Abstract
Background Several anticholinergic scales and equations to evaluate the anticholinergic burden have been previously created. Association of these instruments with the anticholinergic outcomes are usually estimated by means of hypothesis contrast tests, which ignore the size of the association effect. Objective To evaluate the effect size of the associations between the scores on cumulative anticholinergic burden instruments with peripheral or central anticholinergic adverse outcomes in older patients. Setting Internal medicine ward of a Tertiary University Hospital. Methods A case–control study was conducted in patients over 65 years who were admitted to two internal medicine wards of a Portuguese university hospital. The Anticholinergic Drug Scale, Anticholinergic Risk Scale, Anticholinergic Cognitive Burden scale and Drug Burden Index were used to calculate the patients’ anticholinergic burden. Peripheral (dry mouth—swab technique; dry eye—Schirmer test) and central (falls and cognitive impairment—Mini-Mental State Examination) anticholinergic adverse outcomes were investigated. The Barthel Index was used to assess overall physical functionality. The Mann–Whitney test was used to evaluate probabilistic differences in the anticholinergic scores between case and control individuals. To establish the effect size of the associations, the area under the curve of the receiver operating characteristics curve was calculated. Main outcome measure Anticholinergic adverse effects. Results A total of 250 patients (mean age 81.67 years, standard deviation 7.768; 50% females) were included. In total, 148 patients (59.2%) presented with dry mouth, 85 (34%) with dry eye, 141 (56.4%) with impaired functionality, 44 (17.6%) with a history of falls and 219 (87.6%) with cognitive impairment. Significant differences (p < 0.05) were obtained for the majority of the associations between Anticholinergic Drug Scale, Anticholinergic Risk Scale, Anticholinergic Cognitive Burden and Drug Burden Index and adverse effects. Conversely, the effect sizes of these associations ranged from “fail” (area under the curve 0.5 to 0.6) to “fair” (area under the curve 0.7 to 0.8). Conclusion Although significant differences in the scores of anticholinergic burden instruments and adverse outcomes may exist, the effect sizes of these associations ranged from ‘fail’ to ‘fair’, which limits their utility in preventing anticholinergic adverse outcomes with medication review interventions.
Similar content being viewed by others
References
Naples JG, Marcum ZA, Perera S, Gray SL, Newman AB, Simonsick EM, et al. Concordance between anticholinergic burden scales. J Am Geriatr Soc. 2015;63:2120–4.
Nishtala PS, Salahudeen MS, Hilmer SN. Anticholinergics: theoretical and clinical overview. Expert Opin Drug Saf. 2016;15:753–68.
Duran CE, Azermai M, Vander Stichele RH. Systematic review of anticholinergic risk scales in older adults. Eur J Clin Pharmacol. 2013;69:1485–96.
Salahudeen MS, Duffull SB, Nishtala PS. Anticholinergic burden quantified by anticholinergic risk scales and adverse outcomes in older people: a systematic review. BMC Geriatr. 2015;15:31.
Mayer T, Haefeli WE, Seidling HM. Different methods, different results—How do available methods link a patient’s anticholinergic load with adverse outcomes? Eur J Clin Pharmacol. 2015;71:1299–314.
Villalba-Moreno AM, Alfaro-Lara ER, Perez-Guerrero MC, Nieto-Martin MD, Santos-Ramos B. Systematic review on the use of anticholinergic scales in poly pathological patients. Arch Gerontol Geriatr. 2016;62:1–8.
Kersten H, Wyller TB. Anticholinergic drug burden in older people’s brain—How well is it measured? Basic Clin Pharmacol Toxicol. 2014;114:151–9.
Rudd KM, Raehl CL, Bond CA, Abbruscato TJ, Stenhouse AC. Methods for assessing drug-related anticholinergic activity. Pharmacotherapy. 2005;25:1592–601.
