Abstract
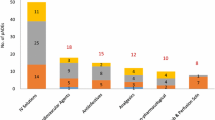
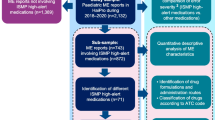
Background Medication errors occur frequently in intensive care units (ICU). Voluntarily reported medication errors form an easily available source of information. Objective This study aimed to characterize prescribing, monitoring and medication transfer errors that were voluntarily reported in the ICU, in order to reveal medication safety issues. Setting This retrospective data analysis study included reports of medication errors from eleven Dutch ICU’s from January 2016 to December 2017. Method We used data extractions from the incident reporting systems of the participating ICU’s. The reports were transferred into one database and categorized into type of error, cause, medication (groups), and patient harm. Descriptive statistics were used to calculate the proportion of medication errors and the distribution of subcategories. Based on the analysis, ICU medication safety issues were revealed. Main outcome measure The main outcome measure was the proportion of prescribing, monitoring and medication transfer error reports. Results Prescribing errors were reported most frequently (n = 233, 33%), followed by medication transfer errors (n = 85, 12%) and monitoring errors (n = 27, 4%). Other findings were: medication transfer errors frequently caused serious harm, especially the omission of home medication involving the central nervous system and proton pump inhibitors; omissions and dosing errors occurred most frequently; protocol problems caused a quarter of the medication errors; and medications needing blood level monitoring (e.g. tacrolimus, vancomycin, heparin and insulin) were frequently involved. Conclusion This analysis of voluntarily reported prescribing, monitoring and medication transfer errors warrants several improvement measures in these processes, which may help to increase medication safety in the ICU.



Similar content being viewed by others
Abbreviations
- APTT:
-
Activated Partial Thromboplastin Time
- ATC:
-
Anatomical Therapeutic Chemical (a medication classification system)
- CPOE:
-
Computerized provider order entry
- CNS:
-
Central nervous system
- ICU:
-
Intensive care unit
- INR:
-
International normalized ratio
- IRS:
-
Incident reporting system
- IT:
-
Information technology
- LMWH:
-
Low molecule weight heparin
- ME:
-
Medication errors
- MoE:
-
Monitoring errors
- MTE:
-
Medication transfer errors
- PE:
-
Prescribing errors
- PIS:
-
Patient Information System
- TDM:
-
Therapeutic drug monitoring
References
Garrouste-Orgeas M, Philippart F, Bruel C, Max A, Lau N, Misset B. Overview of medical errors and adverse events. Ann Intensive Care. 2012;2(1):2.
Rothschild JM, Landrigan CP, Cronin JW, Kaushal R, Lockley SW, Burdick E, et al. The critical care safety study: the incidence and nature of adverse events and serious medical errors in intensive care. Crit Care Med. 2005;33(8):1694–700.
Kane-Gill SL, Jacobi J, Rothschild JM. Adverse drug events in intensive care units: risk factors, impact, and the role of team care. Crit Care Med. 2010;38(6 Suppl):S83–S8989.
Garrouste-Orgeas M, Timsit JF, Vesin A, Schwebel C, Arnodo P, Lefrant JY, et al. Selected medical errors in the intensive care unit: results of the IATROREF study: parts I and II. Am J Respir Crit Care Med. 2010;181(2):134–42.
Cullen DJ, Sweitzer BJ, Bates DW, Burdick E, Edmondson A, Leape LL. Preventable adverse drug events in hospitalized patients: a comparative study of intensive care and general care units. Crit Care Med. 1997;25(8):1289–97.
Kane-Gill SL, Kowiatek JG, Weber RJ. A comparison of voluntarily reported medication errors in intensive care and general care units. Qual Saf Health Care. 2010;19(1):55–9.
Heselmans A, van Krieken J, Cootjans S, Nagels K, Filliers D, Dillen K, et al. Medication review by a clinical pharmacist at the transfer point from ICU to ward: a randomized controlled trial. J Clin Pharm Ther. 2015;40(5):578–83.
Agency EM. Medication errors [cited 2019 26 Nov]. Available from: https://www.ema.europa.eu/ema/index.jsp?curl=pages/special_topics/general/general_content_000570.jsp&mid=WC0b01ac0580659655.
