Touchon J, Ritchie K. Non-degenerative mild cognitive impairment in elderly people and use of anticholinergic drugs: longitudinal cohort study. BMJ. 2006;332:455–9.
Marshall S, Bauer J, Isenring E. The consequences of malnutrition following discharge from rehabilitation to the community: a systematic review of current evidence in older adults. J Hum Nutr Diet. 2014;27(2):133–41.
Kose E, Wakabayashi H. Rehabilitation pharmacotherapy: a scoping review. Geriatr Gerontol Int. 2020;20(7):655–33.
Acknowledgements
The authors thank the manager of Hitachinaka Gereral Hospital who agreed for this study to take place.
Funding
This study was not sponsored or funded by any industry, government, or institution.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kose, E., Hirai, T., Seki, T. et al. The impact of decreasing potentially inappropriate medications on activities of daily living in a convalescent rehabilitation setting. Int J Clin Pharm 43, 577–585 (2021). https://doi.org/10.1007/s11096-020-01165-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-020-01165-3