Abstract
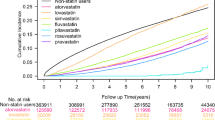
Background While there is clear evidence for the benefit of statins in the secondary prevention of cardiovascular and cerebrovascular events, there is a lack of research on the effects of statin regimens in older patients aged 75 years and over. Objectives To compare the effectiveness of statin regimens in the secondary prevention of ischemic cardiovascular and cerebrovascular events among patients aged 75 years and over. Setting Claims data from the South Korean National Health Insurance Database from 2006 to 2014. Methods This retrospective cohort study included patients aged 75–100 years with a prior history of cardiovascular or cerebrovascular disease who began statin therapy in 2009–2011. Propensity score matching and the Cox proportional hazards regression model were used to compare the effectiveness of the statin regimens in secondary prevention. Main outcome measure The hazard ratios for ischemic cardiovascular and cerebrovascular events and all-cause mortality. Results Neither high nor low-intensity statin therapy significantly differed from moderate-intensity statin therapy in preventing ischemic cardiovascular and cerebrovascular events or all-cause mortality. Of the moderate-intensity statin therapies, the use of 10 mg rosuvastatin was more strongly associated with a reduced risk of ischemic cardiovascular and cerebrovascular events than was 10 mg atorvastatin [HR 0.79 (95% CI 0.64–0.98), p = 0.029]. Subgroup analysis revealed that the protective effects of 10 mg rosuvastatin against ischemic cardiovascular and cerebrovascular events were more obvious for patients who were 75–79 years old, those who were statin-adherent, those who did not have diabetes mellitus at baseline, and those who were non-adherent to aspirin or antiplatelet drugs during the selection and follow-up periods. Conclusion The results of this study support the preferential prescription of moderate-intensity rosuvastatin over moderate-intensity atorvastatin for the secondary prevention of ischemic cardiovascular and cerebrovascular events in older patients aged ≥ 75 years.

Similar content being viewed by others
References
Forman D, Wenger NK. What do the recent American Heart Association/American College of Cardiology Foundation Clinical Practice Guidelines tell us about the evolving management of coronary heart disease in older adults? J Geriatr Cardiol. 2013;10(2):123–8.
Jacobson TA, Maki KC, Orringer CE, Jones PH, Kris-Etherton P, Sikand G, et al. National lipid association recommendations for patient-centered management of dyslipidemia: part 2. J Clin Lipidol. 2015;9(6 Suppl):S1-122.e1.
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation. 2016;133(4):e38–360.
Stone NJ, Robinson J, Lichtenstein AH, Merz CNB, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S1–45.
Leya M, Stone NJ. Statin prescribing in the elderly: special considerations. Curr Atheroscler Rep. 2017;19(11):47.
Beers MH, Stefanacci RG. The class effect: is it relevant to geriatrics? J Am Geriatr Soc. 2005;53(8):1402–4.
Knopp RH. Drug treatment of lipid disorders. N Engl J Med. 1999;341(7):498–511.
Cheol Seong S, Kim YY, Khang YH, Heon Park J, Kang HJ, Lee H, et al. Data resource profile: the national health information database of the national health insurance service in South Korea. Int J Epidemiol. 2017;46(3):799–800.
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–9.
Simpson RJ Jr, Mendys P. The effects of adherence and persistence on clinical outcomes in patients treated with statins: a systematic review. J Clin Lipidol. 2010;4:462–71.
Chi MD, Vansomphone SS, Liu IL, Cheetham C, Green KR, Scott RD, et al. Adherence to statins and LDL-cholesterol goal attainment. Am J Manag Care. 2014;20(4):e105–12.
Wei L, Wang J, Thompson P, Wong S, Struthers AD, MacDonald TM. Adherence to statin treatment and readmission of patients after myocardial infarction: a six year follow up study. Heart. 2002;88(3):229–33.
Cramer JA, Roy A, Burrell A, Fairchild CJ, Fuldeore MJ, Ollendorf DA, et al. Medication compliance and persistence: terminology and definitions. Value Health. 2008;11(1):44–7.
Choudhry NK, Levin R, Winkelmayer WC. Statins in elderly patients with acute coronary syndrome: an analysis of dose and class effects in typical practice. Heart. 2007;93(8):945–51.
Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, Bhala N, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376(9753):1670–81.
Schuetz CA, van Herick A, Alperin P, Peskin B, Hsia J, Gandhi S. Comparing the effectiveness of rosuvastatin and atorvastatin in preventing cardiovascular outcomes: estimates using the Archimedes model. J Med Econ. 2012;15(6):1118–29.
van Herick A, Schuetz CA, Alperin P, Bullano MF, Balu S, Gandhi S. The impact of initial statin treatment decisions on cardiovascular outcomes in clinical care settings: estimates using the Archimedes Model. Clinicoecon Outcomes Res. 2012;4:337–47.
Folse H, Sternhufvud C, Andy Schuetz C, Rengarajan B, Gandhi S. Impact of switching treatment from rosuvastatin to atorvastatin on rates of cardiovascular events. Clin Ther. 2014;36(1):58–69.
Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366(9493):1267–78.
McKenney JM, Jones PH, Adamczyk MA, Cain VA, Bryzinski BS, Blasetto JW. Comparison of the efficacy of rosuvastatin versus atorvastatin, simvastatin, and pravastatin in achieving lipid goals: results from the STELLAR trial. Curr Med Res Opin. 2003;19(8):689–98.