Cardwell K, Hughes CM, Ryan C. The association between anticholinergic medication burden and health related outcomes in the ‘oldest old’: a systematic review of the literature. Drugs Aging. 2015;32:835–48.
Welsh TJ, van der Wardt V, Ojo G, Gordon AL, Gladman JRF. Anticholinergic drug burden tools/scales and adverse outcomes in different clinical settings: a systematic review of reviews. Drugs Aging. 2018;35:523–38.
Sullivan GM, Feinn R. Using effect size-or why the P value is not enough. J Grad Med Educ. 2012;4:279–82.
Oliveira J, Cabral AC, Lavrador M, Costa FA, Almeida FF, Macedo A, et al. Contribution of different patient information sources to create the best possible medication history. Acta Med Port. 2020;33:384–9.
Rudolph JL, Salow MJ, Angelini MC, McGlinchey RE. The anticholinergic risk scale and anticholinergic adverse effects in older persons. Arch Intern Med. 2008;168:508–13.
Carnahan RM, Lund BC, Perry PJ, Pollock BG, Culp KR. The Anticholinergic Drug Scale as a measure of drug-related anticholinergic burden: associations with serum anticholinergic activity. J Clin Pharmacol. 2006;46:1481–6.
Campbell NL, Maidment I, Fox C, Khan B, Boustani M. The 2012 Update to the Anticholinergic Cognitive Burden Scale. J Am Geriatr Soc. 2013;61:S142–3.
Hilmer SN, Mager DE, Simonsick EM, Cao Y, Ling SM, Windham BG, et al. A drug burden index to define the functional burden of medications in older people. Arch Intern Med. 2007;167:781–7.
Hilmer SN, Mager DE, Simonsick EM, Ling SM, Windham BG, Harris TB, et al. Drug burden index score and functional decline in older people. Am J Med. 2009;122(1142–9):e1–2.
O’Connell J, Burke E, Mulryan N, O’Dwyer C, Donegan C, McCallion P, et al. Drug burden index to define the burden of medicines in older adults with intellectual disabilities: an observational cross-sectional study. Br J Clin Pharmacol. 2018;84:553–67.
Gnjidic D, Bell JS, Hilmer SN, Lonnroos E, Sulkava R, Hartikainen S. Drug Burden Index associated with function in community-dwelling older people in Finland: a cross-sectional study. Ann Med. 2012;44:458–67.
Kersten H, Molden E, Tolo IK, Skovlund E, Engedal K, Wyller TB. Cognitive effects of reducing anticholinergic drug burden in a frail elderly population: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2013;68:271–8.
Jongerius PH, van Limbeek J, Rotteveel JJ. Assessment of salivary flow rate: biologic variation and measure error. Laryngoscope. 2004;114:1801–4.
Lofgren CD, Wickstrom C, Sonesson M, Lagunas PT, Christersson C. A systematic review of methods to diagnose oral dryness and salivary gland function. BMC Oral Health. 2012;12:29.
Schirmer Test. Available at: https://www.sciencedirect.com/topics/medicine-and-dentistry/schirmer-test. Accessed 2019-07-18..
Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J. 1965;14:61–5.
Pasina L, Djade CD, Lucca U, Nobili A, Tettamanti M, Franchi C, et al. Association of anticholinergic burden with cognitive and functional status in a cohort of hospitalized elderly: comparison of the anticholinergic cognitive burden scale and anticholinergic risk scale: results from the REPOSI study. Drugs Aging. 2013;30:103–12.
Folstein MF, Folstein SE, McHugh PR. Mini-mental state A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98.
Gnjidic D, Cumming RG, Le Couteur DG, Handelsman DJ, Naganathan V, Abernethy DR, et al. Drug Burden Index and physical function in older Australian men. Br J Clin Pharmacol. 2009;68:97–105.
Fritz CO, Morris PE, Richler JJ. Effect size estimates: current use, calculations, and interpretation. J Exp Psychol Gen. 2012;141:2–18.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Mahwah: Lawrence Erlbaum; 1988.
