Abstract
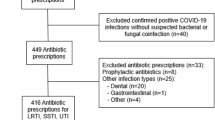
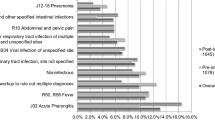
Background Antimicrobial stewardship programs ensure antibiotic therapy is used appropriately and includes de-escalation when clinical status or culture data indicates broad-spectrum agents are no longer needed. Although the impact of infectious diseases clinical pharmacists has been well documented, there is limited research evaluating the impact of adult internal medicine clinical pharmacists on broad-spectrum antibiotic de-escalation while rounding on internal medicine teams. Objective To determine if broad-spectrum antibiotics were de-escalated more regularly and more rapidly in patients on internal medicine services with a rounding pharmacist at the bedside compared to internal medicine services without rounding pharmacists. Setting A single 700 bed academic medical center in the United States of America. Method This was a prospective observational cohort chart review. Main outcome measure The primary endpoint was appropriate broad-spectrum antibiotic de-escalation within 72 h or upon return of culture results. Result A total of 64 patients were included in this study with 39 in the pharmacist group and 25 in the no pharmacist group. De-escalation occurred in 35/39 patients on services with pharmacists and in 13/25 patients on services without pharmacists (p = 0.001). In terms of mean days of broad-spectrum antibiotic therapy, services with rounding pharmacists saw patients on Methicillin-resistant Staphylococcus aureus coverage for an average of 2.12 days of their duration of therapy compared to 2.8 days in those without pharmacists (p = 0.821). Services with rounding pharmacists saw patients on Pseudomonas aeruginosa coverage for 2 days of their length of stay compared to 3 days in those without pharmacists (0.398). Conclusion This data shows that broad-spectrum antibiotics were de-escalated more frequently on medicine services with rounding pharmacists compared to services without pharmacists.
Similar content being viewed by others
References
MacDougall C, Polk RE. Antimicrobial stewardship programs in health care systems. Clin Microbiol Rev. 2005;18(4):638–56.
Dellit TH, Owens RC, McGowan JE Jr, Gerding DN, Weinstein RA, Burke JP, et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis. 2007;44:159–77.
Shlaes DM, Gerding DN, John JF Jr, Craig WA, Bornstein DL, Duncan RA, et al. Society for Healthcare Epidemiology of America and Infectious Diseases Society of America Joint Committee on the Prevention of Antimicrobial Resistance: Guidelines for the prevention of antimicrobial resistance in hospitals. Clin Infect Dis. 1997;25:584–99.
Tonna AP, Stewart D, West B, McCaig D. Antimicrobial optimization is secondary care: the pharmacist as part of a multidisciplinary antimicrobial programme—a literature review. Int J Antimicrob Agents. 2008;31:511–7.
Toth NR, Chambers RM, Davis SL. Implementation of a care bundle for antimicrobial stewardship. Am J Health-Syst Pharm. 2010;67:746–9.
Yu K, Rho J, Morcos M, Nomura J, Kaplan D, Sakamoto K, et al. Evaluation of dedicated infectious diseases pharmacists on antimicrobial stewardship teams. Am J Health-Syst Pharm. 2014;71:1019–28.
Doron S, Davidson LE. Antimicrobial stewardship. Mayo Clin Proc. 2011;86(11):1113–23.
Gums JG, Yancey RW, Hamilton CA, Kubilis PS. A randomized, prospective study measuring outcomes after antibiotic therapy intervention by a multidisciplinary consult team. Pharmacotherapy. 1999;19(12):1369–77.
Dyar OJ, Huttner B, Schouten J, Pulcini C. What is antimicrobial stewardship? Clin Microbiol Infect. 2017;11:793–8.
Parente DM, Morton J. Role of the pharmacist in antimicrobial stewardship. Med Clin North Am. 2018;102(5):929–36.
Weier N, Tebano G, Thilly N, Demore B, Pulcini C, Zaidi STR. Pharmacist participation in antimicrobial stewardship in Australian and French hospitals: a cross-sectional nationwide survey. J Antimicrob Chemother. 2018;73(3):804–13.
Heil EL, Kuti JL, Bearden DT, Gallagher JC. The essential role of pharmacists in antimicrobial stewardship. Infect Control Hosp Epidemiol. 2016;37(7):753–4.
Garau J, Bassetti M. Role of pharmacists in antimicrobial stewardship programmes. Int J Clin Pharm. 2018;40(5):948–52.
Cunha CB. Antimicrobial stewardship programs: principles and practice. Med Clin North Am. 2018;102(5):797–803.
Huang CY, Hseih RW, Yen HT, Hsu TC, Chen CY, Chen YC, et al. Short-versus long-course antibiotics in osteomyelitis: a systematic review and meta-analysis. Int J Antimicrob Agents. 2019;53(3):246–60.
Magedanz L, Silliprandi EM, Pires dos Santos R. Impact of the pharmacist on a multidisciplinary team in an antimicrobial stewardship program: a quasi-experimental study. Int J Clin Pharm. 2012;34:290–94.
Pardo J, Klinker KP, Borgert SJ, Trikha G, Rand KH, Ramphal R. Time to positivity of blood cultures supports antibiotic de-escalation at 48 hours. Ann Pharmacotherapy. 2014;48(1):33–40.
Apisarnthanarak A, Lapcharoen P, Vanichkul P, Srisaeng-Ngoen T, Mundy LM. Design and analysis of a pharmacist-enhanced antimicrobial stewardship program in Thailand. Am J Infect Control. 2015;43(9):956–9.
The Joint Commission. New antimicrobial stewardship standard; Standard MM.09.01.01 Issued June 22, 2016.
Fortin R. Role of the pharmacist in antimicrobial stewardship. Rhode Island Med J. 2008;101(5):26–7.
DiDiodato G, McAthur L. Transition from a dedicated to a non-dedicated, ward-based pharmacist antimicrobial stewardship programme model in a non-academic hospital and its impact on length of stay of patients admitted with pneumonia: a prospective observational study. BMJ Open Quality. 2017;6:e000060.
Acknowledgements
The authors would like to acknowledge Catessa Howard, PharmD, BCIDP, Zach Griffith, PharmD, and Kelsea Seago, PharmD, BCOP for their help in the data collection process.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Conflicts of interest
The authors have no financial support or personal connections to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ford, B.A., Martello, J.L., Wietholter, J.P. et al. Antibiotic de-escalation on internal medicine services with rounding pharmacists compared to services without. Int J Clin Pharm 42, 772–776 (2020). https://doi.org/10.1007/s11096-020-01029-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-020-01029-w