Thomas AN, MacDonald JJ. A review of patient safety incidents reported as 'severe' or 'death' from critical care units in England and Wales between 2004 and 2014. Anaesthesia. 2016;71(9):1013–23.
Thomas AN, Panchagnula U. Medication-related patient safety incidents in critical care: a review of reports to the UK national patient safety agency. Anaesthesia. 2008;63(7):726–33.
Thomas AN, Taylor RJ. An analysis of patient safety incidents associated with medications reported from critical care units in the North West of England between 2009 and 2012. Anaesthesia. 2014;69(7):735–45.
Latif A, Rawat N, Pustavoitau A, Pronovost PJ, Pham JC. National study on the distribution, causes, and consequences of voluntarily reported medication errors between the ICU and non-ICU settings. Crit Care Med. 2013;41(2):389–98.
Bosma LBE, Hunfeld NGM, Quax RAM, Meuwese E, Melief P, van Bommel J, et al. The effect of a medication reconciliation program in two intensive care units in the Netherlands: a prospective intervention study with a before and after design. Ann Intensive Care. 2018;8(1):19.
Ridley SA, Booth SA, Thompson CM. Intensive care society's working group on adverse I. Prescription errors in UK critical care units. Anaesthesia. 2004;59(12):1193–200.
Kopp BJ, Erstad BL, Allen ME, Theodorou AA, Priestley G. Medication errors and adverse drug events in an intensive care unit: direct observation approach for detection. Crit Care Med. 2006;34(2):415–25.
Montesi G, Lechi A. Prevention of medication errors: detection and audit. Br J Clin Pharmacol. 2009;67(6):651–5.
Mahajan RP. Critical incident reporting and learning. Br J Anaesth. 2010;105(1):69–75.
Kiekkas P, Aretha D, Stefanopoulos N, Baltopoulos GI. Knowledge is power: studying critical incidents in intensive care. Crit Care. 2012;16(1):102.
VMS. The Dutch patient safety programme [cited 2019 26 Nov]. Available from: https://www.medicalfacts.nl/2014/12/11/engelstalige-film-over-vms-veiligheidsprogramma/.
Infoland. Risk management software: change risks into opportunities! [cited 2019 26 Nov]. Available from: https://www.infoland.eu/software/risk-management/.
Cheung KC, van den Bemt PM, Bouvy ML, Wensing M, De Smet PA. A nationwide medication incidents reporting system in The Netherlands. J Am Med Inform Assoc. 2011;18(6):799–804.
Arabi YM, Al Owais SM, Al-Attas K, Alamry A, AlZahrani K, Baig B, et al. Learning from defects using a comprehensive management system for incident reports in critical care. Anaesth Intensive Care. 2016;44(2):210–20.
Brunsveld-Reinders AH, Arbous MS, De Vos R, De Jonge E. Incident and error reporting systems in intensive care: a systematic review of the literature. Int J Qual Health Care. 2016;28(1):2–13.
Kuperman GJ, Bobb A, Payne TH, Avery AJ, Gandhi TK, Burns G, et al. Medication-related clinical decision support in computerized provider order entry systems: a review. J Am Med Inform Assoc. 2007;14(1):29–40.
Z-index. Dutch drug database G-Standaard Medication Surveillance [cited 2019 26 Nov]. Available from: https://www.z-index.nl/english.
Horn E, Jacobi J. The critical care clinical pharmacist: evolution of an essential team member. Crit Care Med. 2006;34(3 Suppl):S46–51.
Kane SL, Weber RJ, Dasta JF. The impact of critical care pharmacists on enhancing patient outcomes. Intensive Care Med. 2003;29(5):691–8.
MacLaren R, Bond CA. Effects of pharmacist participation in intensive care units on clinical and economic outcomes of critically ill patients with thromboembolic or infarction-related events. Pharmacotherapy. 2009;29(7):761–8.
MacLaren R, Bond CA, Martin SJ, Fike D. Clinical and economic outcomes of involving pharmacists in the direct care of critically ill patients with infections. Crit Care Med. 2008;36(12):3184–9.