Hajian-Tilaki K. Receiver operating characteristic (ROC) curve analysis for medical diagnostic test evaluation. Caspian J Intern Med. 2013;4:627–35.
The Area Under a ROC Curve. Available at: http://gim.unmc.edu/dxtests/roc3.htm. Accessed 18 July 2019.
Millsop JW, Wang EA, Fazel N. Etiology, evaluation, and management of xerostomia. Clin Dermatol. 2017;35:468–76.
Schreiber JB. New paradigms for considering statistical significance: a way forward for health services research journals, their authors, and their readership. Res Soc Adm Pharm. 2019;16:591–4.
Wasserstein RL, Lazar NA. The ASA statement on p-values: context, process, and purpose. The American Statistician. 2016;70:129–33.
Kersten H, Molden E, Willumsen T, Engedal K, Bruun WT. Higher anticholinergic drug scale (ADS) scores are associated with peripheral but not cognitive markers of cholinergic blockade. cross sectional data from 21 Norwegian nursing homes. Br J Clin Pharmacol. 2013;75:842–9.
Wouters H, van der Meer H, Taxis K. Quantification of anticholinergic and sedative drug load with the Drug Burden Index: a review of outcomes and methodological quality of studies. Eur J Clin Pharmacol. 2017;73:257–66.
Whalley LJ, Sharma S, Fox HC, Murray AD, Staff RT, Duthie AC, et al. Anticholinergic drugs in late life: adverse effects on cognition but not on progress to dementia. J Alzheimers Dis. 2012;30:253–61.
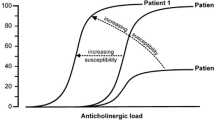
Boustani M, Campbell N, Munger S, Maidment I, Fox C. Impact of anticholinergics on the aging brain: a review and practical application. Aging Health. 2008;4:311–20.
Gnjidic D, Le Couteur DG, Naganathan V, Cumming RG, Creasey H, Waite LM, et al. Effects of drug burden index on cognitive function in older men. J Clin Psychopharmacol. 2012;32:273–7.
Bostock CV, Soiza RL, Mangoni AA. Associations between different measures of anticholinergic drug exposure and Barthel Index in older hospitalized patients. Therap Adv Drug Saf. 2013;4:235–45.
Tan MP, Tan GJ, Mat S, Luben RN, Wareham NJ, Khaw KT, et al. Use of Medications with anticholinergic properties and the long-term risk of hospitalization for falls and fractures in the EPIC-Norfolk longitudinal cohort study. Drugs Aging. 2019;37:105–14.
Salahudeen MS, Chyou TY, Nishtala PS. Serum anticholinergic activity and cognitive and functional adverse outcomes in older people: a systematic review and meta-analysis of the literature. PLoS ONE. 2016;11:e0151084.
Alba AC, Agoritsas T, Walsh M, Hanna S, Iorio A, Devereaux PJ. Discrimination and calibration of clinical prediction models: users’ guides to the medical literature. JAMA. 2017;318:1377–84.
Kaufmann CP, Tremp R, Hersberger KE, Lampert ML. Inappropriate prescribing: a systematic overview of published assessment tools. Eur J Clin Pharmacol. 2014;70:1–11.
Acknowledgements
Marta Lavrador acknowledges the FCT—Fundação para a Ciência e a Tecnologia for funding her with a Doctoral Grant.
Funding
Marta Lavrador obtained a complete Doctoral Grant from the FCT—Fundação para a Ciência e a Tecnologia (SFRH/BD/123678/2016). No other external funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lavrador, M., Cabral, A.C., Figueiredo, I.V. et al. Size of the associations between anticholinergic burden tool scores and adverse outcomes in older patients. Int J Clin Pharm 43, 128–136 (2021). https://doi.org/10.1007/s11096-020-01117-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-020-01117-x