Stender S, Schuster H, Barter P, Watkins C, Kallend D. Comparison of rosuvastatin with atorvastatin, simvastatin and pravastatin in achieving cholesterol goals and improving plasma lipids in hypercholesterolaemic patients with or without the metabolic syndrome in the MERCURY I trial. Diabetes Obes Metab. 2005;7(4):430–8.
Binbrek AS, Elis A, Al-Zaibag M, Eha J, Keber I, Cuevas AM, et al. Rosuvastatin versus atorvastatin in achieving lipid goals in patients at high risk for cardiovascular disease in clinical practice: a randomized, open-label, parallel-group, multicenter study (DISCOVERY Alpha study). Curr Ther Res Clin Exp. 2006;67(1):21–43.
Insull W Jr, Ghali JK, Hassman DR, Jw YA, Gandhi SK, Miller E. Achieving low-density lipoprotein cholesterol goals in high-risk patients in managed care: comparison of rosuvastatin, atorvastatin, and simvastatin in the SOLAR trial. Mayo Clin Proc. 2007;82(5):543–50.
Park JS, Kim YJ, Choi JY, Kim YN, Hong TJ, Kim DS, et al. Comparative study of low doses of rosuvastatin and atorvastatin on lipid and glycemic control in patients with metabolic syndrome and hypercholesterolemia. Korean J Intern Med. 2010;25(1):27–35.
Harley CR, Gandhi S, Blasetto J, Heien H, Sasane R, Nelson SP. Low-density lipoprotein cholesterol (LDL-C) levels and LDL-C goal attainment among elderly patients treated with rosuvastatin compared with other statins in routine clinical practice. Am J Geriatr Pharmacother. 2007;5(3):185–94.
Khurana S, Gupta S, Bhalla H, Nandwani S, Gupta V. Comparison of anti-inflammatory effect of atorvastatin with rosuvastatin in patients of acute coronary syndrome. J Pharmacol Pharmacother. 2015;6(3):130–5.
Takagi H, Umemoto T. A meta-analysis of randomized head-to-head trials for effects of rosuvastatin versus atorvastatin on apolipoprotein profiles. Am J Cardiol. 2014;113(2):292–301.
Lee CW, Kang SJ, Ahn JM, Song HG, Lee JY, Kim WJ, et al. Comparison of effects of atorvastatin (20 mg) versus rosuvastatin (10 mg) therapy on mild coronary atherosclerotic plaques (from the ARTMAP trial). Am J Cardiol. 2012;109(12):1700–4.
Foody JM, Rathore SS, Galusha D, Masoudi FA, Havranek EP, Radford MJ, et al. Hydroxymethylglutaryl-CoA reductase inhibitors in older persons with acute myocardial infarction: evidence for an age-statin interaction. J Am Geriatr Soc. 2006;54(3):421–30.
Welch HG, Albertsen PC, Nease RF, Bubolz TA, Wasson JH. Estimating treatment benefits for the elderly: the effect of competing risks. Ann Intern Med. 1996;124(6):577–84.
Kronmal RA, Cain KC, Ye Z, Omenn GS. Total serum cholesterol levels and mortality risk as a function of age. A report based on the Framingham data. Arch Intern Med. 1993;153(9):1065–73.
Krumholz HM, Seeman TE, Merrill SS, Mendes de Leon CF, Vaccarino V, Silverman DI, et al. Lack of association between cholesterol and coronary heart disease mortality and morbidity and all-cause mortality in persons older than 70 years. JAMA. 1994;272(17):1335–40.
Ofori-Asenso R, Jakhu A, Zomer E, Curtis AJ, Korhonen MJ, Nelson M, et al. Adherence and persistence among statin users aged 65 years and over: a systematic review and meta-analysis. J Gerontol A Biol Sci Med Sci. 2018;73(6):813–9.
Chowdhury R, Khan H, Heydon E, Shroufi A, Fahimi S, Moore C, et al. Adherence to cardiovascular therapy: a meta-analysis of prevalence and clinical consequences. Eur Heart J. 2013;34(38):2940–8.
Ho PM, Magid DJ, Shetterly SM, Olson KL, Maddox TM, Peterson PN, et al. Medication nonadherence is associated with a broad range of adverse outcomes in patients with coronary artery disease. Am Heart J. 2008;155(4):772–9.
Quinn KL, Macdonald EM, Mamdani MM, Diong C, Juurlink DN, Canadian Drug Safety and Effectiveness Research Network (CDSERN). Lipophilic statins and the risk of intracranial hemorrhage following ischemic stroke: a population-based study. Drug Saf. 2017;40(10):887–93.
Acknowledgements
The authors would like to thank the South Korean National Health Insurance Service for the provision of the claims data from the South Korean National Health Information Database.
Funding
This study was supported by the National Research Foundation, Korea (NRF-2017R1C1B5018232). The funding organization had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflicts of interest
The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kwak, A., Kim, J.H., Choi, C.U. et al. Comparative effectiveness of statins in secondary prevention among the older people aged 75 years and over. Int J Clin Pharm 41, 460–469 (2019). https://doi.org/10.1007/s11096-019-00810-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-019-00810-w