Papadopoulos J, Rebuck JA, Lober C, Pass SE, Seidl EC, Shah RA, et al. The critical care pharmacist: an essential intensive care practitioner. Pharmacotherapy. 2002;22(11):1484–8.
Bosma BE, van den Bemt P, Melief P, van Bommel J, Tan SS, Hunfeld NGM. Pharmacist interventions during patient rounds in two intensive care units: clinical and financial impact. Neth J Med. 2018;76(3):115–24.
Chisholm-Burns MA, Kim Lee J, Spivey CA, Slack M, Herrier RN, Hall-Lipsy E, et al. US pharmacists' effect as team members on patient care: systematic review and meta-analyses. Med Care. 2010;48(10):923–33.
Montazeri M, Cook DJ. Impact of a clinical pharmacist in a multidisciplinary intensive care unit. Crit Care Med. 1994;22(6):1044–8.
Bond CA, Raehl CL. Clinical pharmacy services, pharmacy staffing, and hospital mortality rates. Pharmacotherapy. 2007;27(4):481–93.
Provost LP. Analytical studies: a framework for quality improvement design and analysis. BMJ Qual Saf. 2011;20(Suppl 1):i92–i9696.
Vo TH, Charpiat B, Catoire C, Juste M, Roubille R, Rose FX, et al. Tools for assessing potential significance of pharmacist interventions: a systematic review. Drug Saf. 2016;39(2):131–46.
Shulman R, McKenzie CA, Landa J, Bourne RS, Jones A, Borthwick M, et al. Pharmacist's review and outcomes: treatment-enhancing contributions tallied, evaluated, and documented (PROTECTED-UK). J Crit Care. 2015;30(4):808–13.
La MK, Thompson Bastin ML, Gisewhite JT, Johnson CA, Flannery AH. Impact of restarting home neuropsychiatric medications on sedation outcomes in medical intensive care unit patients. J Crit Care. 2018;43:102–7.
van Sluisveld N, Oerlemans A, Westert G, van der Hoeven JG, Wollersheim H, Zegers M. Barriers and facilitators to improve safety and efficiency of the ICU discharge process: a mixed methods study. BMC Health Serv Res. 2017;17(1):251.
Sevransky JE, Checkley W, Herrera P, Pickering BW, Barr J, Brown SM, et al. Protocols and hospital mortality in critically Ill patients: the united states critical illness and injury trials group critical illness outcomes study. Crit Care Med. 2015;43(10):2076–84.
Corwin GS, Mills PD, Shanawani H, Hemphill RR. Root cause analysis of ICU adverse events in the veterans health administration. Jt Comm J Qual Patient Saf. 2017;43(11):580–90.
Nolan TW. System changes to improve patient safety. BMJ. 2000;320(7237):771–3.
Egan S, Murphy PG, Fennell JP, Kelly S, Hickey M, McLean C, et al. Using six sigma to improve once daily gentamicin dosing and therapeutic drug monitoring performance. BMJ Qual Saf. 2012;21(12):1042–51.
Umpierrez GE, Pasquel FJ. Management of inpatient hyperglycemia and diabetes in older adults. Diabetes Care. 2017;40(4):509–17.
Krinsley JS, Chase JG, Gunst J, Martensson J, Schultz MJ, Taccone FS, et al. Continuous glucose monitoring in the ICU: clinical considerations and consensus. Crit Care. 2017;21(1):197.
Preiser JC, Lheureux O, Thooft A, Brimioulle S, Goldstein J, Vincent JL. Near-continuous glucose monitoring makes glycemic control safer in ICU patients. Crit Care Med. 2018;46(8):1224–9.
Kiekkas P, Aretha D, Karga M, Karanikolas M. Self report may lead to underestimation of 'wrong dose' medication errors. Br J Clin Pharmacol. 2009;68(6):963–4.
Acknowledgements
We thank Christine Earl for reviewing the article on English grammar.
Funding
No specific funding was obtained.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicting interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bosma, B.E., Hunfeld, N.G.M., Roobol-Meuwese, E. et al. Voluntarily reported prescribing, monitoring and medication transfer errors in intensive care units in The Netherlands. Int J Clin Pharm 43, 66–76 (2021). https://doi.org/10.1007/s11096-020-01101-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-020-01101-5